A Saudi Child with Chronic Immune Thrombocytopenia and Vitiligo
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D
Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D. Director of Ethnic Skin Care Voluntary Assistant Professor Miller/University of Miami School of Medicine Department of Dermatology and Cutaneous Surgery What Determines Skin Color? What Determines Skin Color? No significant difference in the number of melanocytes between the races 2000 epidermal melanocytes/mm2 on head and forearm 1000 epidermal melanocytes/mm2 on the rest of the body differences present at birth Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff,K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192-220, New York, NY: McGraw Hill Melanosomes in Black and White Skin Black White Szabo G, Gerald AB, Pathak MA, Fitzpatrick TB. Nature1969;222:1081-1082 Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff, K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192- 220, New York, NY: McGraw Hill Role of Melanin-Advantages Melanin absorbs and scatters energy from UV and visible light to protect epidermal cells from UV damage Disadvantages Inflammation or injury to the skin is almost immediately accompanied by alteration in pigmentation Hyperpigmentation Hypopigmentation Dyschromias Post-Inflammatory hyperpigmentation Acne Melasma Lichen Planus Pigmentosus Progressive Macular Hypomelanosis -

Thrombotic Thrombocytopenic Purpura and Systemic Lupus Erythematosus: Successful Management of a Rare Presentation
Indian J Crit Care Med July-September 2008 Vol 12 Issue 3 Case Report Thrombotic thrombocytopenic purpura and systemic lupus erythematosus: Successful management of a rare presentation Pratish George, Jasmine Das, Basant Pawar1, Naveen Kakkar2 Thrombotic thrombocytopenic purpura (TTP) and systemic lupus erythematosus (SLE) very rarely present simultaneously and pose a diagnostic and therapeutic dilemma to the critical care team. Prompt diagnosis and management with plasma exchange and immunosuppression is life-saving. A patient critically ill with TTP and SLE, successfully managed in the acute period of illness with plasma exchange, steroids and Abstract mycophenolate mofetil is described. Key words: Plasma exchange, systemic lupus erythematosus, thrombotic thrombocytopenic purpura Introduction Case Report Systemic lupus erythematosis (SLE) is diagnosed by A 30-year-old lady was admitted with fever and the presence of four or more of the following criteria, jaundice. A week earlier she had undergone an serially or simultaneously: malar rash, discoid rash, uncomplicated medical termination of pregnancy at photosensitivity, oral ulcers, non erosive arthritis, serositis, another hospital, at 13 weeks of gestation. She had an renal abnormalities including proteinuria or active urinary uneventful pregnancy with twins two years earlier and sediments, neuropsychiatric features, hematological the twins were diagnosed to have thalassemia major. abnormalities including hemolytic anemia, leucopenia, She was subsequently diagnosed to have thalassemia lymphopenia and thrombocytopenia, immunological minor and her husband had thalassemia minor trait. No markers like anti-ds DNA or anti-Smith antibody and high earlier history of spontaneous Þ rst trimester abortions Antinuclear antibody titres. Thrombotic thrombocytopenic was present. purpura (TTP) in patients with SLE is extremely rare. -

Frequency of Different Types of Facial Melanoses Referring to the Department of Dermatology and Venereology, Nepal Medical Colle
Amatya et al. BMC Dermatology (2020) 20:4 https://doi.org/10.1186/s12895-020-00100-3 RESEARCH ARTICLE Open Access Frequency of different types of facial melanoses referring to the Department of Dermatology and Venereology, Nepal Medical College and Teaching Hospital in 2019, and assessment of their effect on health-related quality of life Bibush Amatya* , Anil Kumar Jha and Shristi Shrestha Abstract Background: Abnormalities of facial pigmentation, or facial melanoses, are a common presenting complaint in Nepal and are the result of a diverse range of conditions. Objectives: The objective of this study was to determine the frequency, underlying cause and impact on quality of life of facial pigmentary disorders among patients visiting the Department of Dermatology and Venereology, Nepal Medical College and Teaching Hospital (NMCTH) over the course of one year. Methods: This was a cross-sectional study conducted at the Department of Dermatology and Venereology, NMCT H. We recruited patients with facial melanoses above 16 years of age who presented to the outpatient department. Clinical and demographic data were collected and all the enrolled participants completed the validated Nepali version of the Dermatology Life Quality Index (DLQI). Results: Between January 5, 2019 to January 4, 2020, a total of 485 patients were recruited in the study. The most common diagnoses were melasma (166 patients) and post acne hyperpigmentation (71 patients). Quality of life impairment was highest in patients having melasma with steroid induced rosacea-like dermatitis (DLQI = 13.54 ± 1.30), while it was lowest in participants with ephelides (2.45 ± 1.23). Conclusion: Facial melanoses are a common presenting complaint and lead to substantial impacts on quality of life. -

