A Guide to the Review of Systems
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Advanced Interpretation of Adult Vital Signs in Trauma William D
Advanced Interpretation of Adult Vital Signs in Trauma William D. Hampton, DO Emergency Physician 26 March 2015 Learning Objectives 1. Better understand vital signs for what they can tell you (and what they can’t) in the assessment of a trauma patient. 2. Appreciate best practices in obtaining accurate vital signs in trauma patients. 3. Learn what teaching about vital signs is evidence-based and what is not. 4. Explain the importance of vital signs to more accurately triage, diagnose, and confidently disposition our trauma patients. 5. Apply the monitoring (and manipulation of) vital signs to better resuscitate trauma patients. Disclosure Statement • Faculty/Presenters/Authors/Content Reviewers/Planners disclose no conflict of interest relative to this educational activity. Successful Completion • To successfully complete this course, participants must attend the entire event and complete/submit the evaluation at the end of the session. • Society of Trauma Nurses is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission on Accreditation. Vital Signs Vital Signs Philosophy: “View vital signs as compensatory to the illness/complaint as opposed to primary.” Crowe, Donald MD. “Vital Sign Rant.” EMRAP: Emergency Medicine Reviews and Perspectives. February, 2010. Vital Signs Truth over Accuracy: • Document the true status of the patient: sick or not? • Complete vital signs on every patient, every time, regardless of the chief complaint. • If vital signs seem misleading or inaccurate, repeat them! • Beware sending a patient home with abnormal vitals (especially tachycardia)! •Treat vital signs the same as any other diagnostics— review them carefully prior to disposition. The Mother’s Vital Sign: Temperature Case #1 - 76-y/o homeless ♂ CC: 76-y/o homeless ♂ brought to the ED by police for eval. -

Cardiovascular Assessment
Cardiovascular Assessment A Home study Course Offered by Nurses Research Publications P.O. Box 480 Hayward CA 94543-0480 Office: 510-888-9070 Fax: 510-537-3434 No unauthorized duplication photocopying of this course is permitted Editor: Nurses Research 1 HOW TO USE THIS COURSE Thank you for choosing Nurses Research Publication home study for your continuing education. This course may be completed as rapidly as you desire. However there is a one-year maximum time limit. If you have downloaded this course from our website you will need to log back on to pay and complete your test. After you submit your test for grading you will be asked to complete a course evaluation and then your certificate of completion will appear on your screen for you to print and keep for your records. Satisfactory completion of the examination requires a passing score of at least 70%. No part of this course may be copied or circulated under copyright law. Instructions: 1. Read the course objectives. 2. Read and study the course. 3. Log back onto our website to pay and take the test. If you have already paid for the course you will be asked to login using the username and password you selected when you registered for the course. 4. When you are satisfied that the answers are correct click grade test. 5. Complete the evaluation. 6. Print your certificate of completion. If you have a procedural question or “nursing” question regarding the materials, call (510) 888-9070 for assistance. Only instructors or our director may answer a nursing question about the test. -

(June 2000) I. INTRODUCTION WHAT IS DOCUMENTATION and WHY
DRAFT EVALUATION & MANAGEMENT DOCUMENTATION GUIDELINES (June 2000) I. INTRODUCTION WHAT IS DOCUMENTATION AND WHY IS IT IMPORTANT? Medical record documentation is required to record pertinent facts, findings, and observations about an individual's health history including past and present illnesses, examinations, tests, treatments, and outcomes. The medical record chronologically documents the care of the patient and is an important element contributing to high quality care. The medical record facilitates: · the ability of the physician and other health care professionals to evaluate and plan the patient's immediate treatment, and to monitor his/her health care over time. · communication and continuity of care among physicians and other health care professionals involved in the patient's care; · accurate and timely claims review and payment; · appropriate utilization review and quality of care evaluations; and · collection of data that may be useful for research and education. An appropriately documented medical record can reduce many of the "hassles" associated with claims processing and may serve as a legal document to verify the care provided, if necessary. WHAT DO PAYERS WANT AND WHY? Because payers have a contractual obligation to enrollees, they may require reasonable documentation that services are consistent with the insurance coverage provided. They may request information to validate: · the site of service; · the medical necessity and appropriateness of the diagnostic and/or therapeutic services provided; and/or · that services provided have been accurately reported. II. GENERAL PRINCIPLES OF MEDICAL RECORD DOCUMENTATION The principles of documentation listed below are applicable to all types of medical and surgical Pg. 1 services in all settings. For Evaluation and Management (E/M) services, the nature and amount of physician work and documentation varies by type of service, place of service and the patient's status. -

