Eating Behavior in Anorexia Nervosa—An Excess of Both Orexigenic and Anorexigenic Signalling? a Inui
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

THE IMPORTANCE of NUTRITION AS the BEST MEDICINE for EATING DISORDERS Carolyn Coker Ross, MD, MPH
DIET AND NUTRITION THE IMPORTANCE OF NUTRITION AS THE BEST MEDICINE FOR EATING DISORDERS Carolyn Coker Ross, MD, MPH ver seven million girls and women groups. Current research demonstrates to 24, and the suicide rate was 75 times and one million boys and men that eating disorder symptoms may be as higher. will suffer from an eating disorder common or more common among certain Medical consequences of eating disor- in their lifetime. Up to 3.7% of ethnic groups (Asians, blacks, and Hispan- ders include arrested sexual maturity and O 6 females will be diagnosed with anorexia ics) when compared with whites. There growth failure in prepubertal patients. nervosa and an estimated 4.2% will have was no difference found in dieting and Many with eating disorders may look and bulimia nervosa.1 The majority of adoles- restraint scores between Asian, Latino, feel deceptively well and may have normal cent patients seen in referral centers fit and white adolescent girls and boys7 and electrograms but are still at high risk for into a third category, “eating disorder not no difference in binging or BED in obese cardiac arrhythmias and sudden death. otherwise specified” or EDNOS and do patients who sought to lose weight with Prolonged amenorrhea is associated with not fit strict criteria for either anorexia or bariatric surgery.8 These changes may be an increased risk of osteopenia and rate of bulimia.2 Nineteen percent of college- related to an extension of cultural ideals in fractures. Neuroimaging studies with com- aged females are bulimic; many go undi- these ethnic populations of what is attrac- puterized tomography (CT) have demon- agnosed until much later. -

Overview of Bariatric Surgery for the Physician
■ CLINICAL PRACTICE Clinical Medicine 2012, Vol 12, No 5: 435–40 Overview of bariatric surgery for the physician Keng Ngee Hng and Yeng S Ang ABSTRACT – The worldwide pandemic of obesity carries effectiveness2,6,15 have fuelled an increase in the number of pro- alarming health and socioeconomic implications. Bariatric cedures performed. surgery is currently the only effective treatment for severe obesity. It is safe, with mortality comparable to that of chole- Types of surgery cystectomy, and effective in producing substantial and sus- tainable weight loss, along with high rates of resolution of Bariatric surgical procedures are traditionally classified as restric- associated comorbidities, including type 2 diabetes. For this tive, malabsorptive or combined according to their mechanism reason, indications for bariatric surgery are being widened. In of action. The procedures most commonly performed are addition to volume restriction and malabsorption, bariatric laparoscopic adjustable gastric banding and roux-en-y gastric surgery brings about neurohormonal changes that affect bypass.3,13 Sleeve gastrectomy is increasingly performed.2,6,7 satiety and glucose homeostasis. Increased understanding of Biliopancreatic diversion and biliopancreatic diversion with these mechanisms will help realise therapeutic benefits by duodenal switch are much more complex and performed infre- pharmacological means. Bariatric surgery improves long-term quently.2,5,17,22 Other historical procedures are no longer in mortality but can cause long-term nutritional deficiencies. common use. The safety of pregnancy after bariatric surgery is still being In addition to restriction and malabsorption, recent evidence elucidated. suggests that neurohormonal changes are an important effect of bariatric surgery.2,6,7,17,18 Bariatric surgery is only part of the KEY WORDS: bariatric surgery, obesity, weight loss, diabetes, management of severe obesity. -