In Dermatology Visit with Me to Discuss
From time to time new treatments surface for any medical field, and the last couple of years have seen new treatments emerge, or new applications for familiar treatments. I wanted to summarize some of these New Therapies widely available remedies and encourage you to schedule a in Dermatology visit with me to discuss. Written by Board Certified Dermatologist James W. Young, DO, FAOCD Nicotinamide a significant reduction in melanoma in Antioxidants Nicotinamide (niacinamide) is a form high risk skin cancer patients at doses Green tea, pomegranate, delphinidin of vitamin B3. The deficiency of vitamin more than 600 and less than 4,000 IU and fisetin are all under current study for daily. B3 causes pellagra, a condition marked either oral or topical use in the reduction by 4D’s – (photo) Dermatitis, Dementia, Polypodium Leucotomos of the incidence of skin cancer, psoriasis Diarrhea and (if left untreated) Death. and other inflammatory disorders. I’ll be Polypodium leucotomos is a Central This deficiency is rare in developed sure to keep patients updated. countries, but is occasionally seen America fern that is available in several in alcoholism, dieting restrictions, or forms, most widely as Fernblock What Are My Own Thoughts? malabsorption syndromes. Nicotinamide (Amazon) or Heliocare (Walgreen’s and I take Vitamin D 1,000 IU and Heliocare does not cause the adverse effects of Amazon) and others. It is an antioxidant personally. Based on new research, I Nicotinic acid and is safe at doses up to that reduces free oxygen radicals and have also added Nicotinamide which 3,000mg daily. may reduce inflammation in eczema, dementia, sunburn, psoriasis, and vitiligo. -

Psoriasis and Vitiligo: an Association Or Coincidence?
igmentar f P y D l o is a o n r r d e u r o s J Solovan C, et al., Pigmentary Disorders 2014, 1:1 Journal of Pigmentary Disorders DOI: 10.4172/jpd.1000106 World Health Academy ISSN: 2376-0427 Letter To Editor Open Access Psoriasis and Vitiligo: An Association or Coincidence? Caius Solovan1, Anca E Chiriac2, Tudor Pinteala2, Liliana Foia2 and Anca Chiriac3* 1University of Medicine and Pharmacy “V Babes” Timisoara, Romania 2University of Medicine and Pharmacy “Gr T Popa” Iasi, Romania 3Apollonia University, Nicolina Medical Center, Iasi, Romania *Corresponding author: Anca Chiriac, Apollonia University, Nicolina Medical Center, Iasi, Romania, Tel: 00-40-721-234-999; E-mail: [email protected] Rec date: April 21, 2014; Acc date: May 23, 2014; Pub date: May 25, 2014 Citation: Solovan C, Chiriac AE, Pinteala T, Foia L, Chiriac A (2014) Psoriasis and Vitiligo: An Association or Coincidence? Pigmentary Disorders 1: 106. doi: 10.4172/ jpd.1000106 Copyright: © 2014 Solovan C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Letter to Editor Dermatitis herpetiformis 1 0.08% Sir, Chronic urticaria 2 0.16% The worldwide occurrence of psoriasis in the general population is Lyell syndrome 1 0.08% about 2–3% and of vitiligo is 0.5-1%. Coexistence of these diseases in the same patient is rarely reported and based on a pathogenesis not Quincke edema 1 0.08% completely understood [1]. -

