Acute Immune Thrombocytopenic Purpura (ITP) in Childhood
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Transfusion Problems in Hemolytic Anemias*
Transfusion Problems in Hemolytic Anemias* ALI A. HOSSAIN! Department of Pathdlogy, Medical College of Virginia, Richmond 23219 All hemolytic anemias feature shortened red cell Extrinsic Mechanisms survival due to premature hemolysis of the cell. For the Those hemolytic anemias which are due to extrinsic purposes of this presentation, we may classify the factors may be classified, further, as non-immune or hemolytic anemias, most broadly, according to the immune. Non-immune mechanisms include a) drugs mechanisms leading to hemolysis. and chemicals (phenylhydrazine, naphthalene, lead, snake venoms); b) physical agents (heat); c) bacteria Intrinsic Mechanisms and parasites (hemolytic streptococci, Clostridium Hemolytic anemias due to intrinsically defective welchii, Bartonella, plasmodia); and d) acquired sen erythrocytes are essentially of three types. First are sitivity to penicillin, methylodopa, Keftin®, or fava those anemias in which the red cells are defective due plant as examples. Some of the agents in this. last to lack of an essential factor, eg, pernicious anemia group serve to lyse the cells, either through duect in relapse. The second type includes those in which action or by formation of antibodies. the red cells have an abnormal shape because of an These hemolytic anemias due to extrinsic factors inherited error in the chemical makeup of the hemo of the non-immune variety present no transfusion globin molecules; eg, sickle cells, elliptocytes, sphero problem for the Blood Bank. However, it ~~st b.e cytes, and the target -

Thrombotic Thrombocytopenic Purpura and Systemic Lupus Erythematosus: Successful Management of a Rare Presentation
Indian J Crit Care Med July-September 2008 Vol 12 Issue 3 Case Report Thrombotic thrombocytopenic purpura and systemic lupus erythematosus: Successful management of a rare presentation Pratish George, Jasmine Das, Basant Pawar1, Naveen Kakkar2 Thrombotic thrombocytopenic purpura (TTP) and systemic lupus erythematosus (SLE) very rarely present simultaneously and pose a diagnostic and therapeutic dilemma to the critical care team. Prompt diagnosis and management with plasma exchange and immunosuppression is life-saving. A patient critically ill with TTP and SLE, successfully managed in the acute period of illness with plasma exchange, steroids and Abstract mycophenolate mofetil is described. Key words: Plasma exchange, systemic lupus erythematosus, thrombotic thrombocytopenic purpura Introduction Case Report Systemic lupus erythematosis (SLE) is diagnosed by A 30-year-old lady was admitted with fever and the presence of four or more of the following criteria, jaundice. A week earlier she had undergone an serially or simultaneously: malar rash, discoid rash, uncomplicated medical termination of pregnancy at photosensitivity, oral ulcers, non erosive arthritis, serositis, another hospital, at 13 weeks of gestation. She had an renal abnormalities including proteinuria or active urinary uneventful pregnancy with twins two years earlier and sediments, neuropsychiatric features, hematological the twins were diagnosed to have thalassemia major. abnormalities including hemolytic anemia, leucopenia, She was subsequently diagnosed to have thalassemia lymphopenia and thrombocytopenia, immunological minor and her husband had thalassemia minor trait. No markers like anti-ds DNA or anti-Smith antibody and high earlier history of spontaneous Þ rst trimester abortions Antinuclear antibody titres. Thrombotic thrombocytopenic was present. purpura (TTP) in patients with SLE is extremely rare. -

