Clostridium Perfringens
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Official Nh Dhhs Health Alert
THIS IS AN OFFICIAL NH DHHS HEALTH ALERT Distributed by the NH Health Alert Network [email protected] May 18, 2018, 1300 EDT (1:00 PM EDT) NH-HAN 20180518 Tickborne Diseases in New Hampshire Key Points and Recommendations: 1. Blacklegged ticks transmit at least five different infections in New Hampshire (NH): Lyme disease, Anaplasma, Babesia, Powassan virus, and Borrelia miyamotoi. 2. NH has one of the highest rates of Lyme disease in the nation, and 50-60% of blacklegged ticks sampled from across NH have been found to be infected with Borrelia burgdorferi, the bacterium that causes Lyme disease. 3. NH has experienced a significant increase in human cases of anaplasmosis, with cases more than doubling from 2016 to 2017. The reason for the increase is unknown at this time. 4. The number of new cases of babesiosis also increased in 2017; because Babesia can be transmitted through blood transfusions in addition to tick bites, providers should ask patients with suspected babesiosis whether they have donated blood or received a blood transfusion. 5. Powassan is a newer tickborne disease which has been identified in three NH residents during past seasons in 2013, 2016 and 2017. While uncommon, Powassan can cause a debilitating neurological illness, so providers should maintain an index of suspicion for patients presenting with an unexplained meningoencephalitis. 6. Borrelia miyamotoi infection usually presents with a nonspecific febrile illness similar to other tickborne diseases like anaplasmosis, and has recently been identified in one NH resident. Tests for Lyme disease do not reliably detect Borrelia miyamotoi, so providers should consider specific testing for Borrelia miyamotoi (see Attachment 1) and other pathogens if testing for Lyme disease is negative but a tickborne disease is still suspected. -

Evaluating Compliance with the Produce Safety Rule and Managing Mycotoxins
Walden University ScholarWorks Walden Dissertations and Doctoral Studies Walden Dissertations and Doctoral Studies Collection 2021 Evaluating Compliance with the Produce Safety Rule and Managing Mycotoxins Yvette May Molajo Walden University Follow this and additional works at: https://scholarworks.waldenu.edu/dissertations Part of the Public Administration Commons, and the Public Policy Commons This Dissertation is brought to you for free and open access by the Walden Dissertations and Doctoral Studies Collection at ScholarWorks. It has been accepted for inclusion in Walden Dissertations and Doctoral Studies by an authorized administrator of ScholarWorks. For more information, please contact [email protected]. Walden University College of Social and Behavioral Sciences This is to certify that the doctoral dissertation by Yvette Molajo has been found to be complete and satisfactory in all respects, and that any and all revisions required by the review committee have been made. Review Committee Dr. Marcia A. Kessack, Committee Chairperson, Public Policy and Administration Faculty Dr. Asghar Zomorrodian, Committee Member, Public Policy and Administration Faculty Dr. Meena Clowes, University Reviewer, Public Policy and Administration Faculty Chief Academic Officer and Provost Sue Subocz, Ph.D. Walden University 2021 Abstract Evaluating Compliance with the Produce Safety Rule and Managing Mycotoxins by Yvette Molajo MA, Walden University, 2020 MPA, Nova Southeastern University, 2014 BS, University of Maryland, College Park, 2012 Dissertation Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy Public Policy and Administration Walden University August 2021 Abstract Foodborne diseases are the cause of many illnesses that occur from foods that contain mycotoxins. Mycotoxins are produced from fungi and are environmental and carcinogenic agents that contaminate agricultural foods during preharvest and postharvest conditions. -

Feed Safety 2016
Annual Report The surveillance programme for feed materials, complete and complementary feed in Norway 2016 - Mycotoxins, fungi and bacteria NORWEGIAN VETERINARY INSTITUTE The surveillance programme for feed materials, complete and complementary feed in Norway 2016 – Mycotoxins, fungi and bacteria Content Summary ...................................................................................................................... 3 Introduction .................................................................................................................. 4 Aims ........................................................................................................................... 5 Materials and methods ..................................................................................................... 5 Quantitative determination of total mould, Fusarium and storage fungi ........................................ 6 Chemical analysis .......................................................................................................... 6 Bacterial analysis .......................................................................................................... 7 Statistical analysis ......................................................................................................... 7 Results and discussion ...................................................................................................... 7 Cereals ..................................................................................................................... -