Pityriasis Alba Revisited: Perspectives on an Enigmatic Disorder of Childhood
Pediatric ddermatologyermatology Series Editor: Camila K. Janniger, MD Pityriasis Alba Revisited: Perspectives on an Enigmatic Disorder of Childhood Yuri T. Jadotte, MD; Camila K. Janniger, MD Pityriasis alba (PA) is a localized hypopigmented 80 years ago.2 Mainly seen in the pediatric popula- disorder of childhood with many existing clinical tion, it primarily affects the head and neck region, variants. It is more often detected in individuals with the face being the most commonly involved with a darker complexion but may occur in indi- site.1-3 Pityriasis alba is present in individuals with viduals of all skin types. Atopy, xerosis, and min- all skin types, though it is more noticeable in those with eral deficiencies are potential risk factors. Sun a darker complexion.1,3 This condition also is known exposure exacerbates the contrast between nor- as furfuraceous impetigo, erythema streptogenes, mal and lesional skin, making lesions more visible and pityriasis streptogenes.1 The term pityriasis alba and patients more likely to seek medical atten- remains accurate and appropriate given the etiologic tion. Poor cutaneous hydration appears to be a elusiveness of the disorder. common theme for most riskCUTIS factors and may help elucidate the pathogenesis of this disorder. The Epidemiology end result of this mechanism is inappropriate mel- Pityriasis alba primarily affects preadolescent children anosis manifesting as hypopigmentation. It must aged 3 to 16 years,4 with onset typically occurring be differentiated from other disorders of hypopig- between 6 and 12 years of age.5 Most patients are mentation, such as pityriasis versicolor alba, vitiligo, younger than 15 years,3 with up to 90% aged 6 to nevus depigmentosus, and nevus anemicus. -