Review of Systems
code: GF004 REVIEW OF SYSTEMS First Name Middle Name / MI Last Name Check the box if you are currently experiencing any of the following : General Skin Respiratory Arthritis/Rheumatism Abnormal Pigmentation Any Lung Troubles Back Pain (recurrent) Boils Asthma or Wheezing Bone Fracture Brittle Nails Bronchitis Cancer Dry Skin Chronic or Frequent Cough Diabetes Eczema Difficulty Breathing Foot Pain Frequent infections Pleurisy or Pneumonia Gout Hair/Nail changes Spitting up Blood Headaches/Migraines Hives Trouble Breathing Joint Injury Itching URI (Cold) Now Memory Loss Jaundice None Muscle Weakness Psoriasis Numbness/Tingling Rash Obesity Skin Disease Osteoporosis None Rheumatic Fever Weight Gain/Loss None Cardiovascular Gastrointestinal Eyes - Ears - Nose - Throat/Mouth Awakening in the night smothering Abdominal Pain Blurring Chest Pain or Angina Appetite Changes Double Vision Congestive Heart Failure Black Stools Eye Disease or Injury Cyanosis (blue skin) Bleeding with Bowel Movements Eye Pain/Discharge Difficulty walking two blocks Blood in Vomit Glasses Edema/Swelling of Hands, Feet or Ankles Chrohn’s Disease/Colitis Glaucoma Heart Attacks Constipation Itchy Eyes Heart Murmur Cramping or pain in the Abdomen Vision changes Heart Trouble Difficulty Swallowing Ear Disease High Blood Pressure Diverticulosis Ear Infections Irregular Heartbeat Frequent Diarrhea Ears ringing Pain in legs Gallbladder Disease Hearing problems Palpitations Gas/Bloating Impaired Hearing Poor Circulation Heartburn or Indigestion Chronic Sinus Trouble Shortness -

Review of Systems – Return Visit Have You Had Any Problems Related to the Following Symptoms in the Past Month? Circle Yes Or No
REVIEW OF SYSTEMS – RETURN VISIT HAVE YOU HAD ANY PROBLEMS RELATED TO THE FOLLOWING SYMPTOMS IN THE PAST MONTH? CIRCLE YES OR NO Today’s Date: ______________ Name: _______________________________ Date of Birth: __________________ GENERAL GENITOURINARY Fatigue Y N Blood in Urine Y N Fever / Chills Y N Menstrual Irregularity Y N Night Sweats Y N Painful Menstrual Cycle Y N Weight Gain Y N Vaginal Discharge Y N Weight Loss Y N Vaginal Dryness Y N EYES Vaginal Itching Y N Vision Changes Y N Painful Sex Y N EAR, NOSE, & THROAT SKIN Hearing Loss Y N Hair Loss Y N Runny Nose Y N New Skin Lesions Y N Ringing in Ears Y N Rash Y N Sinus Problem Y N Pigmentation Change Y N Sore Throat Y N NEUROLOGIC BREAST Headache Y N Breast Lump Y N Muscular Weakness Y N Tenderness Y N Tingling or Numbness Y N Nipple Discharge Y N Memory Difficulties Y N CARDIOVASCULAR MUSCULOSKELETAL Chest Pain Y N Back Pain Y N Swelling in Legs Y N Limitation of Motion Y N Palpitations Y N Joint Pain Y N Fainting Y N Muscle Pain Y N Irregular Heart Beat Y N ENDOCRINE RESPIRATORY Cold Intolerance Y N Cough Y N Heat Intolerance Y N Shortness of Breath Y N Excessive Thirst Y N Post Nasal Drip Y N Excessive Amount of Urine Y N Wheezing Y N PSYCHOLOGY GASTROINTESTINAL Difficulty Sleeping Y N Abdominal Pain Y N Depression Y N Constipation Y N Anxiety Y N Diarrhea Y N Suicidal Thoughts Y N Hemorrhoids Y N HEMATOLOGIC / LYMPHATIC Nausea Y N Easy Bruising Y N Vomiting Y N Easy Bleeding Y N GENITOURINARY Swollen Lymph Glands Y N Burning with Urination Y N ALLERGY / IMMUNOLOGY Urinary -

