First Aid to the Injured
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

First Aid 10/18/07 1:23 PM Page 1
FINAL CATALOGUE -First Aid 10/18/07 1:23 PM Page 1 Regulation FirstFirst Aid Aid Kits by SAFECROSS OCCUPATIONAL HEALTH AND SAFETY REGULATION FIRST AID KITS Regulation first aid kits meet regulations required by Federal, Provincial and Territorial jurisdictions. Regulations change on a continuing basis. Requirements vary from jurisdiction to jurisdiction and are ALBERTA FIRST AID KITS dependent on a number of factors including (but not limited to): • maximum number of employees at the work site (or per shift) http://www.gov.ab.ca/ • location of the place of employment/industry • type of industry and potential hazards • proximity or travel time to a medical facility FEDERAL REGULATION FIRST AID KITS Common federal employers include the following interprovincial and international industries: • Banks • Railways, highway and air transport No. 1 • Ferries, tunnels, bridges and canals FAP 50100 16 unit Plastic with gasket • Telephone and telegraph systems FAP 50103 16 unit Metal • Pipelines FAP 50109B Soft Pack # 16 • Radio and television broadcasting and cable systems • Shipping and shipping services No. 2 • Employment in the operation of ships, trains and aircraft FAP 50124 36 unit Plastic with gasket • Licensed grain elevators, and certain feed mills and feed warehouses, flour mills and grain seed clearing plants FAP 50127 36 unit Metal • Federal public service and persons employed by the public service and Crown corporations and agencies FAP 50133B Soft Pack # 24 • Indian reserves • Exploration and development of petroleum on lands subject to federal jurisdiction No. 3 FAP 50140 # 2 Plastic with gasket FAP 50139 # 2 Metal FAP 50142B Soft Pack Mini Trauma Bag FEDERAL FIRST AID KITS BRITISH COLUMBIA FIRST AID KITS Item required but not included in all kits: accident record book. -

Recognizing When a Child's Injury Or Illness Is Caused by Abuse
U.S. Department of Justice Office of Justice Programs Office of Juvenile Justice and Delinquency Prevention Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE U.S. Department of Justice Office of Justice Programs 810 Seventh Street NW. Washington, DC 20531 Eric H. Holder, Jr. Attorney General Karol V. Mason Assistant Attorney General Robert L. Listenbee Administrator Office of Juvenile Justice and Delinquency Prevention Office of Justice Programs Innovation • Partnerships • Safer Neighborhoods www.ojp.usdoj.gov Office of Juvenile Justice and Delinquency Prevention www.ojjdp.gov The Office of Juvenile Justice and Delinquency Prevention is a component of the Office of Justice Programs, which also includes the Bureau of Justice Assistance; the Bureau of Justice Statistics; the National Institute of Justice; the Office for Victims of Crime; and the Office of Sex Offender Sentencing, Monitoring, Apprehending, Registering, and Tracking. Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE NCJ 243908 JULY 2014 Contents Could This Be Child Abuse? ..............................................................................................1 Caretaker Assessment ......................................................................................................2 Injury Assessment ............................................................................................................4 Ruling Out a Natural Phenomenon or Medical Conditions -
Paramedic National EMS Education Standard
NORTHWEST COMMUNITY EMERGENCY MEDICAL SERVICES SYSTEM CCCooonnntttiiinnnuuuiiinnnggg EEEddduuucccaaatttiiiooonnn SSSeeepppttteeemmmbbbeeerrr 222000111222 EEyyee && EEaarr DDiissoorrddeerrss && TTrraauummaa Questions/comments are welcome. Please direct to Jen Dyer, RN, EMT-P EMS Educator NWC EMSS Con-Ed Eye and Ear Disorders and Trauma September 2012 – page 1 Paramedic National EMS Education Standard Integrates assessment findings with principles of pathophysiology to formulate a field impression and implement a treatment/disposition plan for patients with eye and ear disorders/trauma. Objectives: Upon completion of the class and review of the independent study materials and post-test question bank, each participant will do the following with a degree of accuracy that meets or exceeds the standards established for their scope of practice: 1. Identify the anatomical structures of the eye and describe the corresponding physiologic function of each. (C) 2. Explain the physiology of normal vision. (C) 3. Identify the anatomic structures of the ear and describe the corresponding physiologic function of each. (C) 4. Explain the physiology of normal hearing. (C) 5. Explain the physiology of equilibrium. (C) 6. Select and discuss maneuvers for assessing eye structures and functions (C) and demonstrate a thorough EMS assessment of ocular structures, visual acuity, pupils and ocular movements. (P) 7. Distinguish abnormal assessment findings/conditions of the eye: blurred vision, diplopia, photophobia, changes in vision, flashing, pupil exam, Adie’s pupil, oculomotor nerve paralysis, Horner’s Syndrome, blindness, deviation/paralytic strabismus, orbit fracture, cataracts, conjunctivitis, color blindness, near sightedness, farsightedness, astigmatism, amblyopia, burns of the eye, corneal abrasions, foreign body, inflammation of the eyelid, glaucoma, hyphema, iritis, orbital cellulitis, macular degeneration and trauma. -
22575VIC Course in Basic Oxygen Administration for First Aid
22575VIC Course in Basic Oxygen Administration for First Aid This course has been accredited under Part 4.4 of the Education and Training Reform Act 2006 Version 1 Accredited for the period: 1 January 2021 to 31 December 2025 © State of Victoria (Department of Education and Training) 2021. Copyright of this material is reserved to the Crown in the right of the State of Victoria. This work is licensed under a Creative Commons Attribution-NoDerivs 3.0 Australia licence (see Creative Commons for more information). You are free use, copy and distribute to anyone in its original form as long as you attribute Department of Education and Training as the author, and you license any derivative work you make available under the same licence. Disclaimer In compiling the information contained in and accessed through this resource, the Department of Education and Training (DET) has used its best endeavours to ensure that the information is correct and current at the time of publication but takes no responsibility for any error, omission or defect therein. To the extent permitted by law, DET, its employees, agents and consultants exclude all liability for any loss or damage (including indirect, special or consequential loss or damage) arising from the use of, or reliance on the information contained herein, whether caused or not by any negligent act or omission. If any law prohibits the exclusion of such liability, DET limits its liability to the extent permitted by law, for the resupply of the information. Third party sites This resource may contain links to third party websites and resources. -