Immune-Pathophysiology and -Therapy of Childhood Purpura
Egypt J Pediatr Allergy Immunol 2009;7(1):3-13. Review article Immune-pathophysiology and -therapy of childhood purpura Safinaz A Elhabashy Professor of Pediatrics, Ain Shams University, Cairo Childhood purpura - Overview vasculitic disorders present with palpable Purpura (from the Latin, purpura, meaning purpura2. Purpura may be secondary to "purple") is the appearance of red or purple thrombocytopenia, platelet dysfunction, discolorations on the skin that do not blanch on coagulation factor deficiency or vascular defect as applying pressure. They are caused by bleeding shown in table 1. underneath the skin. Purpura measure 0.3-1cm, A thorough history (Table 2) and a careful while petechiae measure less than 3mm and physical examination (Table 3) are critical first ecchymoses greater than 1cm1. The integrity of steps in the evaluation of children with purpura3. the vascular system depends on three interacting When the history and physical examination elements: platelets, plasma coagulation factors suggest the presence of a bleeding disorder, and blood vessels. All three elements are required laboratory screening studies may include a for proper hemostasis, but the pattern of bleeding complete blood count, peripheral blood smear, depends to some extent on the specific defect. In prothrombin time (PT) and activated partial general, platelet disorders manifest petechiae, thromboplastin time (aPTT). With few exceptions, mucosal bleeding (wet purpura) or, rarely, central these studies should identify most hemostatic nervous system bleeding; -
Alopecia Areata, Atopic Dermatitis and Vitiligo (Global) Competitive Grant Program - Internal Pfizer Review Process
Pfizer Announces a Research Grant RFP Alopecia Areata, Atopic Dermatitis and Vitiligo (Global) Competitive Grant Program - internal Pfizer review process I. Background Pfizer Global Medical Grants (GMG) supports the global healthcare community’s independent initiatives (e.g., research, quality improvement, or education) to improve patient outcomes in areas of unmet medical need that are aligned with Pfizer’s medical and/or scientific strategies. Pfizer’s GMG competitive grant program involves a publicly posted general Request for Proposal (RFP) that provides detail regarding a general area of interest, sets timelines for review and approval, and uses an internal Pfizer review process to make final grant decisions. Organizations are invited to submit an application addressing the research gaps as outlined in the specific RFP. For all Investigator Sponsored Research (ISRs) and general research grants, the grant requester (and ultimately the grantee) is responsible for the design, implementation, sponsorship, and conduct of the independent initiative supported by the grant, including compliance with any regulatory requirements. Pfizer must not be involved in any aspect of study protocol or project development, nor the conduct or monitoring of the research program. Alopecia3 Areata, Atopic Dermatitis and Vitiligo (Global) II. Eligibility Geographic Scope: Global (including U.S.A.) Applicant Eligibility • Only organizations are eligible to receive grants, not individuals or Criteria medical practice groups. • The applicant (PI) must have a -
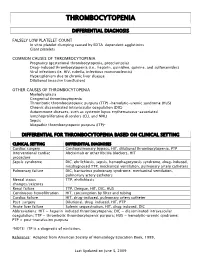
Thrombocytopenia.Pdf
THROMBOCYTOPENIA DIFFERENTIAL DIAGNOSIS FALSELY LOW PLATELET COUNT In vitro platelet clumping caused by EDTA-dependent agglutinins Giant platelets COMMON CAUSES OF THROMBOCYTOPENIA Pregnancy (gestational thrombocytopenia, preeclampsia) Drug-induced thrombocytopenia (i.e., heparin, quinidine, quinine, and sulfonamides) Viral infections (ie. HIV, rubella, infectious mononucleosis) Hypersplenism due to chronic liver disease Dilutional (massive transfusion) OTHER CAUSES OF THROMBOCYTOPENIA Myelodysplasia Congenital thrombocytopenia Thrombotic thrombocytopenic purpura (TTP) -hemolytic-uremic syndrome (HUS) Chronic disseminated intravascular coagulation (DIC) Autoimmune diseases, such as systemic lupus erythematosus-associated lymphoproliferative disorders (CLL and NHL) Sepsis Idiopathic thrombocytopenic purpura (ITP)* DIFFERENTIAL FOR THROMBOCYTOPENIA BASED ON CLINICAL SETTING CLINICAL SETTING DIFFERENTIAL DIAGNOSES Cardiac surgery Cardiopulmonary bypass, HIT, dilutional thrombocytopenia, PTP Interventional cardiac Abciximab or other IIb/IIIa blockers, HIT procedure Sepsis syndrome DIC, ehrlichiosis, sepsis, hemophagocytosis syndrome, drug-induced, misdiagnosed TTP, mechanical ventilation, pulmonary artery catheters Pulmonary failure DIC, hantavirus pulmonary syndrome, mechanical ventilation, pulmonary artery catheters Mental status TTP, ehrlichiosis changes/seizures Renal failure TTP, Dengue, HIT, DIC, HUS Continuous hemofiltration HIT, consumption by filter and tubing Cardiac failure HIT, drug-induced, pulmonary artery catheter Post-surgery -

Pathobiology of Thrombocytopenia and Bleeding in Patients with Wiskott-Aldrich Syndrome
TITLE: Pathobiology of Thrombocytopenia and Bleeding in Patients with Wiskott-Aldrich Syndrome Principal Investigator: James B. Bussel, MD IRB Protocol Number: 0801009600 ClinicalTrials.gov ID: NCT00909363 Compound Number: SB-497115 Development Phase: Phase II Effective Date: August 26th 2010 Updated: September 18, 2015 Protocol Versions: August 15, 2013 October 28, 2014 December 31, 2014 July 7, 2015 1 TABLE OF CONTENTS List of Abbreviations 4 1 INTRODUCTION 5 1.1 Background 5 1.2 Rationale 5 2 OBJECTIVE(S) 6 2.1 Primary Objective 6 2.2 Secondary Objectives 6 3 INVESTIGATIONAL PLAN 6 3.1 Study Design 6 3.2 Laboratory Testing 7 4 SUBJECT SELECTION AND WITHDRAWAL CRITERIA 8 4.1 Number of Subjects 8 4.2 Inclusion Criteria 8 4.3 Exclusion Criteria 8 4.4 Withdrawal Criteria 9 4.4.1 Study Stopping Rules 10 4.4.2 Patient Stopping Rules 10 5 STUDY TREATMENTS 10 5.1 Treatment Assignment 10 5.2 Product Accountability 11 5.3 Treatment Compliance 11 5.4 Concomitant Medications and Non-Drug Therapies 11 5.4.1 Permitted Medications and Non-Drug Therapies 11 5.4.2 Prohibited Medications and Non-Drug Therapies 11 5.5 Treatment after the End of the Study 11 5.6 Treatment of Investigational Product Overdose 11 5.7 Treatment Plan 12 6 STUDY ASSESSMENTS AND PROCEDURES 13 6.1 Critical Baseline Assessments 13 6.2 Efficacy 13 6.3 Safety 13 6.3.1 Liver chemistry stopping and follow-up criteria 15 6.4 Adverse Events 16 6.4.1 Definition of an AE 16 6.4.2 Definition of a SAE 17 6.4.3 Disease-Related Events and/or Disease-Related Outcomes Not Qualifying as SAEs -