Patient/ Family History
Patient/ Family Mankato History Location: Mankato Fairmont New Prague Springfield St. James Waseca PATIENT PROVIDED INFORMATION The information you provide us will greatly help us to provide the highest quality and comprehensive care for you. Date Gender Male Female Date of birth (Month/Day/Year) A. PAST MEDICAL HISTORY 1. Have you ever traveled or lived outside of the United States or Canada? Do not know No Yes 2. Have you ever received a blood transfusion? Do not know No Yes (If yes, check all that apply.) Before 1980 1980-1990 After 1990 3. Have you received the following immunizations and/or had the disease? Pneumococcal (For pneumonia) Do not know No Yes Mumps Do not know No Yes Hepatitis B Do not know No Yes Rubella Do not know No Yes Hepatitis A Do not know No Yes Polio Do not know No Yes Measles Do not know No Yes Varicella (For chicken pox) Do not know No Yes 4. Indicate whether you have ever had a medical problem or surgery related to each of the following. Check all that apply. Medical Problem Surgery/Year Medical Problem Surgery/Year Eyes Lungs Ears Esophagus (Food or swallowing pipe) Nose Stomach (Ulcer) Sinuses Bowel (Small or large intestine, rectum) Tonsils Appendix Thyroid or parathyroid gland Lymph nodes Heart problems: Spleen Heart attack Liver Heart valves Gallbladder Abnormal heart rhythm Pancreas Narrowed coronary arteries Hernia Other Kidneys Arteries (Head, arms, legs, aorta, etc.) Bladder Veins or blood clots in the veins Bones ©2014 Mayo Foundation for Medical Education and Research Page 1 of 4 1081MR rev10/14 (Label) Patient Name DOB Unit No. -
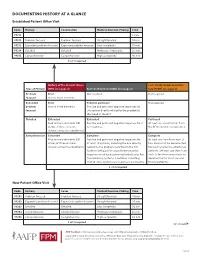
Documenting History at a Glance
DOCUMENTING HISTORY AT A GLANCE Established Patient Office Visit Code History Examination Medical Decision-Making Time 99211 — — — 5 min. 99212 Problem focused Problem focused Straightforward 10 min. 99213 Expanded problem focused Expanded problem focused Low complexity 15 min. 99214 Detailed Detailed Moderate complexity 25 min. 99215 Comprehensive Comprehensive High complexity 40 min. 2 of 3 required History of the Present Illness Past, Family and/or Social His- Type of History (HPI) (see page 2) Review of Systems (ROS) (see page 2) tory (PFSH) (see page 2) Problem Brief Not required Not required focused One to three elements Expanded Brief Problem pertinent Not required problem One to three elements Positive and pertinent negative responses for focused the system directly related to the problem(s) identified in the HPI. Detailed Extended Extended Pertinent Four or more elements (OR Positive and pertinent negative responses for 2 At least one specific item from status of three or more to 9 systems. the PFSH must be documented. chronic or inactive conditions) Comprehensive Extended Complete Complete Four or more elements (OR Positive and pertinent negative responses for At least one item from each of status of three or more at least 10 systems, including the one directly two areas must be documented chronic or inactive conditions) related to the problem identified in the HPI. for most services to established Systems with positive or pertinent negative patients. (At least one item from responses must be documented individually. For each of the three areas must be the remaining systems, a notation indicating documented for most services that all other systems are negative is permissible. -