Hemolytic Disease of the Newborn
Intensive Care Nursery House Staff Manual Hemolytic Disease of the Newborn INTRODUCTION and DEFINITION: Hemolytic Disease of the Newborn (HDN), also known as erythroblastosis fetalis, isoimmunization, or blood group incompatibility, occurs when fetal red blood cells (RBCs), which possess an antigen that the mother lacks, cross the placenta into the maternal circulation, where they stimulate antibody production. The antibodies return to the fetal circulation and result in RBC destruction. DIFFERENTIAL DIAGNOSIS of hemolytic anemia in a newborn infant: -Isoimmunization -RBC enzyme disorders (e.g., G6PD, pyruvate kinase deficiency) -Hemoglobin synthesis disorders (e.g., alpha-thalassemias) -RBC membrane abnormalities (e.g., hereditary spherocytosis, elliptocytosis) -Hemangiomas (Kasabach Merritt syndrome) -Acquired conditions, such as sepsis, infections with TORCH or Parvovirus B19 (anemia due to RBC aplasia) and hemolysis secondary to drugs. ISOIMMUNIZATION A. Rh disease (Rh = Rhesus factor) (1) Genetics: Rh positive (+) denotes presence of D antigen. The number of antigenic sites on RBCs varies with genotype. Prevalence of genotype varies with the population. Rh negative (d/d) individuals comprise 15% of Caucasians, 5.5% of African Americans, and <1% of Asians. A sensitized Rh negative mother produces anti-Rh IgG antibodies that cross the placenta. Risk factors for antibody production include 2nd (or later) pregnancies*, maternal toxemia, paternal zygosity (D/D rather than D/d), feto-maternal compatibility in ABO system and antigen load. (2) Clinical presentation of HDN varies from mild jaundice and anemia to hydrops fetalis (with ascites, pleural and pericardial effusions). Because the placenta clears bilirubin, the chief risk to the fetus is anemia. Extramedullary hematopoiesis (due to anemia) results in hepatosplenomegaly. -

A Newly Recognized Blood Group in Domestic Shorthair Cats: the Mik Red Cell Antigen
J Vet Intern Med 2007;21:287–292 A Newly Recognized Blood Group in Domestic Shorthair Cats: The Mik Red Cell Antigen Nicole M. Weinstein, Marie-Claude Blais, Kimberly Harris, Donna A. Oakley, Lillian R. Aronson, and Urs Giger Background: Naturally occurring alloantibodies produced against A and B red cell antigens in cats can cause acute hemolytic transfusion reactions. Blood incompatibilities, unrelated to the AB blood group system, have also been suspected after blood transfusions through routine crossmatch testing or as a result of hemolytic transfusion reactions. Hypothesis: Incompatible crossmatch results among AB compatible cats signify the presence of a naturally occurring alloantibody against a newly identified blood antigen in a group of previously never transfused blood donor cats. The associated alloantibody is clinically important based upon a hemolytic transfusion reaction after inadvertent transfusion of red cells expressing this red cell antigen in a feline renal transplant recipient that lacks this red cell antigen. Methods: Blood donor and nonblood donor cats were evaluated for the presence of auto- and alloantibodies using direct antiglobulin and crossmatch tests, respectively, and were blood typed for AB blood group status. Both standard tube and novel gel column techniques were used. Results: Plasma from 3 of 65 cats and 1 feline renal transplant recipient caused incompatible crossmatch test results with AB compatible erythrocytes indicating these cats formed an alloantibody against a red cell antigen they lack, termed Mik. The 3 donors and the renal transplant recipient were crossmatch-compatible with one another. Tube and gel column crossmatch test results were similar. Conclusions and Clinical Importance: The absence of this novel Mik red cell antigen can be associated with naturally occurring anti-Mik alloantibodies and can elicit an acute hemolytic transfusion reaction after an AB-matched blood transfusion. -

Urticarial Vasculitis Associated with Essential Thrombocythaemia
Acta Derm Venereol 2014; 94: 244–245 SHORT COMMUNICATION Urticarial Vasculitis Associated with Essential Thrombocythaemia Annabel D. Scott, Nicholas Francis, Helen Yarranton and Sarita Singh Dermatology Registrar, Department of Dermatology, Chelsea and Westminster Hospital, 369 Fulham Road, London SW10 9NH, United Kingdom. E-mail: [email protected] Accepted Apr 3, 2013; Epub ahead of print Aug 27, 2013 Urticarial vasculitis is a form of leucocytoclastic vas- prednisolone 30 mg once daily, which controlled her culitis whereby the skin lesions resemble urticaria. It is symptoms. associated with systemic lupus erythematosus, Sjögren’s A biopsy was taken from an uticarial lesion on the syndrome, hepatitis B and C viruses (1). Rarely it is asso- arm. Histology showed numerous perivascular neutro- ciated with an underlying haematological disorders and, phils and eosinophils with margination of neutrophils to the best of our knowledge, has never been reported in in the lumen of vessels and some leucocytoclasis with association with essential thrombocythaemia. We present red cell extravasation in keeping with an urticarial a case report of urticarial vasculitis associated with es- vasculitis (Fig. 2). sential thrombocythaemia. Blood tests revealed an erythrocyte sedimentation rate of 47 mm/h (normal range 1–12), a platelet count of 1,098 × 109/l (normal range 135–400) and an eosi- CASE REPORT nophilia of 1.0 × 109/l (normal range 0–0.2). Comple- A 32-year-old woman presented with a several month ment levels, thyroid function, serum iron, haemoglobin, history of recurrent urticaria without angioedema, 4 C-reactive protein, anti-nuclear antibody, anti-nuclear months post-partum. -

