Review of Systems Gastrointestinal Tract
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome
MEDICAL POLICY – 2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome BCBSA Ref. Policy: 2.04.26 Effective Date: July 1, 2021 RELATED MEDICAL POLICIES: Last Revised: June 8, 2021 None Replaces: N/A Select a hyperlink below to be directed to that section. POLICY CRITERIA | DOCUMENTATION REQUIREMENTS | CODING RELATED INFORMATION | EVIDENCE REVIEW | REFERENCES | HISTORY ∞ Clicking this icon returns you to the hyperlinks menu above. Introduction Intestinal dysbiosis is a condition that occurs when the microorganisms in the digestive tract are out of balance. This condition is believed to cause diseases of the digestive tract, including poor nutrient absorption, overgrowth of certain bacteria, and irritable bowel syndrome (IBS). Symptoms of these digestive problems are similar and may include: abdominal pain, excess gas, bloating, and changes in bowel movements (constipation or diarrhea, or both). One method of diagnosing digestive disorders is by testing a fecal sample. Using fecal analysis to diagnose intestinal dysbiosis, IBS, malabsorption, or small intestinal overgrowth of bacteria is unproven (investigational). More studies are needed to see if this testing improves health outcomes. Note: The Introduction section is for your general knowledge and is not to be taken as policy coverage criteria. The rest of the policy uses specific words and concepts familiar to medical professionals. It is intended for providers. A provider can be a person, such as a doctor, nurse, psychologist, or dentist. A provider also can be a place where medical care is given, like a hospital, clinic, or lab. This policy informs them about when a service may be covered. -

Review of Systems
code: GF004 REVIEW OF SYSTEMS First Name Middle Name / MI Last Name Check the box if you are currently experiencing any of the following : General Skin Respiratory Arthritis/Rheumatism Abnormal Pigmentation Any Lung Troubles Back Pain (recurrent) Boils Asthma or Wheezing Bone Fracture Brittle Nails Bronchitis Cancer Dry Skin Chronic or Frequent Cough Diabetes Eczema Difficulty Breathing Foot Pain Frequent infections Pleurisy or Pneumonia Gout Hair/Nail changes Spitting up Blood Headaches/Migraines Hives Trouble Breathing Joint Injury Itching URI (Cold) Now Memory Loss Jaundice None Muscle Weakness Psoriasis Numbness/Tingling Rash Obesity Skin Disease Osteoporosis None Rheumatic Fever Weight Gain/Loss None Cardiovascular Gastrointestinal Eyes - Ears - Nose - Throat/Mouth Awakening in the night smothering Abdominal Pain Blurring Chest Pain or Angina Appetite Changes Double Vision Congestive Heart Failure Black Stools Eye Disease or Injury Cyanosis (blue skin) Bleeding with Bowel Movements Eye Pain/Discharge Difficulty walking two blocks Blood in Vomit Glasses Edema/Swelling of Hands, Feet or Ankles Chrohn’s Disease/Colitis Glaucoma Heart Attacks Constipation Itchy Eyes Heart Murmur Cramping or pain in the Abdomen Vision changes Heart Trouble Difficulty Swallowing Ear Disease High Blood Pressure Diverticulosis Ear Infections Irregular Heartbeat Frequent Diarrhea Ears ringing Pain in legs Gallbladder Disease Hearing problems Palpitations Gas/Bloating Impaired Hearing Poor Circulation Heartburn or Indigestion Chronic Sinus Trouble Shortness -