Common Signs and Symptoms of Eating Disorders (Anorexia/Bulimia)
Common Signs and Symptoms of Eating Disorders (Anorexia/Bulimia) 1. Dramatic weight loss in a relatively short period of time. 2. Wearing big or baggy clothes or dressing in layers to hide body and/or weight loss. 3. Obsession with calories and fat content of foods. 4. Obsession with continuous exercise. 5. Frequent trips to the bathroom immediately following meals (sometimes accompanied with water running in the bathroom for a long period of time to hide the sound of vomiting). 6. Visible food restriction and self-starvation. 7. Visible bingeing and/or purging. 8. Use or hiding use of diet pills, laxatives, ipecac syrup (can cause immediate death!) or enemas. 9. Isolation. Fear of eating around and with others. 10. Hiding food in strange places (closets, cabinets, suitcases, under the bed) to avoid eating (Anorexia) or to eat at a later time (Bulimia). 11. Flushing uneaten food down the toilet (can cause sewage problems). 12. Vague or secretive eating patterns. 13. Keeping a "food diary" or lists that consists of food and/or behaviors (ie., purging, restricting, calories consumed, exercise, etc.) 14. Pre-occupation or obsession with food, weight (even if “average” weight or thin), and/or cooking. 15. Visiting websites that promote unhealthy ways to lose weight. 16. Reading books about weight loss and eating disorders. 17. Unusual food rituals: shifting the food around on the plate to look eaten; cutting food into tiny pieces; making sure the fork avoids contact with the lips (using teeth to scrap food off the fork or spoon); chewing food and spitting it out, but not swallowing; dropping food into napkin on lap to later throw away. -

Role of Neuronal Glucosensing in the Regulation of Energy Homeostasis Barry E
Role of Neuronal Glucosensing in the Regulation of Energy Homeostasis Barry E. Levin,1,2 Ling Kang,2 Nicole M. Sanders,3 and Ambrose A. Dunn-Meynell1,2 Glucosensing is a property of specialized neurons in the studies of damage to the hypothalamus pointed to the brain that regulate their membrane potential and firing brain as the primary regulator of energy homeostasis. rate as a function of ambient glucose levels. These neurons Lesions of the ventromedial hypothalamus (VMH) produce have several similarities to - and ␣-cells in the pancreas, increased food intake (hyperphagia), obesity (1), and which are also responsive to ambient glucose levels. Many defective autonomic function in organs involved in the use glucokinase as a rate-limiting step in the production of ATP and its effects on membrane potential and ion channel regulation of energy expenditure (2,3). On the other hand, function to sense glucose. Glucosensing neurons are orga- electrical stimulation of the VMH leads to generalized nized in an interconnected distributed network throughout sympathoadrenal activation (4) with increased activity in the brain that also receives afferent neural input from thermogenic tissues (5). Lesions of the lateral hypotha- glucosensors in the liver, carotid body, and small intes- lamic area (LHA) reduce food intake and increase sympa- tines. In addition to glucose, glucosensing neurons can use thetic activity and eventually establish a new lower other metabolic substrates, hormones, and peptides to defended body weight (3,5,6). Whereas such early studies regulate their firing rate. Consequently, the output of pointed to the hypothalamus as the central controller of these “metabolic sensing” neurons represents their in- tegrated response to all of these simultaneous inputs. -