GUIDELINES for WRITING SOAP NOTES and HISTORY and PHYSICALS
GUIDELINES FOR WRITING SOAP NOTES and HISTORY AND PHYSICALS by Lois E. Brenneman, M.S.N, C.S., A.N.P, F.N.P. © 2001 NPCEU Inc. all rights reserved NPCEU INC. PO Box 246 Glen Gardner, NJ 08826 908-537-9767 - FAX 908-537-6409 www.npceu.com Copyright © 2001 NPCEU Inc. All rights reserved No part of this book may be reproduced in any manner whatever, including information storage, or retrieval, in whole or in part (except for brief quotations in critical articles or reviews), without written permission of the publisher: NPCEU, Inc. PO Box 246, Glen Gardner, NJ 08826 908-527-9767, Fax 908-527-6409. Bulk Purchase Discounts. For discounts on orders of 20 copies or more, please fax the number above or write the address above. Please state if you are a non-profit organization and the number of copies you are interested in purchasing. 2 GUIDELINES FOR WRITING SOAP NOTES and HISTORY AND PHYSICALS Lois E. Brenneman, M.S.N., C.S., A.N.P., F.N.P. Written documentation for clinical management of patients within health care settings usually include one or more of the following components. - Problem Statement (Chief Complaint) - Subjective (History) - Objective (Physical Exam/Diagnostics) - Assessment (Diagnoses) - Plan (Orders) - Rationale (Clinical Decision Making) Expertise and quality in clinical write-ups is somewhat of an art-form which develops over time as the student/practitioner gains practice and professional experience. In general, students are encouraged to review patient charts, reading as many H/Ps, progress notes and consult reports, as possible. In so doing, one gains insight into a variety of writing styles and methods of conveying clinical information. -

Polyphagia Ellen N
W0117-Section I (31-50).qxd 4/23/04 7:26 PM Page 124 CHAPTER • 34 Polyphagia Ellen N. Behrend olyphagia is the consumption of food in excess of and liver disease) lead to polyphagia by unknown mecha- normal caloric intake. Hunger and satiety and, conse- nisms. Secondary polyphagia can also be caused by certain P quently, feeding behavior are primarily controlled by drugs. certain regions in the central nervous system (CNS), but many factors affect the function of these areas. Thus polypha- gia can be classified as primary (i.e., a CNS abnormality) or HISTORY secondary (i.e., a systemic problem affecting the CNS). Secondary polyphagia is by far more common and usually is Any change in body weight is an important differentiating accompanied by clinical signs of the underlying disease. feature of the various causes of polyphagia (Figure 34-1). Determining whether weight gain or loss has occurred should Primary or drug-induced polyphagia typically results in weight be the first step in formulating a list of differential diagnoses gain, because nutrients are adequate and feeding is inappro- and a diagnostic plan. priately increased. Pathologic secondary polyphagia is more commonly associated with weight loss, because the nutrient supply usually does not meet physiologic demands. However, PHYSIOLOGY some causes, such as acromegaly, hypoglycemia caused by an insulinoma, sudden acquired retinal degeneration syndrome Food intake is controlled by a variety of factors, including gas- (SARDS), and hyperadrenocorticism (HAC), lead to weight trointestinal, environmental, and CNS phenomena. The CNS, gain. Physiologic polyphagia can result in weight gain (e.g., mainly the hypothalamus, controls eating behavior.The lateral pregnancy, growth) or maintenance of weight (e.g., lactation, hypothalamic nuclei represent the “feeding center”; their cold environment, increased exercise). -