Osteoporosis in Skin Diseases
International Journal of Molecular Sciences Review Osteoporosis in Skin Diseases Maria Maddalena Sirufo 1,2, Francesca De Pietro 1,2, Enrica Maria Bassino 1,2, Lia Ginaldi 1,2 and Massimo De Martinis 1,2,* 1 Department of Life, Health and Environmental Sciences, University of L’Aquila, 67100 L’Aquila, Italy; [email protected] (M.M.S.); [email protected] (F.D.P.); [email protected] (E.M.B.); [email protected] (L.G.) 2 Allergy and Clinical Immunology Unit, Center for the Diagnosis and Treatment of Osteoporosis, AUSL 04 64100 Teramo, Italy * Correspondence: [email protected]; Tel.: +39-0861-429548; Fax: +39-0861-211395 Received: 1 June 2020; Accepted: 1 July 2020; Published: 3 July 2020 Abstract: Osteoporosis (OP) is defined as a generalized skeletal disease characterized by low bone mass and an alteration of the microarchitecture that lead to an increase in bone fragility and, therefore, an increased risk of fractures. It must be considered today as a true public health problem and the most widespread metabolic bone disease that affects more than 200 million people worldwide. Under physiological conditions, there is a balance between bone formation and bone resorption necessary for skeletal homeostasis. In pathological situations, this balance is altered in favor of osteoclast (OC)-mediated bone resorption. During chronic inflammation, the balance between bone formation and bone resorption may be considerably affected, contributing to a net prevalence of osteoclastogenesis. Skin diseases are the fourth cause of human disease in the world, affecting approximately one third of the world’s population with a prevalence in elderly men. -

RIPE for the PICKING Experts Profile the Future of Biologic Treatments
RIPE FOR THE PICKING Experts profile the future of biologic treatments 22 DERMATOLOGY WORLD // September 2015 www.aad.org/dw BY VICTORIA HOUGHTON, ASSISTANT MANAGING EDITOR John Harris, MD, PhD, assistant professor of medicine at the University of Massachusetts in the division of dermatology — like many dermatologists — has watched the impressive evolution of treatments for psoriasis over the last decade with anticipation. “We initially had very broad immunosuppressants that were somewhat effective in some patients, but they also had significant side effects,” Dr. Harris said. However, “The onset of biologics and other targeted therapies has been incredible. They’ve revolutionized treatment for psoriasis.” However, while physicians are enthusiastic about the progress of these treatments for psoriasis, there is also hope that interest in developing these innovative therapies is increasingly shifting to other skin conditions. “Pharmaceutical companies have to start looking elsewhere, given how good current psoriasis therapies are,” Dr. Harris said. “The real room for growth is in other diseases.” As psoriasis has paved the way for an interest in developing biologic and other targeted treatments in skin conditions, physicians are anticipating a promising future for these treatments in the following conditions: Atopic dermatitis Hidradenitis suppurativa Chronic urticaria Vitiligo Dermatomyositis >> Alopecia areata DERMATOLOGY WORLD // September 2015 23 RIPE FOR THE PICKING Atopic dermatitis 133; 6:1626-34). The study showed that by blocking the According to Lawrence Eichenfield, MD, professor of immune pathways with CsA, the molecular abnormalities dermatology and pediatrics at the University of California, with AD skin barrier genes, such as filaggrin and loricrin, San Diego and chief of pediatric and adolescent dermatology normalized.