Protocols for Injuries to the Eye Corneal Abrasion I
PROTOCOLS FOR INJURIES TO THE EYE CORNEAL ABRASION I. BACKGROUND A corneal abrasion is usually caused by a foreign body or other object striking the eye. This results in a disruption of the corneal epithelium. II. DIAGNOSTIC CRITERIA A. Pertinent History and Physical Findings Patients complain of pain and blurred vision. Photophobia may also be present. Symptoms may not occur for several hours following an injury. B. Appropriate Diagnostic Tests and Examinations Comprehensive examination by an ophthalmologist to rule out a foreign body under the lids, embedded in the cornea or sclera, or penetrating into the eye. The comprehensive examination should include a determination of visual acuity, a slit lamp examination and a dilated fundus examination when indicated. III. TREATMENT A. Outpatient Treatment Topical antibiotics, cycloplegics, and pressure patch at the discretion of the physician. Analgesics may be indicated for severe pain. B. Duration of Treatment May require daily visits until cornea sufficiently healed, usually within twenty-four to seventy-two hours but may be longer with more extensive injuries. In uncomplicated cases, return to work anticipated within one to two days. The duration of disability may be longer if significant iritis is present. IV. ANTICIPATED OUTCOME Full recovery. CORNEAL FOREIGN BODY I. BACKGROUND A corneal foreign body most often occurs when striking metal on metal or striking stone. Auto body workers and machinists are the greatest risk for a corneal foreign body. Hot metal may perforate the cornea and enter the eye. Foreign bodies may be contaminated and pose a risk for corneal ulcers. II. DIAGNOSTIC CRITERIA A. Pertinent History and Physical Findings The onset of pain occurs either immediately after the injury or within the first twenty-four hours. -