ICD-10 Mental Health Billable Diagnosis Codes in Alphabetical
ICD-10 Mental Health Billable Diagnosis Codes in Alphabetical Order by Description IICD-10 Mental Health Billable Diagnosis Codes in Alphabetic Order by Description Note: SSIS stores ICD-10 code descriptions up to 100 characters. Actual code description can be longer than 100 characters. ICD-10 Diagnosis Code ICD-10 Diagnosis Description F40.241 Acrophobia F41.0 Panic Disorder (episodic paroxysmal anxiety) F43.0 Acute stress reaction F43.22 Adjustment disorder with anxiety F43.21 Adjustment disorder with depressed mood F43.24 Adjustment disorder with disturbance of conduct F43.23 Adjustment disorder with mixed anxiety and depressed mood F43.25 Adjustment disorder with mixed disturbance of emotions and conduct F43.29 Adjustment disorder with other symptoms F43.20 Adjustment disorder, unspecified F50.82 Avoidant/restrictive food intake disorder F51.02 Adjustment insomnia F98.5 Adult onset fluency disorder F40.01 Agoraphobia with panic disorder F40.02 Agoraphobia without panic disorder F40.00 Agoraphobia, unspecified F10.180 Alcohol abuse with alcohol-induced anxiety disorder F10.14 Alcohol abuse with alcohol-induced mood disorder F10.150 Alcohol abuse with alcohol-induced psychotic disorder with delusions F10.151 Alcohol abuse with alcohol-induced psychotic disorder with hallucinations F10.159 Alcohol abuse with alcohol-induced psychotic disorder, unspecified F10.181 Alcohol abuse with alcohol-induced sexual dysfunction F10.182 Alcohol abuse with alcohol-induced sleep disorder F10.121 Alcohol abuse with intoxication delirium F10.188 Alcohol -
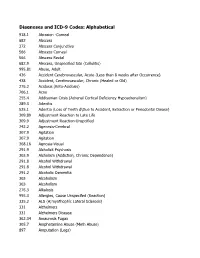
DSM III and ICD 9 Codes 11-2004
Diagnoses and ICD-9 Codes: Alphabetical 918.1 Abrasion -Corneal 682 Abscess 372 Abscess Conjunctiva 566 Abscess Corneal 566 Abscess Rectal 682.9 Abscess, Unspecified Site (Cellulitis) 995.81 Abuse, Adult 436 Accident Cerebrovascular, Acute (Less than 8 weeks after Occurrence) 438 Accident, Cerebrovascular, Chronic (Healed or Old) 276.2 Acidosis (Keto-Acidosis) 706.1 Acne 255.4 Addisonian Crisis (Adrenal Cortical Deficiency Hypoadrenalism) 289.3 Adenitis 525.1 Adentia (Loss of Teeth d\Due to Accident, Extraction or Periodontal Diease) 309.89 Adjustment Reaction to Late Life 309.9 Adjustment Reaction-Unspcified 742.2 Agenesis-Cerebral 307.9 Agitation 307.9 Agitation 368.16 Agnosia-Visual 291.9 Alcholick Psychosis 303.9 Alcholism (Addiction, Chronic Dependence) 291.8 Alcohol Withdrawal 291.8 Alcohol Withdrawal 291.2 Alcoholic Dementia 303 Alcoholism 303 Alcoholism 276.3 Alkalosis 995.3 Allergies, Cause Unspecifed (Reaction) 335.2 ALS (A;myothophic Lateral Sclerosis) 331 Alzheimers 331 Alzheimers Disease 362.34 Amaurosis Fugax 305.7 Amphetamine Abuse (Meth Abuse) 897 Amputation (Legs) 736.89 Amputation, Leg, Status Post (Above Knee, Below Knee) 736.9 Amputee, Site Unspecified (Acquired Deformity) 285.9 Anemia 284.9 Anemia Aplastic (Hypoplastic Bone Morrow) 280 Anemia Due to loss of Blood 281 Anemia Pernicious 280.9 Anemia, Iron Deficiency, Unspecified 285.9 Anemia, Unspecified (Normocytic, Not due to blood loss) 281.9 Anemia, Unspecified Deficiency (Macrocytic, Nutritional 441.5 Aneurysm Aortic, Ruptured 441.1 Aneurysm, Abdominal 441.3 Aneurysm, -

Eating Disorders: About More Than Food
Eating Disorders: About More Than Food Has your urge to eat less or more food spiraled out of control? Are you overly concerned about your outward appearance? If so, you may have an eating disorder. National Institute of Mental Health What are eating disorders? Eating disorders are serious medical illnesses marked by severe disturbances to a person’s eating behaviors. Obsessions with food, body weight, and shape may be signs of an eating disorder. These disorders can affect a person’s physical and mental health; in some cases, they can be life-threatening. But eating disorders can be treated. Learning more about them can help you spot the warning signs and seek treatment early. Remember: Eating disorders are not a lifestyle choice. They are biologically-influenced medical illnesses. Who is at risk for eating disorders? Eating disorders can affect people of all ages, racial/ethnic backgrounds, body weights, and genders. Although eating disorders often appear during the teen years or young adulthood, they may also develop during childhood or later in life (40 years and older). Remember: People with eating disorders may appear healthy, yet be extremely ill. The exact cause of eating disorders is not fully understood, but research suggests a combination of genetic, biological, behavioral, psychological, and social factors can raise a person’s risk. What are the common types of eating disorders? Common eating disorders include anorexia nervosa, bulimia nervosa, and binge-eating disorder. If you or someone you know experiences the symptoms listed below, it could be a sign of an eating disorder—call a health provider right away for help. -

