Pleurisy and Pleural Effusion”
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pleural Effusion and Ventilation/Perfusion Scan Interpretation for Acute Pulmonary Embolus
ventricular function by radionuclide angiography during exercise in normal subjects 33. Verani MS. Myocardial perfusion imaging versus two-dimensional echocardiography: and patients with chronic coronary heart disease. J Am Coll Cardiol 1983;1:1518- comparative value in the diagnosis of coronary artery disease. J NucÃCardiol 1529. 1994;1:399-414. 29. Adam WE. Tarkowska A, Bitter F, Stauch M, Geffers H. Equilibrium (gated) 34. Foster T, McNeill AJ, Salustri A, et al. Simultaneous dobutamine stress echocardiog radionuclide ventriculography. Cardiovasc Radial 1979;2:161-173. raphy and technetium-99m SPECT in patients with suspected coronary artery disease. 30. Hurwitz RA, TrêvesS, Kuroc A. Right ventricular and left ventricular ejection fraction J Am Coll Cardiol I993;21:1591-I596. in pediatrie patients with normal hearts: first pass radionuclide angiography. Am 35. Marwick TH, D'Hondt AM, Mairesse GH, Baudhuin T, Wijins W, Detry JM, Meiin Heart J 1984;107:726-732. 31. Freeman ML, Palac R, Mason J, et al. A comparison of dobutamine infusion and JA. Comparative ability of dobutamine and exercise stress in inducing myocardial ischemia in active patients. Br Heart J 1994:72:31-38. supine bicycle exercise for radionuclide cardiac stress testing. Clin NucÃMed 1984:9:251-255. 36. Senior R, Sridhara BS, Anagnostou E, Handler C, Raftery EB, Lahiri A. Synergistic 32. Cohen JL, Greene TO, Ottenweller J, Binebaum SZ, Wilchfort SD, Kim CS. value of simultaneous stress dobutamine sestamibi single-photon-emission computer Dobutamine digital echocardiography for detecting coronary artery disease. Am J ized tomography and echocardiography in the detection of coronary artery disease. -

Bronchiolitis Obliterans After Severe Adenovirus Pneumonia:A Review of 46 Cases
Bronchiolitis obliterans after severe adenovirus pneumonia:a review of 46 cases Yuan-Mei Lan medical college of XiaMen University Yun-Gang Yang ( [email protected] ) Xiamen University and Fujian Medical University Aliated First Hospital Xiao-Liang Lin Xiamen University and Fujian Medical University Aliated First Hospital Qi-Hong Chen Fujian Medical University Research article Keywords: Bronchiolitis obliterans, Adenovirus, Pneumonia, Children Posted Date: October 26th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-93838/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/13 Abstract Background:This study aimed to investigate the risk factors of bronchiolitis obliterans caused by severe adenovirus pneumonia. Methods: The First Aliated Hospital of Xiamen University in January, 2019 was collected The clinical data of 229 children with severe adenovirus pneumonia from January to January 2020 were divided into obliterative bronchiolitis group (BO group) and non obstructive bronchiolitis group (non BO group) according to the follow-up clinical manifestations and imaging data. The clinical data, laboratory examination and imaging data of the children were retrospectively analyzed. Results: Among 229 children with severe adenovirus pneumonia, 46 cases were in BO group. The number of days of hospitalization, oxygen consumption time, LDH, IL-6, AST, D-dimer and hypoxemia in BO group were signicantly higher than those in non BO group; The difference was statistically signicant (P < 0.05). Univariate logistic regression analysis showed that there were signicant differences in the blood routine neutrophil ratio, platelet level, Oxygen supply time, hospitalization days, AST level, whether there was hypoxemia, timing of using hormone, more than two bacterial feelings were found in the two groups, levels of LDH, albumin and Scope of lung imaging (P < 0.05). -

Pneumothorax Ex Vacuo in a Patient with Malignant Pleural Effusion After Pleurx Catheter Placement
The Medicine Forum Volume 16 Article 20 2015 Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 Thomas Jefferson University, [email protected] Loheetha Ragupathi, MD Thomas Jefferson University, [email protected] Follow this and additional works at: https://jdc.jefferson.edu/tmf Part of the Medicine and Health Sciences Commons Let us know how access to this document benefits ouy Recommended Citation Bhardwaj, MS4, Meera and Ragupathi, MD, Loheetha (2015) "Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement," The Medicine Forum: Vol. 16 , Article 20. DOI: https://doi.org/10.29046/TMF.016.1.019 Available at: https://jdc.jefferson.edu/tmf/vol16/iss1/20 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in The Medicine Forum by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Bhardwaj, MS4 and Ragupathi, MD: Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Pneumothorax ex vacuo in a Patient with Malignant Pleural Effusion After PleurX Catheter Placement Meera Bhardwaj, MS4 and Loheetha Ragupathi, MD INTRODUCTION Pneumothorax ex vacuo (“without vaccuum”) is a type of pneumothorax that can develop in patients with large pleural effusions. -