081999 Disseminated Intravascular Coagulation
The New England Journal of Medicine Current Concepts Systemic activation+ of coagulation DISSEMINATED INTRAVASCULAR COAGULATION Intravascular+ Depletion of platelets+ deposition of fibrin and coagulation factors MARCEL LEVI, M.D., AND HUGO TEN CATE, M.D. Thrombosis of small+ Bleeding and midsize vessels+ ISSEMINATED intravascular coagulation is and organ failure characterized by the widespread activation Dof coagulation, which results in the intravas- Figure 1. The Mechanism of Disseminated Intravascular Coag- cular formation of fibrin and ultimately thrombotic ulation. occlusion of small and midsize vessels.1-3 Intravascu- Systemic activation of coagulation leads to widespread intra- lar coagulation can also compromise the blood sup- vascular deposition of fibrin and depletion of platelets and co- agulation factors. As a result, thrombosis of small and midsize ply to organs and, in conjunction with hemodynam- vessels may occur, contributing to organ failure, and there may ic and metabolic derangements, may contribute to be severe bleeding. the failure of multiple organs. At the same time, the use and subsequent depletion of platelets and coag- ulation proteins resulting from the ongoing coagu- lation may induce severe bleeding (Fig. 1). Bleeding may be the presenting symptom in a patient with disseminated intravascular coagulation, a factor that can complicate decisions about treatment. TABLE 1. COMMON CLINICAL CONDITIONS ASSOCIATED WITH DISSEMINATED ASSOCIATED CLINICAL CONDITIONS INTRAVASCULAR COAGULATION. AND INCIDENCE Sepsis Infectious Disease Trauma Serious tissue injury Disseminated intravascular coagulation is an ac- Head injury Fat embolism quired disorder that occurs in a wide variety of clin- Cancer ical conditions, the most important of which are listed Myeloproliferative diseases in Table 1. -

What Everyone Should Know to Stop Bleeding After an Injury
What Everyone Should Know to Stop Bleeding After an Injury THE HARTFORD CONSENSUS The Joint Committee to Increase Survival from Active Shooter and Intentional Mass Casualty Events was convened by the American College of Surgeons in response to the growing number and severity of these events. The committee met in Hartford Connecticut and has produced a number of documents with rec- ommendations. The documents represent the consensus opinion of a multi-dis- ciplinary committee involving medical groups, the military, the National Security Council, Homeland Security, the FBI, law enforcement, fire rescue, and EMS. These recommendations have become known as the Hartford Consensus. The overarching principle of the Hartford Consensus is that no one should die from uncontrolled bleeding. The Hartford Consensus recommends that all citizens learn to stop bleeding. Further information about the Hartford Consensus and bleeding control can be found on the website: Bleedingcontrol.org 2 SAVE A LIFE: What Everyone Should Know to Stop Bleeding After an Injury Authors: Peter T. Pons, MD, FACEP Lenworth Jacobs, MD, MPH, FACS Acknowledgements: The authors acknowledge the contributions of Michael Cohen and James “Brooks” Hart, CMI to the design of this manual. Some images adapted from Adam Wehrle, EMT-P and NAEMT. © 2017 American College of Surgeons CONTENTS SECTION 1 3 ■ Introduction ■ Primary Principles of Trauma Care Response ■ The ABCs of Bleeding SECTION 2 5 ■ Ensure Your Own Safety SECTION 3 6 ■ A – Alert – call 9-1-1 SECTION 4 7 ■ B – Bleeding – find the bleeding injury SECTION 5 9 ■ C – Compress – apply pressure to stop the bleeding by: ■ Covering the wound with a clean cloth and applying pressure by pushing directly on it with both hands, OR ■Using a tourniquet, OR ■ Packing (stuff) the wound with gauze or a clean cloth and then applying pressure with both hands SECTION 6 13 ■ Summary 2 SECTION 1: INTRODUCTION Welcome to the Stop the Bleed: Bleeding Control for the Injured information booklet. -