Human Illness Caused by E. Coli O157:H7 from Food and Non-Food Sources
FRI BRIEFINGS Human Illness Caused by E. coli O157:H7 from Food and Non-food Sources M. Ellin Doyle1*, John Archer2, Charles W. Kaspar1, and Ronald Weiss1 1Food Research Institute, University of Wisconsin–Madison, Madison, WI 53706 2Wisconsin Division of Public Health, Bureau of Communicable Diseases and Preparedness, Communicable Disease Epidemiology Section, Madison, WI 53702 Contents Introduction ...................................................................................................................................2 Epidemiology of E. coli O157:H7..................................................................................................2 Outbreak Data ........................................................................................................................2 Reservoirs of E. coli O157:H7 ..............................................................................................3 Cattle—the primary reservoir ........................................................................................3 Other ruminants .............................................................................................................4 Other animals .................................................................................................................4 Transport Hosts......................................................................................................................4 Routes of Human Infection ....................................................................................................5 -

E. Coli “The Big Six”1 Bruna Bertoldi, Susanna Richardson, Renée Goodrich Schneider, Ploy Kurdmongkoltham, and Keith R
FSHN13-09 Preventing Foodborne Illness: E. coli “The Big Six”1 Bruna Bertoldi, Susanna Richardson, Renée Goodrich Schneider, Ploy Kurdmongkoltham, and Keith R. Schneider2 This is one in a series of fact sheets discussing common can contain pathogens like E. coli O157:H7, it is important foodborne pathogens of interest to food handlers, processors, to thoroughly wash anything that becomes contaminated, and retailers. For the rest of the series, visit http://edis.ifas. such as food and food contact surfaces (Armstrong et al. ufl.edu/topic_foodborne_illness. 1996; Tuttle et al. 1999). What type of bacterium is E. coli? E. coli are Gram-negative, rod-shaped bacteria. Some pathogenic strains have been variously described as verotoxigenic E. coli (VTEC) or Shiga-like toxin-producing E. coli (SLTEC). Most recently, the designation has been simplified to Shiga toxin-producing E. coli (STEC) in recognition of the similarities of the toxins produced by E. coli and Shigella dysenteriae (Fischer Walker et al. 2012; Murray et al. 2007). Such potent toxins can cause severe damage to the intestinal lining, even in healthy individuals. E. coli-produced toxins are responsible for symptoms such as hemorrhagic colitis. Hemorrhagic colitis is associated Figure 1. E. coli bacterium. Credits: iStock with bloody diarrhea and hemolytic uremic syndrome What is E. coli? (HUS), which is seen in the very young and can cause renal failure and hemolytic anemia. Both illnesses can be harmful Escherichia coli (E. coli) is a bacterium from the family and, in very severe cases, can lead to death (Murray et al. Enterobacteriaceae. It is usually found in the digestive 2007; FDA 2015). -