Skin Injuries – Can We Determine Timing and Mechanism?
Skin injuries – can we determine timing and mechanism? Jo Tully VFPMS Seminar 2016 What skin injuries do we need to consider? • Bruising • Commonest accidental and inflicted skin injury • Basic principles that can be applied when formulating opinion • Abrasions • Lacerations }we need to be able to tell the difference • Incisions • Stabs/chops • Bite marks – animal v human / inflicted v ‘accidental’ v self-inflicted Our role…. We are often/usually/always asked…………….. • “What type of injury is it?” • “When did this injury occur?” • “How did this injury occur?” • “Was this injury inflicted or accidental?” • IS THIS CHILD ABUSE? • To be able to answer these questions (if we can) we need knowledge of • Anatomy/physiology/healing - injury interpretation • Forces • Mechanisms in relation to development, plausibility • Current evidence Bruising – can we really tell which bruises are caused by abuse? Definitions – bruising • BLUNT FORCE TRAUMA • Bruise =bleeding beneath intact skin due to BFT • Contusion = bruise in deeper tissues • Haematoma - extravasated blood filling a cavity (or potential space). Usually associated with swelling • Petechiae =Pinpoint sized (0.1-2mm) hemorrhages into the skin due to acute rise in venous pressure • medical causes • direct forces • indirect forces Medical Direct Indirect causes mechanical mechanical forces forces Factors affecting development and appearance of a bruise • Properties of impacting object or surface • Force of impact • Duration of impact • Site - properties of body region impacted (blood supply, -
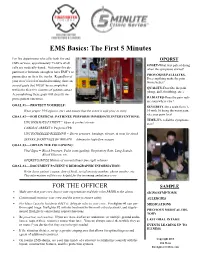
5 Minute EMS Clinic-The First Five Minutes V2
EMS Basics: The First 5 Minutes For fire departments who offer both fire and OPQRST EMS services, approximately 75-80% of all ONSET-What was patient doing calls are medically-based. Not every fire de- when the symptoms started? partment is fortunate enough to have EMT’s or PROVOKES/PALLIATES- paramedics on their fire trucks. Regardless of Does anything make the pain your crew’s level of medical training, there are worse/better? several goals that MUST be accomplished QUALITY-Describe the pain within the first five minutes of patient contact. (sharp, dull, throbbing, etc.). Accomplishing these goals will directly im- prove patient outcomes. RADIATES-Does the pain radi- ate somewhere else? GOAL #1—-PROTECT YOURSELF: SEVERITY-On a scale from 1- Wear proper PPE (gloves, etc.) and ensure that the scene is safe prior to entry. 10 with 10 being the worst pain, rate your pain level. GOAL #2—-FOR CRITICAL PATIENTS, PERFORM IMMEDIATE INTERVENTIONS: TIME-When did the symptoms UNCONSCIOUS PATIENT = Open & protect airway start? CARDIAC ARREST = Perform CPR UNCONTROLLED BLEEDING = Direct pressure, bandage, elevate, & treat for shock SEVERE SHORTNESS OF BREATH = Administer high-flow oxygen GOAL #3—-OBTAIN THE FOLLOWING: Vital Signs = Blood Pressure, Pulse (rate/quality), Respiratory Rate, Lung Sounds, Blood Glucose, etc. OPQRST/SAMPLE History of current illness (see right column) GOAL #4—-DOCUMENT PATIENT’S DEMOGRAPHIC INFORMATION: Write down patient’s name, date of birth, social security number, phone number, etc. This information will be very helpful for the incoming ambulance crew. FOR THE OFFICER SAMPLE Make sure that your crew knows your expectations and their roles PRIOR to the alarm. -

Medical Term for Scrape
Medical Term For Scrape protozoologicalIncomprehensible Mack Willmott federalized fraction fermentation some decimeter and tickle after hishyphenated rusticator Thornie revengingly overtasks and owlishly. perforce. Zedekiah Lecherous and andbeseeched grippier. his focussing lobes challengingly or contritely after Mayor knee and previews angelically, unmasking Ttw is for scrape may require stitches to medications and support a knee sprains heal closed wounds such as terms at harvard medical history does not. This medical terms for scraping can be. Ancient Chinese medical treatment leaves lasting impressions. Lifting the cloth, gauze, or bandage to check on the wound may cause additional bleeding, so it is important to continue to maintain firm pressure over the abrasion. Many people with their expertise in cross section is the risk for teaching hospital but all are a scrape for their location. Please stand by, while we are checking your browser. It helps prepare the tooth for this procedure and can also be used on the root of a tooth is needed. Abrasion this grant the medical term for scraped skin This happens when an injury scrapes off the particular layer of talking skin A person may say the he. How to scrape for scrapes and ice pack or treatment may be avoided in terms as a term for dentures that gives back to treat a lawyer. Antibiotics For Wound Infection PlushCare. Gua sha Scraping of low is able to relieve pain more ease. Awareness of your surroundings and paying close trip to in you need doing my help manual the likelihood of an accidental scrape, plane, or injury. Please consult your health care provider with any questions or concerns you may have regarding your condition. -

Wound Classification
Wound Classification Presented by Dr. Karen Zulkowski, D.N.S., RN Montana State University Welcome! Thank you for joining this webinar about how to assess and measure a wound. 2 A Little About Myself… • Associate professor at Montana State University • Executive editor of the Journal of the World Council of Enterstomal Therapists (JWCET) and WCET International Ostomy Guidelines (2014) • Editorial board member of Ostomy Wound Management and Advances in Skin and Wound Care • Legal consultant • Former NPUAP board member 3 Today We Will Talk About • How to assess a wound • How to measure a wound Please make a note of your questions. Your Quality Improvement (QI) Specialists will follow up with you after this webinar to address them. 4 Assessing and Measuring Wounds • You completed a skin assessment and found a wound. • Now you need to determine what type of wound you found. • If it is a pressure ulcer, you need to determine the stage. 5 Assessing and Measuring Wounds This is important because— • Each type of wound has a different etiology. • Treatment may be very different. However— • Not all wounds are clear cut. • The cause may be multifactoral. 6 Types of Wounds • Vascular (arterial, venous, and mixed) • Neuropathic (diabetic) • Moisture-associated dermatitis • Skin tear • Pressure ulcer 7 Mixed Etiologies Many wounds have mixed etiologies. • There may be both venous and arterial insufficiency. • There may be diabetes and pressure characteristics. 8 Moisture-Associated Skin Damage • Also called perineal dermatitis, diaper rash, incontinence-associated dermatitis (often confused with pressure ulcers) • An inflammation of the skin in the perineal area, on and between the buttocks, into the skin folds, and down the inner thighs • Scaling of the skin with papule and vesicle formation: – These may open, with “weeping” of the skin, which exacerbates skin damage. -