Blood Bank I D
The Osler Institute Blood Bank I D. Joe Chaffin, MD Bonfils Blood Center, Denver, CO The Fun Just Never Ends… A. Blood Bank I • Blood Groups B. Blood Bank II • Blood Donation and Autologous Blood • Pretransfusion Testing C. Blood Bank III • Component Therapy D. Blood Bank IV • Transfusion Complications * Noninfectious (Transfusion Reactions) * Infectious (Transfusion-transmitted Diseases) E. Blood Bank V (not discussed today but available at www.bbguy.org) • Hematopoietic Progenitor Cell Transplantation F. Blood Bank Practical • Management of specific clinical situations • Calculations, Antibody ID and no-pressure sample questions Blood Bank I Blood Groups I. Basic Antigen-Antibody Testing A. Basic Red Cell-Antibody Interactions 1. Agglutination a. Clumping of red cells due to antibody coating b. Main reaction we look for in Blood Banking c. Two stages: 1) Coating of cells (“sensitization”) a) Affected by antibody specificity, electrostatic RBC charge, temperature, amounts of antigen and antibody b) Low Ionic Strength Saline (LISS) decreases repulsive charges between RBCs; tends to enhance cold antibodies and autoantibodies c) Polyethylene glycol (PEG) excludes H2O, tends to enhance warm antibodies and autoantibodies. 2) Formation of bridges a) Lattice structure formed by antibodies and RBCs b) IgG isn’t good at this; one antibody arm must attach to one cell and other arm to the other cell. c) IgM is better because of its pentameric structure. P}Chaffin (12/28/11) Blood Bank I page 1 Pathology Review Course 2. Hemolysis a. Direct lysis of a red cell due to antibody coating b. Uncommon, but equal to agglutination. 1) Requires complement fixation 2) IgM antibodies do this better than IgG. -

Immune-Pathophysiology and -Therapy of Childhood Purpura
Egypt J Pediatr Allergy Immunol 2009;7(1):3-13. Review article Immune-pathophysiology and -therapy of childhood purpura Safinaz A Elhabashy Professor of Pediatrics, Ain Shams University, Cairo Childhood purpura - Overview vasculitic disorders present with palpable Purpura (from the Latin, purpura, meaning purpura2. Purpura may be secondary to "purple") is the appearance of red or purple thrombocytopenia, platelet dysfunction, discolorations on the skin that do not blanch on coagulation factor deficiency or vascular defect as applying pressure. They are caused by bleeding shown in table 1. underneath the skin. Purpura measure 0.3-1cm, A thorough history (Table 2) and a careful while petechiae measure less than 3mm and physical examination (Table 3) are critical first ecchymoses greater than 1cm1. The integrity of steps in the evaluation of children with purpura3. the vascular system depends on three interacting When the history and physical examination elements: platelets, plasma coagulation factors suggest the presence of a bleeding disorder, and blood vessels. All three elements are required laboratory screening studies may include a for proper hemostasis, but the pattern of bleeding complete blood count, peripheral blood smear, depends to some extent on the specific defect. In prothrombin time (PT) and activated partial general, platelet disorders manifest petechiae, thromboplastin time (aPTT). With few exceptions, mucosal bleeding (wet purpura) or, rarely, central these studies should identify most hemostatic nervous system bleeding; -
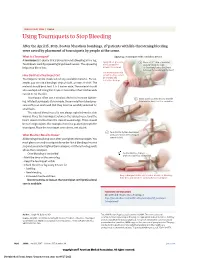
Using Tourniquets to Stop Bleeding
JAMA PATIENT PAGE | Trauma Using Tourniquets to Stop Bleeding After the April 15, 2013, Boston Marathon bombings, 27 patients with life-threatening bleeding were saved by placement of tourniquets by people at the scene. What Is a Tourniquet? Applying a tourniquet with a windlass device A tourniquet is a device that is placed around a bleeding arm or leg. Apply direct pressure 1 Place a 2-3” strip of material Tourniquets work by squeezing large blood vessels. The squeezing to the wound for about 2” from the edge helps stop blood loss. at least 15 minutes. of the wound over a long bone between the wound and the heart. Use a tourniquet only How Do I Put a Tourniquet On? when bleeding cannot be stopped and Tourniquets can be made out of any available material. For ex- is life threatening. ample, you can use a bandage, strip of cloth, or even a t-shirt. The material should be at least 2 to 3 inches wide. The material should also overlap itself. Using thin straps or material less than 2 inches wide can rip or cut the skin. Tourniquets often use a windlass device to increase tighten- 2 Insert a stick or other strong, straight ing. Inflated tourniquets (for example, those made from blood pres- item into the knot to act as a windlass. sure cuffs) can work well. But they must be carefully watched for small leaks. The injured blood vessel is not always right below the skin wound. Place the tourniquet between the injured vessel and the heart, about 2 inches from the closest wound edge. -