Naeglaria and Brain Infections
Can bacteria shrink tumors? Cancer Therapy: The Microbial Approach n this age of advanced injected live Streptococcus medical science and into cancer patients but after I technology, we still the recipients unfortunately continue to hunt for died from subsequent innovative cancer therapies infections, Coley decided to that prove effective and safe. use heat killed bacteria. He Treatments that successfully made a mixture of two heat- eradicate tumors while at the killed bacterial species, By Alan Barajas same time cause as little Streptococcus pyogenes and damage as possible to normal Serratia marcescens. This Alani Barajas is a Research and tissue are the ultimate goal, concoction was termed Development Technician at Hardy but are also not easy to find. “Coley’s toxins.” Bacteria Diagnostics. She earned her bachelor's degree in Microbiology at were either injected into Cal Poly, San Luis Obispo. The use of microorganisms in tumors or into the cancer therapy is not a new bloodstream. During her studies at Cal Poly, much idea but it is currently a of her time was spent as part of the undergraduate research team for the buzzing topic in cancer Cal Poly Dairy Products Technology therapy research. Center studying spore-forming bacteria in dairy products. In the late 1800s, German Currently she is working on new physicians W. Busch and F. chromogenic media formulations for Fehleisen both individually Hardy Diagnostics, both in the observed that certain cancers prepared and powdered forms. began to regress when patients acquired accidental erysipelas (cellulitis) caused by Streptococcus pyogenes. William Coley was the first to use New York surgeon William bacterial injections to treat cancer www.HardyDiagnostics.com patients. -
Diagnostic Code Descriptions (ICD9)
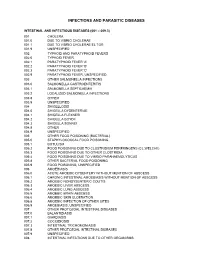
INFECTIONS AND PARASITIC DISEASES INTESTINAL AND INFECTIOUS DISEASES (001 – 009.3) 001 CHOLERA 001.0 DUE TO VIBRIO CHOLERAE 001.1 DUE TO VIBRIO CHOLERAE EL TOR 001.9 UNSPECIFIED 002 TYPHOID AND PARATYPHOID FEVERS 002.0 TYPHOID FEVER 002.1 PARATYPHOID FEVER 'A' 002.2 PARATYPHOID FEVER 'B' 002.3 PARATYPHOID FEVER 'C' 002.9 PARATYPHOID FEVER, UNSPECIFIED 003 OTHER SALMONELLA INFECTIONS 003.0 SALMONELLA GASTROENTERITIS 003.1 SALMONELLA SEPTICAEMIA 003.2 LOCALIZED SALMONELLA INFECTIONS 003.8 OTHER 003.9 UNSPECIFIED 004 SHIGELLOSIS 004.0 SHIGELLA DYSENTERIAE 004.1 SHIGELLA FLEXNERI 004.2 SHIGELLA BOYDII 004.3 SHIGELLA SONNEI 004.8 OTHER 004.9 UNSPECIFIED 005 OTHER FOOD POISONING (BACTERIAL) 005.0 STAPHYLOCOCCAL FOOD POISONING 005.1 BOTULISM 005.2 FOOD POISONING DUE TO CLOSTRIDIUM PERFRINGENS (CL.WELCHII) 005.3 FOOD POISONING DUE TO OTHER CLOSTRIDIA 005.4 FOOD POISONING DUE TO VIBRIO PARAHAEMOLYTICUS 005.8 OTHER BACTERIAL FOOD POISONING 005.9 FOOD POISONING, UNSPECIFIED 006 AMOEBIASIS 006.0 ACUTE AMOEBIC DYSENTERY WITHOUT MENTION OF ABSCESS 006.1 CHRONIC INTESTINAL AMOEBIASIS WITHOUT MENTION OF ABSCESS 006.2 AMOEBIC NONDYSENTERIC COLITIS 006.3 AMOEBIC LIVER ABSCESS 006.4 AMOEBIC LUNG ABSCESS 006.5 AMOEBIC BRAIN ABSCESS 006.6 AMOEBIC SKIN ULCERATION 006.8 AMOEBIC INFECTION OF OTHER SITES 006.9 AMOEBIASIS, UNSPECIFIED 007 OTHER PROTOZOAL INTESTINAL DISEASES 007.0 BALANTIDIASIS 007.1 GIARDIASIS 007.2 COCCIDIOSIS 007.3 INTESTINAL TRICHOMONIASIS 007.8 OTHER PROTOZOAL INTESTINAL DISEASES 007.9 UNSPECIFIED 008 INTESTINAL INFECTIONS DUE TO OTHER ORGANISMS -