Slipping Rib Syndrome
Slipping Rib Syndrome Jackie Dozier, BS Edited by Lisa E McMahon, MD FACS FAAP David M Notrica, MD FACS FAAP Case Presentation AA is a 12 year old female who presented with a 7 month history of right-sided chest/rib pain. She states that the pain was not preceded by trauma and she had never experienced pain like this before. She has been seen in the past by her pediatrician, chiropractor, and sports medicine physician for her pain. In May 2012, she was seen in the ER after having manipulations done on her ribs by a sports medicine physician. Pain at that time was constant throughout the day and kept her from sleeping. However, it was relieved with hydrocodone/acetaminophen in the ER. Case Presentation Over the following months, the pain became progressively worse and then constant. She also developed shortness of breath. She is a swimmer and says she has had difficulty practicing due to the pain and SOB. AA was seen by a pediatric surgeon and scheduled for an interventional pain management service consult for a test injection. Following good temporary relief by local injection, she was scheduled costal cartilage removal to treat her pain. What is Slipping Rib Syndrome? •Slipping Rib Syndrome (SRS) is caused by hypermobility of the anterior ends of the false rib costal cartilages, which leads to slipping of the affected rib under the superior adjacent rib. •SRS an lead to irritation of the intercostal nerve or strain of the muscles surrounding the rib. •SRS is often misdiagnosed and can lead to months or years of unresolved abdominal and/or thoracic pain. -
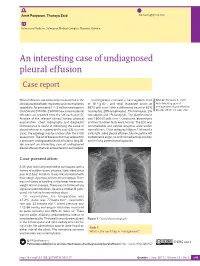
An Interesting Case of Undiagnosed Pleural Effusion Case Report
Amit Panjwani, Thuraya Zaid [email protected] Pulmonary Medicine, Salmaniya Medical Complex, Manama, Bahrain. An interesting case of undiagnosed pleural effusion Case report Pleural effusions are commonly encountered in the Investigations revealed a haemoglobin level Cite as: Panjwani A, Zaid T. clinical practise of both respiratory and nonrespiratory of 16.4 g⋅dL−1, and total leukocyte count of An interesting case of specialists. An estimated 1–1.5 million new cases in 8870 cells⋅mm−3 with a differential count of 62% undiagnosed pleural effusion. the USA and 200 000–250 000 new cases of pleural neutrophils, 28% lymphocytes, 7% monocytes, 2% Breathe 2017; 13: e46–e52. effusions are reported from the UK each year [1]. eosinophils and 1% basophils. The platelet count Analysis of the relevant clinical history, physical was 160 000 cells⋅mm−3. Creatinine, electrolytes examination, chest radiography and diagnostic and liver function tests were normal. The ECG was thoracentesis is useful in identifying the cause of unremarkable and cardiac enzymes were within pleural effusion in majority of the cases [2]. In a few normal limits. Chest radiograph (figure 1) showed a cases, the aetiology may be unclear after the initial mild, right-sided pleural effusion, blunting of the left assessment. The list of diseases that may account for costophrenic angle, no shift of mediastinal position a persistent undiagnosed pleural effusion is long [3]. and no lung parenchymal opacities. We present an interesting case of undiagnosed pleural effusion that was encountered in our hospital. R Case presentation A 33-year-old male presented to our hospital with a history of sudden-onset, pleuritic, right-sided chest pain of 2 days’ duration. -

Signs and Symptoms of COPD
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES Signs and Symptoms of COPD Chronic obstructive pulmonary disease (COPD) can cause shortness of breath, tiredness, Short ness of Breath production of mucus, and cough. Many people with COPD develop most if not all, of these signs Avo iding Activities and symptoms. Sho rtness wit of Breath h Man s Why is shortness of breath a symptom of COPD? y Activitie Shortness of breath (or breathlessness) is a common Avoiding symptom of COPD because the obstruction in the A breathing tubes makes it difficult to move air in and ny Activity out of your lungs. This produces a feeling of difficulty breathing (See ATS Patient Information Series fact sheet Shor f B tness o on Breathlessness). Unfortunately, people try to avoid this reath Sitting feeling by becoming less and less active. This plan may or Standing work at first, but in time it leads to a downward spiral of: avoiding activities which leads to getting out of shape or becoming deconditioned, and this can result in even more Is tiredness a symptom of COPD? shortness of breath with activity (see diagram). Tiredness (or fatigue) is a common symptom in COPD. What can I do to treat shortness of breath? Tiredness may discourage you from keeping active, which leads to greater loss of energy, which then leads to more If your shortness of breath is from COPD, you can do several tiredness. When this cycle begins it is sometimes hard to things to control it: break. CLIP AND COPY AND CLIP ■■ Take your medications regularly. -