Sudden Death in Eating Disorders
Vascular Health and Risk Management Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Sudden death in eating disorders Beatriz Jáuregui-Garrido1 Abstract: Eating disorders are usually associated with an increased risk of premature death Ignacio Jáuregui-Lobera2,3 with a wide range of rates and causes of mortality. “Sudden death” has been defined as the abrupt and unexpected occurrence of fatality for which no satisfactory explanation of the 1Department of Cardiology, University Hospital Virgen del Rocío, 2Behavioral cause can be ascertained. In many cases of sudden death, autopsies do not clarify the main Sciences Institute, 3Pablo de Olavide cause. Cardiovascular complications are usually involved in these deaths. The purpose of University, Seville, Spain this review was to report an update of the existing literature data on the main findings with respect to sudden death in eating disorders by means of a search conducted in PubMed. The most relevant conclusion of this review seems to be that the main causes of sudden death in eating disorders are those related to cardiovascular complications. The predictive value of the For personal use only. increased QT interval dispersion as a marker of sudden acute ventricular arrhythmia and death has been demonstrated. Eating disorder patients with severe cardiovascular symptoms should be hospitalized. In general, with respect to sudden death in eating disorders, some findings (eg, long-term eating disorders, chronic hypokalemia, chronically low plasma albumin, and QT intervals .600 milliseconds) must be taken into account, and it must be highlighted that during refeeding, the adverse effects of hypophosphatemia include cardiac failure. -
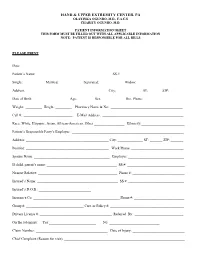
Patient Information Sheet This Form Must Be Filled out with All Applicable Information Note: Patient Is Responsible for All Bills
HAND & UPPER EXTREMITY CENTER, PA OLAYINKA OGUNRO, M.D., F.A.C.S CHARITY OGUNRO, M.D. PATIENT INFORMATION SHEET THIS FORM MUST BE FILLED OUT WITH ALL APPLICABLE INFORMATION NOTE: PATIENT IS RESPONSIBLE FOR ALL BILLS PLEASE PRINT Date: ________________________________________ Patient’s Name: _________________________________________ SS #: __________________________________ Single: __________ Married: ___________ Separated: ___________ Widow: ____________ Address: _____________________________________________ City: _____________ ST: ______ ZIP:________ Date of Birth: ___________________ Age:_________ Sex: ____________ Hm. Phone: ______________________ Weight: _________ Height: _________ Pharmacy Name & No: ________________________________________ Cell #: ___________________________ E-Mail Address: _____________________________________________ Race: White, Hispanic, Asian, African-American, Other _________________ Ethnicity:________________________ Patient’s Responsible Party’s Employer: ______________________________________________________________ Address: ______________________________________________ City: ______________ ST: _______ ZIP: _______ Position: ______________________________________________ Work Phone: _____________________________ Spouse Name: __________________________________________ Employer: _______________________________ If child, parent’s name: _______________________________________ SS #: ________________________________ Nearest Relative: ____________________________________________ Phone #: _____________________________ -

Medical History and Physical Examination Worksheet
U.S. Department of State OMB No. 1405-0113 EXPIRATION DATE: xx/xx/xxxx MEDICAL HISTORY AND PHYSICAL EXAMINATION WORKSHEET ESTIMATED BURDEN: 35 minutes For use with DS-2053 (See Page 2 - Back of Form) Name (Last, First, MI) Exam Date (mm-dd-yyyy) Birth Date (mm-dd-yyyy) Passport Number Alien (Case) Number 1. Past Medical History (indicate conditions requiring medication or other treatment after resettlement and give details in Remarks) NOTE: The following history has been reported, has not been verified by a physician, and should not be deemed medically definitive. No Yes No Yes General Ever caused SERIOUS injury to others, caused MAJOR Illness or injury requiring hospitalization (including psychiatric) property damage or had trouble with the law because of Cardiology medical condition, mental disorder, or influence of alcohol or drugs Angina pectoris Hypertension (high blood pressure) Obstetrics and Sexually Transmitted Diseases Pregnancy Fundal height cm Cardiac arrhythmia Last menstrual period Date (mm-dd-yyyy) Congenital heart disease Sexually transmitted diseases, specify Pulmonology History of tobacco use Current useYes No Endocrinology and Hematology Asthma Diabetes mellitus Chronic obstructive pulmonary disease (emphysema) Thyroid disease History of tuberculosis (TB) disease History of malaria Treated Yes No Other Current TB symptoms Yes No Malignancy, specify Neurology and Psychiatry Chronic renal disease History of stroke, with current impairment Chronic hepatitis or other chronic liver disease Seizure disorder Hansen's Disease