Clostridium Perfringens
CLOSTRIDIUM PERFRINGENS: SPORES & CELLS MEDIA & MODELING Promotor: prof. dr. ir. Frans M. Rombouts Hoogleraar in de levensmiddelenhygiëne en –microbiologie Co-promotor: dr. Rijkelt R. Beumer Universitair docent Leerstoelgroep levensmiddelenmicrobiologie Promotiecommissie: prof. dr. ir. Johan M. Debevere (Universiteit Gent, België) dr. ir. Servé H.W. Notermans (TNO Voeding, Zeist) prof. dr. Michael W. Peck (Institute of Food Research, Norwich, UK) prof. dr. ir. Marcel H. Zwietering (Wageningen Universiteit) CLOSTRIDIUM PERFRINGENS: SPORES & CELLS MEDIA & MODELING Aarieke Eva Irene de Jong Proefschrift ter verkrijging van de graad van doctor op gezag van de rector magnificus van Wageningen Universiteit, prof. dr. ir. L. Speelman, in het openbaar te verdedigen op dinsdag 21 oktober 2003 des namiddags te vier uur in de Aula A.E.I. de Jong – Clostridium perfringens: spores & cells, media & modeling – 2003 Thesis Wageningen University, Wageningen, The Netherlands – With summary in Dutch ISBN 90-5808-931-2 ABSTRACT Clostridium perfringens is one of the five major food borne pathogens in the western world (expressed in cases per year). Symptoms are caused by an enterotoxin, for which 6% of type A strains carry the structural gene. This enterotoxin is released when ingested cells sporulate in the small intestine. Research on C. perfringens has been limited to a couple of strains that sporulate well in Duncan and Strong (DS) medium. These abundantly sporulating strains in vitro are not necessarily a representation of the most dangerous strains in vivo. Therefore, sporulation was optimized for C. perfringens strains in general. None of the tested media and methods performed well for all strains, but Peptone-Bile- Theophylline medium (with and without starch) yielded highest spore numbers. -
![CDC and Food Safety Fact Sheet. Pdf Icon[PDF – 2 Pages]](https://docslib.b-cdn.net/cover/9203/cdc-and-food-safety-fact-sheet-pdf-icon-pdf-2-pages-249203.webp)
CDC and Food Safety Fact Sheet. Pdf Icon[PDF – 2 Pages]
CDC and Food Safety Foodborne illness is common, costly, and preventable. CDC estimates that each year 1 in 6 Americans USDA estimates that foodborne illnesses cost the get sick from contaminated food or beverages and United States more than $15.6 billion a year. 3,000 die from foodborne illness. CDC provides the vital link between foodborne illness and the food safety systems of government agencies and food producers. CDC helps make food safer by: Working with partners to determine the major sources of foodborne illnesses and number of illnesses, investigate multistate foodborne disease outbreaks, and implement systems to prevent illnesses and detect and stop outbreaks. Government partners include state and local health departments, the U.S. Food and Drug Administration (FDA), and the U.S. Department of Agriculture’s (USDA) Food Safety and Inspection Service. The food industry, animal health partners, and consumers also play essential roles. Helping state and local health departments improve the tracking and investigation of foodborne illnesses and outbreaks through surveillance systems such as PulseNet, the System for Enteric Disease Response, Investigation, and Coordination (SEDRIC), and other programs. Using data to determine whether prevention measures are working and where further efforts and additional targets for prevention are needed to reduce foodborne illness. Working with other countries and international agencies to improve tracking, investigation, and prevention of foodborne infections in the United States and around the world. Using Advanced Technology to Find Outbreaks Whole genome sequencing (WGS) is a tool used to generate a DNA “fingerprint.” CDC scientists and partners use WGS data to determine if strains of bacteria have similar DNA fingerprints, which could mean they come from the same source—for example, the same food or processing facility. -

CDC Estimates of Foodborne Illness in the United States
CDC Estimates of Foodborne Illness FINDINGS in the United States CDC 2011 Estimates CDC estimates that each year roughly 1 out of 6 Americans (or 48 million people) get sick, 128,000 are hospitalized, and 3,000 Reducing foodborne die of foodborne diseases. The 2011 estimates provide the most illness by 10% would accurate picture yet of which foodborne bacteria, viruses, microbes (“pathogens”) are causing the most illnesses in the United States, keep about 5 million as well as estimating the number of foodborne illnesses without a Americans from known cause.* The estimates show that there is still much work to be done—specifically in focusing efforts on the top known pathogens getting sick each year. and identifying the causes of foodborne illness and death without a known cause. CDC has estimates for two major groups of foodborne illnesses: Known foodborne pathogens— 31 pathogens known to cause foodborne illness. Many of these pathogens are tracked by public health systems that track diseases and outbreaks. *Unspecified agents— Agents with insufficient data to estimate agent-specific burden; known agents not yet identified as causing foodborne illness; microbes, chemicals, or other substances known to be in food whose ability to cause illness is unproven; and agents not yet identified. Because you can’t “track” what isn’t yet identified, estimates for this group of agents started with the health effects or symptoms that they are most likely to cause— acute gastroenteritis. To estimate the total number of foodborne illnesses, CDC estimated the number of illnesses caused by both known and unspecified agents. We also estimated the number of hospitalizations and deaths caused by these illnesses. -