Acute (Serious) Bronchitis
Acute (serious) Bronchitis This is an infection of the air tubes that go down to your lungs. It often follows a cold or the flu. Most people do not need treatment for this. The infection normally goes away in 7-10 days. We make every effort to make sure the information is correct (right). However, we cannot be responsible for any actions as a result of using this information. Getting Acute Bronchitis How the lungs work Your lungs are like two large sponges filled with tubes. As you breathe in, you suck oxygen through your nose and mouth into a tube in your neck. Bacteria and viruses in the air can travel into your lungs. Normally, this does not cause a problem as your body kills the bacteria, or viruses. However, sometimes infection can get through. If you smoke or if you have had another illness, infections are more likely to get through. Acute Bronchitis Acute bronchitis is when the large airways (breathing tubes) to the lungs get inflamed (swollen and sore). The infection makes the airways swell and you get a build up of phlegm (thick mucus). Coughing is a way of getting the phlegm out of your airways. The cough can sometimes last for up to 3 weeks. Acute Bronchitis usually goes away on its own and does not need treatment. We make every effort to make sure the information is correct (right). However, we cannot be responsible for any actions as a result of using this information. Symptoms (feelings that show you may have the illness) Symptoms of Acute Bronchitis include: • A chesty cough • Coughing up mucus, which is usually yellow, or green • Breathlessness when doing more energetic activities • Wheeziness • Dry mouth • High temperature • Headache • Loss of appetite The cough usually lasts between 7-10 days. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

New Jersey Chapter American College of Physicians
NEW JERSEY CHAPTER AMERICAN COLLEGE OF PHYSICIANS ASSOCIATES ABSTRACT COMPETITION 2015 SUBMISSIONS 2015 Resident/Fellow Abstracts 1 1. ID CATEGORY NAME ADDITIONAL PROGRAM ABSTRACT AUTHORS 2. 295 Clinical Abed, Kareem Viren Vankawala MD Atlanticare Intrapulmonary Arteriovenous Malformation causing Recurrent Cerebral Emboli Vignette FACC; Qi Sun MD Regional Medical Ischemic strokes are mainly due to cardioembolic occlusion of small vessels, as well as large vessel thromboemboli. We describe a Center case of intrapulmonary A-V shunt as the etiology of an acute ischemic event. A 63 year old male with a past history of (Dominik supraventricular tachycardia and recurrent deep vein thrombosis; who has been non-compliant on Rivaroxaban, presents with Zampino) pleuritic chest pain and was found to have a right lower lobe pulmonary embolus. The deep vein thrombosis and pulmonary embolus were not significant enough to warrant ultrasound-enhanced thrombolysis by Ekosonic EndoWave Infusion Catheter System, and the patient was subsequently restarted on Rivaroxaban and discharged. The patient presented five days later with left arm tightness and was found to have multiple areas of punctuate infarction of both cerebellar hemispheres, more confluent within the right frontal lobe. Of note he was compliant at this time with Rivaroxaban. The patient was started on unfractionated heparin drip and subsequently admitted. On admission, his vital signs showed a blood pressure of 138/93, heart rate 65 bpm, and respiratory rate 16. Cardiopulmonary examination revealed regular rate and rhythm, without murmurs, rubs or gallops and his lungs were clear to auscultation. Neurologic examination revealed intact cranial nerves, preserved strength in all extremities, mild dysmetria in the left upper extremity and an NIH score of 1. -