Hypokalaemia in a Woman with Eating Disorder
Grand Rounds Vol 11 pages 53–55 Specialities: Acute Medicine; Nephrology; Psychiatry Article Type: Case Report DOI: 10.1102/1470-5206.2011.0013 ß 2011 e-MED Ltd Hypokalaemia in a woman with eating disorder Zachary Z. Brenera, Boris Medvedovskya, James F. Winchestera and Michael Bergmanb aDivision of Nephrology, Department of Medicine, Beth Israel Medical Center, Albert Einstein School of Medicine of Yeshiva University, New York, USA; bDepartment of Medicine, Campus Golda, Rabin Medical Center, Petah-Tikva, Tel-Aviv University, Israel Corresponding address: Dr Zachary Z. Brener, 350 E. 17th St., Division of Nephrology, Beth Israel Medical Center, New York, NY 10003, USA. Email: [email protected] Date accepted for publication 13 April 2011 Abstract Chronic hypokalaemia often remains a diagnostic challenge, especially in young women without hypertension. A concealed diuretic abuse should be suspected, especially in young women with eating disorders. This case describes a woman with chronic hypokalaemia in whom a thorough medical history and proper laboratory tests were essential to early and accurate diagnosis. Keywords Hypokalaemia; eating disorders; diuretics. Introduction Chronic hypokalaemia often remains a diagnostic challenge, especially in young women without hypertension. After the exclusion of the most obvious causes, a concealed diuretic abuse associated with or without surreptitious vomiting and laxative abuse should be suspected, especially in young women concerned with their body image. A conclusive diagnosis may be difficult as such patients often vigorously deny diuretic intake[1]. Also, only a minority of patients with eating disorders (approximately 6%) abuse diuretics[2–4]. This case describes a woman with chronic hypokalaemia in whom a thorough medical history and proper laboratory tests were essential to an early and accurate diagnosis. -

Section 15: Treatment of Eating Disorders
Formulary and Prescribing Guidelines SECTION 15: TREATMENT OF EATING DISORDERS Section 15. Treatment of eating disorders 15.1 Introduction Please review the Trust document “Guidelines for the assessment and treatment of eating disorders” in the CAMHS Operational Policy. When screening for eating disorders one or two simple questions should be considered for use with specific target groups 1. Do you think you have an eating problem? 2. Do you worry excessively about your weight?’ Early detection may be helped by five screening questions using The SCOFF questionnaire. A score of two or more positive answers should raise clinical suspicion and lead to an in depth diagnostic evaluation. 1. Do you ever make yourself Sick because you feel uncomfortably full? 2. Do you worry you have lost Control over how much you eat? 3. Have you recently lost more than One stone in a three month period? 4. Do you believe yourself to be Fat when others say you are too thin? 5. Would you say that Food dominates your life? It is important to take into account that clients with eating disorders can develop Acute Kidney Injury through a variety of mechanisms associated with each condition. Clinicians should be vigilant in the monitoring of physical health especially serum creatinine and levels of hydration.3 15.2 Anorexia nervosa The following would represent a reasonable initial screen for Anorexia Nervosa in primary care if there are no other indications or diagnostic concerns: Full Blood Count, ESR, Urea and Electrolytes, Creatinine, Liver Function Tests, Random Blood Glucose, Urinalysis, ECG (should be considered in all cases and essential if symptoms/signs of compromised cardiac function, bradycardia, electrolyte abnormality and/or BMI less than 15 kg/m2 or equivalent on centile chart). -

Anorexia/Cachexia Heart Failure Symptom Management Guideline for Adults, Age 19 and Older in British Columbia
Anorexia/Cachexia Heart Failure Symptom Management Guideline For adults, age 19 and older in British Columbia What is anorexia? Anorexia is a syndrome characterized by some or all of the following symptoms: loss of appetite, nausea, early satiety, weakness, fatigue, food aversion, and significant physical and/or psychological symptoms. Causes of anorexia are multifactorial and include fatigue, dyspnea, medication side-effects, nausea, depression, anxiety and sodium restricted diets, which may all be found in patients with heart failure. What is cachexia? Cachexia is a syndrome characterized by severe body weight, fat and muscle loss and increased protein catabolism due to underlying disease. The prevalence of cachexia is 16–42% in the heart failure population and is associated with a 50%, 18 month mortality risk independent of variables such as ejection fraction, age and functional ability. How is cachexia diagnosed? Chronic condition with >5% weight loss in <12 months; or body mass index (BMI) <20kg/m2; and 3 out of 5 additional criteria: 1) Fatigue, 2) Decreased muscle strength, 3) Anorexia, 4) Low muscle mass, 5) Abnormal biochemistry *Blood testing to diagnose cachexia in advanced stages of disease is not advocated. Reminder: Malnutrition also affects prognosis in patients with heart failure and is often found in early transitions of the disease. However this symptom management guideline will focus on the assessment and treatment of anorexia and cachexia. Approach to Managing Anorexia/Cachexia Assessment History: When did weight loss begin? How much weight was lost? Obtain baseline (dry) weight. How is [the patients] appetite? What do they eat or drink on a typical day? How has weight loss affected mood? Ask about: nausea, early satiety, dyspnea, poor oral hygiene, dysphagia, malabsorption, bowel habits. -