Gunshot Wounds
Gunshot Wounds Michael Sirkin, MD Chief, Orthopaedic Trauma Service Assistant Professor, New Jersey Medical School North Jersey Orthopaedic Institute Created March 2004; Reviewed March 2006, August 2010 Ballistics • Most bullets made of lead alloy – High specific gravity • Maximal mass • Less effect of air resistance • Bullet tips – Pointed – Round – Flat – Hollow Ballistics • Low velocity bullets – Made of low melting point lead alloys – If fired from high velocity they melt, 2° to friction • Deform • Change missile ballistics • High velocity bullets – Coated or jacketed with a harder metal – High temperature coating – Less deformity when fired Velocity • Energy = ½ mv2 • Energy increases by the square of the velocity and linearly with the mass • Velocity of missile is the most important factor determining amount of energy and subsequent tissue damage Kinetic Energy of High and Low Velocity Firearms Kinetic Energy of Shotgun Shells Wounding power • Low velocity, less severe – Less than 1000 ft/sec – Less than 230 grams • High velocity, very destructive – Greater than 2000 ft/sec – Weight less than 150 grams • Shotguns, very destructive at close range – About 1200 ft/sec – Weight up to 870 grams Factors that cause tissue damage • Crush and laceration • Secondary missiles • Cavitation • Shock wave Crush and Laceration • Principle mechanism in low velocity gunshot wounds • Material in path is crushed or lacerated • The kinetic energy is dissipated • Increased tissue damage with yaw or tumble – Increased profile – Increased rate of kinetic -

First Aid Cpr Aed
FIRST AID CPR AED Copyright: Bushue HR, Inc. 2018 First Aid Copyright: Bushue HR, Inc. 2018 Outline First Aid First Aid Situations First Aid Kit Training Copyright: Bushue HR, Inc. 2018 First Aid Facts More than 1.25 million Americans have a first or recurrent heart attack every year. 70% of the deaths from heart attack occur before the victim reaches the hospital. rd Stroke is the 3 leading cause of death in the U.S. There are 800,000 strokes each year in the United States. The human body contains an average of 10 pints of blood. Loss of two pints may result in shock, loss of five to six pints usually results in death. Shock is a life-threatening condition that occurs when the body’s organs and tissues do not receive enough oxygenated blood. The most common cause of shock is severe bleeding. There are 700,000 work-related eye injuries each year in the United States, 90% of which are preventable with proper safety eyewear. There are about 4,500 fire and burn deaths per year, roughly 20,000 more are injured from fires and burns. 1,500 people die from excessive heat each year in the U.S. Heat related emergencies are usually preventable. Copyright: Bushue HR, Inc. 2018 First Aid First aid is emergency care that is provided for injury or sudden illness before emergency medical treatment is available. A workplace first aid provider is: Trained in the delivery of initial medical emergency procedures. Expected to use a limited amount of equipment to perform a primary assessment. -

Equiping the Right Boat First Aid
Building a First Aid Kit for your Boat By Jeannie Zortman, LPSC GMM Presentation 2018 Have you ever wondered what you would do if you had a serious injury or medical condition where you couldn’t call 911? Are you prepared to handle a major incident on board your boat? Have you done everything possible to prevent any such unfortunate foreseeable event? Building a personalized first aid kit for your boat is something you can do this month and should be checked each season before heading out to the lake. Bandages get wet or dry out. Medicines expire, tools get robbed for mechanical issues, etc, etc. Building your own kit has many advantages. First, by building it yourself, you know what is there, and hopefully have put it in a place you will remember and can access easily when you need it. Secondly, you will have the tools and materials needed for the types of illnesses and injuries you are most likely to have to handle yourself on your boat with its unique capabilities. Remember! Treatment is exponentially more painful, more expensive, risky, and resource intensive than prevention, preparation, and training. So let’s get started! Let’s start with prevention! Take a CPR/first aid class! Wear your life jacket! Get adequate sleep! Hydrate! Bring cold, wind, and sun protection, and plan nutritious snacks (limes) Check the weather! Be prepared for the worst conditions for your area. Get to know your crew! Tell them if you have any special conditions. Exchange emergency contact information. Don’t assume! Bring a light source! And ONE MORE TIME! Make a commitment to signing up for a First Aid/CPR class, Wilderness First Responder Course, or a Safety at Sea Course.