Octreotide Treatment of Idiopathic Pulmonary Fibrosis: a Proof-Of-Concept Study
drugs, while two patients underwent surgery in addition to Roncaccio 16, 21049, Tradate, Italy. E-mail: giovannibattista. chemotherapy. [email protected] As in other reference centres, the E. Morelli Hospital needs to transfer out all admitted cases to the hospitals referring them for Support Statement: This study was supported by the current specialised treatment, when culture conversion and clinical research funds of the participating institutions. For this stability have been achieved. Patients were transferred out after publication, the research leading to these results has received a median (IQR) hospital stay of 75.5 (51.5–127.5) days; 12 (100%) funding from the European Community’s Seventh Framework out of 12 and nine (75%) out of 12 achieved sputum-smear and Programme (FP7/2007-2013) under grant agreement FP7- culture conversion, after a median (IQR) time of 40.5 (24–64) and 223681. 70 (44–95) days, respectively. As of June 2011, one patient was cured, two had died and nine were still under treatment. Statement of Interest: None declared. Four (33.3%) cases reported adverse events, two being major (16.7%; neuropathy and low platelet count, needing temporary REFERENCES interruption of linezolid) and two minor (neuropathy and mild 1 Villar M, Sotgiu G, D’Ambrosio L, et al. Linezolid safety, anaemia). All adverse events were reversible. tolerability and efficacy to treat multidrug- and extensively drug-resistant tuberculosis. Eur Respir J 2011; 38: 730–733. In conclusion, despite the intrinsic difficulty of evaluating the 2 World Health Organization. Multidrug and extensively drug safety and tolerability of linezolid (administered within different resistant TB (M/XDR-TB): 2010 global report on surveillance and regimens including multiple anti-TB drugs guided by drug response. -
Problem Based Review: Pleuritic Chest Pain
172 Acute Medicine 2012; 11(3): 172-182 Trainee Section 172 Problem based review: Pleuritic Chest Pain RW Lee, LE Hodgson, MB Jackson & N Adams Abstract Pleuritic pain, a sharp discomfort near the chest wall exacerbated by inspiration is associated with a number of pathologies. Pulmonary embolus and infection are two common causes but diagnosis can often be challenging, both for experienced physicians and trainees. The underlying anatomy and pathophysiology of such pain and the most common aetiologies are presented. Clinical symptoms and signs that may arise alongside pleuritic pain are then discussed, followed by an introduction to the diagnostic tools such as the Wells’ score and current guidelines that can help to select the most appropriate investigation(s). Management of pulmonary embolism and other common causes of pleuritic pain are also discussed and highlighted by a clinical vignette. Keywords Pleuritic pain, pulmonary embolus, pleurisy, chest pain Key Points 1. Pleuritic chest pain is a common reason for presentation to hospital. 2. Pulmonary embolism is a common, potentially life-threatening cause but can be difficult to diagnose, with clear overlap Richard William Lee between typical presentations. MBBS, MRCP, MA 3. Excluding other differential diagnoses can be difficult without definitive investigation e.g. CT Pulmonary Angiography (Cantab.) (CTPA). Respiratory Registrar, 4. Clinical probability and scoring systems (e.g. Wells’ score) can assist the physician in further management. Darent Valley Hospital 5. Several key guidelines from the thoracic and cardiological societies provide useful algorithms for investigation and further reading. Luke Eliot Hodgson MBBS, MRCP, MSc Respiratory Registrar, Introduction Brighton & Sussex Case History University Hospitals NHS Pleuritic pain is a sharp, ‘catching’ pain perceived A 37 year-old male smoker, with no previous medical Trust. -

Allergic Bronchopulmonary Aspergillosis: a Perplexing Clinical Entity Ashok Shah,1* Chandramani Panjabi2
Review Allergy Asthma Immunol Res. 2016 July;8(4):282-297. http://dx.doi.org/10.4168/aair.2016.8.4.282 pISSN 2092-7355 • eISSN 2092-7363 Allergic Bronchopulmonary Aspergillosis: A Perplexing Clinical Entity Ashok Shah,1* Chandramani Panjabi2 1Department of Pulmonary Medicine, Vallabhbhai Patel Chest Institute, University of Delhi, Delhi, India 2Department of Respiratory Medicine, Mata Chanan Devi Hospital, New Delhi, India This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. In susceptible individuals, inhalation of Aspergillus spores can affect the respiratory tract in many ways. These spores get trapped in the viscid spu- tum of asthmatic subjects which triggers a cascade of inflammatory reactions that can result in Aspergillus-induced asthma, allergic bronchopulmo- nary aspergillosis (ABPA), and allergic Aspergillus sinusitis (AAS). An immunologically mediated disease, ABPA, occurs predominantly in patients with asthma and cystic fibrosis (CF). A set of criteria, which is still evolving, is required for diagnosis. Imaging plays a compelling role in the diagno- sis and monitoring of the disease. Demonstration of central bronchiectasis with normal tapering bronchi is still considered pathognomonic in pa- tients without CF. Elevated serum IgE levels and Aspergillus-specific IgE and/or IgG are also vital for the diagnosis. Mucoid impaction occurring in the paranasal sinuses results in AAS, which also requires a set of diagnostic criteria. Demonstration of fungal elements in sinus material is the hall- mark of AAS.