A Guide for People Living with Von Willebrand Disorder CONTENTS
A guide for people living with von Willebrand disorder CONTENTS What is von Willebrand disorder (VWD)?................................... 3 Symptoms............................................................................................... 5 Types of VWD...................................................................................... 6 How do you get VWD?...................................................................... 7 VWD and blood clotting.................................................................... 11 Diagnosis................................................................................................. 13 Treatment............................................................................................... 15 Taking care of yourself or your child.............................................. 19 (Education, information, first aid/medical emergencies, medication to avoid) Living well with VWD......................................................................... 26 (Sport, travel, school, telling others, work) Special issues for women and girls.................................................. 33 Connecting with others..................................................................... 36 Can I live a normal life with von Willebrand disorder?............. 37 More information................................................................................. 38 2 WHAT IS VON WILLEBRAND DISORDER (VWD)? Von Willebrand disorder (VWD) is an inherited bleeding disorder. People with VWD have a problem with a protein -

Autoimmune Hemolytic Anemia in COVID-19 Patients, the « Transmissible » Direct Coombs Test
J H C R JOURNAL OF HEMATOLOGY 2640-2823 AND CLINICAL RESEARCH Research Article More Information *Address for Correspondence: Alice Brochier, Hematology Department of Laboratory Medicine, Autoimmune hemolytic anemia in Saint-Luc University Hospital, Avenue Hippocrate 10, 1200 Brussels, Belgium, Tel: +322764 6814; COVID-19 patients, the « transmissible » Email: [email protected]; Véronique Deneys, Hematology Department of Laboratory Medicine, Saint-Luc University direct Coombs test Hospital, Avenue Hippocrate 10, 1200 Brussels, Belgium, Email: [email protected] Alice Brochier1*, Julien Cabo1, Claudine Guerrieri1, Leïla Belkhir2, Submitted: March 24, 2021 3 1 Pierre-François Laterre and Véronique Deneys * Approved: April 06, 2021 Published: April 07, 2021 1Hematology Department of Laboratory Medicine, Saint-Luc University Hospital, Brussels, Belgium 2Department of Internal Medicine and Infectious Diseases, Saint-Luc University Hospital, Brussels, How to cite this article: Brochier A, Cabo J, Guerrieri C, Belkhir L, Laterre PF, Deneys V. Belgium Autoimmune hemolytic anemia in COVID-19 3 Department of Intensive Care Medicine, Saint-Luc University Hospital, Brussels, Belgium patients, the « transmissible » direct Coombs test. J Hematol Clin Res. 2021; 5: 004-008. Abstract DOI: 10.29328/journal.jhcr.1001016 Copyright: © 2021 Brochier A, et al. This Background: Like other viruses, the SARS-CoV-2 (severe acute respiratory syndrome is an open access article distributed under coronavirus 2) appears to be responsible for several autoimmune complications. The occurrence the Creative Commons Attribution License, of autoimmune hemolytic anemia has been described in several case reports. This AIHA was also which permits unrestricted use, distribution, noticeable by the important number of blood transfusions required for COVID-19 (coronavirus and reproduction in any medium, provided the disease 2019) patients.