Deep Brain Stimulation in Psychiatric Practice
Clinical Memorandum Deep brain stimulation in psychiatric practice March 2018 Authorising Committee/Department: Board Responsible Committee/Department: Section of Electroconvulsive Therapy and Neurostimulation Document Code: CLM PPP Deep brain stimulation in psychiatric practice The Royal Australian and New Zealand College of Psychiatrists (RANZCP) has developed this clinical memorandum to inform psychiatrists who are involved in using DBS as a treatment for psychiatric disorders. Clinical trials into the use of Deep Brain Stimulation (DBS) to treat psychiatric disorders such as depression, obsessive-compulsive disorder, substance use disorders, and anorexia are occurring worldwide, including within Australia. Although overall the existing literature shows promise for DBS in the treatment of psychiatric disorders, its use is still an emerging treatment and requires a stronger clinical evidence base of randomised control trials to develop a substantial body of evidence to identify and support its efficacy (Widge et al., 2016; Barrett, 2017). The RANZCP supports further research and clinical trials into the use of DBS for psychiatric disorders and acknowledges that it has potential application as a treatment for appropriately selected patients. Background DBS is an established treatment for movement disorders such as Parkinson’s disease, tremor and dystonia, and has also been used in the control of movement disorder associated with severe and medically intractable Tourette syndrome (Cannon et al., 2012). In Australia the Therapeutic Goods Administration has approved devices for DBS. It is eligible for reimbursement under the Medicare Benefits Schedule for the treatment of Parkinson’s disease but not for other neurological or psychiatric disorders. As the use of DBS in the treatment of psychiatric disorders is emerging, it is currently only available in speciality clinics or hospitals under research settings. -

Anorexia Nervosa: Current Research from a Biological Perspective
The Science Journal of the Lander College of Arts and Sciences Volume 6 Number 1 Fall 2012 - 1-1-2012 Anorexia Nervosa: Current Research From a Biological Perspective Udy Tropp Touro College Follow this and additional works at: https://touroscholar.touro.edu/sjlcas Part of the Mental Disorders Commons, and the Nutritional and Metabolic Diseases Commons Recommended Citation Tropp, U. (2012). Anorexia Nervosa: Current Research From a Biological Perspective. The Science Journal of the Lander College of Arts and Sciences, 6(1). Retrieved from https://touroscholar.touro.edu/sjlcas/ vol6/iss1/14 This Article is brought to you for free and open access by the Lander College of Arts and Sciences at Touro Scholar. It has been accepted for inclusion in The Science Journal of the Lander College of Arts and Sciences by an authorized editor of Touro Scholar. For more information, please contact [email protected]. 143 ANOREXIA NERVOSA: CURRENT RESEARCH FROM A BIOLOGICAL PERSPECTIVE Udy Tropp ABSTRACT Eating disorders are viewed as serious mental illnesses, carrying significant, life-threatening medical and psychiatric implications, including morbidity and mortality. According to the Academy of Eating Disorders, anorexia nervosa has the highest mortality rate of any psychiatric disorder. The American Psychiatric Association (2004) claims that approximately three percent of the United States female population has a clinically relevant eating disorder. Risk of premature death is 6-12 times higher in women with anorexia as compared to the general population, and it has become the third most common form of chronic illness among adolescent women aged 15 to 19 years. Although the prevalence and seriousness of this problem have gained increasing attention in recent years, relatively little is known about the role that leptin plays in this disorder.