Establishment of Listeria Monocytogenes in the Gastrointestinal Tract
microorganisms Review Establishment of Listeria monocytogenes in the Gastrointestinal Tract Morgan L. Davis 1, Steven C. Ricke 1 and Janet R. Donaldson 2,* 1 Center for Food Safety, Department of Food Science, University of Arkansas, Fayetteville, AR 72704, USA; [email protected] (M.L.D.); [email protected] (S.C.R.) 2 Department of Cell and Molecular Biology, The University of Southern Mississippi, Hattiesburg, MS 39406, USA * Correspondence: [email protected]; Tel.: +1-601-266-6795 Received: 5 February 2019; Accepted: 5 March 2019; Published: 10 March 2019 Abstract: Listeria monocytogenes is a Gram positive foodborne pathogen that can colonize the gastrointestinal tract of a number of hosts, including humans. These environments contain numerous stressors such as bile, low oxygen and acidic pH, which may impact the level of colonization and persistence of this organism within the GI tract. The ability of L. monocytogenes to establish infections and colonize the gastrointestinal tract is directly related to its ability to overcome these stressors, which is mediated by the efficient expression of several stress response mechanisms during its passage. This review will focus upon how and when this occurs and how this impacts the outcome of foodborne disease. Keywords: bile; Listeria; oxygen availability; pathogenic potential; gastrointestinal tract 1. Introduction Foodborne pathogens account for nearly 6.5 to 33 million illnesses and 9000 deaths each year in the United States [1]. There are over 40 pathogens that can cause foodborne disease. The six most common foodborne pathogens are Salmonella, Campylobacter jejuni, Escherichia coli O157:H7, Listeria monocytogenes, Staphylococcus aureus, and Clostridium perfringens. -

615.9Barref.Pdf
INDEX Abortifacient, abortifacients bees, wasps, and ants ginkgo, 492 aconite, 737 epinephrine, 963 ginseng, 500 barbados nut, 829 blister beetles goldenseal blister beetles, 972 cantharidin, 974 berberine, 506 blue cohosh, 395 buckeye hawthorn, 512 camphor, 407, 408 ~-escin, 884 hypericum extract, 602-603 cantharides, 974 calamus inky cap and coprine toxicity cantharidin, 974 ~-asarone, 405 coprine, 295 colocynth, 443 camphor, 409-411 ethanol, 296 common oleander, 847, 850 cascara, 416-417 isoxazole-containing mushrooms dogbane, 849-850 catechols, 682 and pantherina syndrome, mistletoe, 794 castor bean 298-302 nutmeg, 67 ricin, 719, 721 jequirity bean and abrin, oduvan, 755 colchicine, 694-896, 698 730-731 pennyroyal, 563-565 clostridium perfringens, 115 jellyfish, 1088 pine thistle, 515 comfrey and other pyrrolizidine Jimsonweed and other belladonna rue, 579 containing plants alkaloids, 779, 781 slangkop, Burke's, red, Transvaal, pyrrolizidine alkaloids, 453 jin bu huan and 857 cyanogenic foods tetrahydropalmatine, 519 tansy, 614 amygdalin, 48 kaffir lily turpentine, 667 cyanogenic glycosides, 45 lycorine,711 yarrow, 624-625 prunasin, 48 kava, 528 yellow bird-of-paradise, 749 daffodils and other emetic bulbs Laetrile", 763 yellow oleander, 854 galanthamine, 704 lavender, 534 yew, 899 dogbane family and cardenolides licorice Abrin,729-731 common oleander, 849 glycyrrhetinic acid, 540 camphor yellow oleander, 855-856 limonene, 639 cinnamomin, 409 domoic acid, 214 rna huang ricin, 409, 723, 730 ephedra alkaloids, 547 ephedra alkaloids, 548 Absorption, xvii erythrosine, 29 ephedrine, 547, 549 aloe vera, 380 garlic mayapple amatoxin-containing mushrooms S-allyl cysteine, 473 podophyllotoxin, 789 amatoxin poisoning, 273-275, gastrointestinal viruses milk thistle 279 viral gastroenteritis, 205 silibinin, 555 aspartame, 24 ginger, 485 mistletoe, 793 Medical Toxicology ofNatural Substances, by Donald G.