Review of Systems – Return Visit Have You Had Any Problems Related to the Following Symptoms in the Past Month? Circle Yes Or No
REVIEW OF SYSTEMS – RETURN VISIT HAVE YOU HAD ANY PROBLEMS RELATED TO THE FOLLOWING SYMPTOMS IN THE PAST MONTH? CIRCLE YES OR NO Today’s Date: ______________ Name: _______________________________ Date of Birth: __________________ GENERAL GENITOURINARY Fatigue Y N Blood in Urine Y N Fever / Chills Y N Menstrual Irregularity Y N Night Sweats Y N Painful Menstrual Cycle Y N Weight Gain Y N Vaginal Discharge Y N Weight Loss Y N Vaginal Dryness Y N EYES Vaginal Itching Y N Vision Changes Y N Painful Sex Y N EAR, NOSE, & THROAT SKIN Hearing Loss Y N Hair Loss Y N Runny Nose Y N New Skin Lesions Y N Ringing in Ears Y N Rash Y N Sinus Problem Y N Pigmentation Change Y N Sore Throat Y N NEUROLOGIC BREAST Headache Y N Breast Lump Y N Muscular Weakness Y N Tenderness Y N Tingling or Numbness Y N Nipple Discharge Y N Memory Difficulties Y N CARDIOVASCULAR MUSCULOSKELETAL Chest Pain Y N Back Pain Y N Swelling in Legs Y N Limitation of Motion Y N Palpitations Y N Joint Pain Y N Fainting Y N Muscle Pain Y N Irregular Heart Beat Y N ENDOCRINE RESPIRATORY Cold Intolerance Y N Cough Y N Heat Intolerance Y N Shortness of Breath Y N Excessive Thirst Y N Post Nasal Drip Y N Excessive Amount of Urine Y N Wheezing Y N PSYCHOLOGY GASTROINTESTINAL Difficulty Sleeping Y N Abdominal Pain Y N Depression Y N Constipation Y N Anxiety Y N Diarrhea Y N Suicidal Thoughts Y N Hemorrhoids Y N HEMATOLOGIC / LYMPHATIC Nausea Y N Easy Bruising Y N Vomiting Y N Easy Bleeding Y N GENITOURINARY Swollen Lymph Glands Y N Burning with Urination Y N ALLERGY / IMMUNOLOGY Urinary -
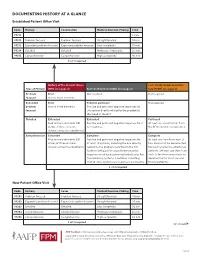
Documenting History at a Glance
DOCUMENTING HISTORY AT A GLANCE Established Patient Office Visit Code History Examination Medical Decision-Making Time 99211 — — — 5 min. 99212 Problem focused Problem focused Straightforward 10 min. 99213 Expanded problem focused Expanded problem focused Low complexity 15 min. 99214 Detailed Detailed Moderate complexity 25 min. 99215 Comprehensive Comprehensive High complexity 40 min. 2 of 3 required History of the Present Illness Past, Family and/or Social His- Type of History (HPI) (see page 2) Review of Systems (ROS) (see page 2) tory (PFSH) (see page 2) Problem Brief Not required Not required focused One to three elements Expanded Brief Problem pertinent Not required problem One to three elements Positive and pertinent negative responses for focused the system directly related to the problem(s) identified in the HPI. Detailed Extended Extended Pertinent Four or more elements (OR Positive and pertinent negative responses for 2 At least one specific item from status of three or more to 9 systems. the PFSH must be documented. chronic or inactive conditions) Comprehensive Extended Complete Complete Four or more elements (OR Positive and pertinent negative responses for At least one item from each of status of three or more at least 10 systems, including the one directly two areas must be documented chronic or inactive conditions) related to the problem identified in the HPI. for most services to established Systems with positive or pertinent negative patients. (At least one item from responses must be documented individually. For each of the three areas must be the remaining systems, a notation indicating documented for most services that all other systems are negative is permissible. -

An Osteopathic Approach to Reduction of Readmissions for Neonatal Jaundice
Osteopathic Family Physician (2013) 5, 17–23 REVIEW ARTICLE An osteopathic approach to reduction of readmissions for neonatal jaundice Rachel Click, DO,a Julie Dahl-Smith, DO,a Lindsay Fowler, DO,a Jacqueline DuBose, MD,a Margi Deneau-Saxton, RN, CCCE, CIMI, CLC, CPD,b Jennifer Herbert, MDc From aGeorgia Health Sciences University, Medical College of Georgia, Department of Family Medicine, GA; bGeorgia Health System, OB Labor and Delivery, GA; and cUniversity Primary Care, Evans, GA. KEYWORDS: Jaundice is a potentially life-threatening condition that continues to affect at-risk newborns, accounting Breastfeeding; for continued hospital readmissions. As family physicians, we should be cognizant of neonates who may Jaundice; be at risk for jaundice, including those with pathologic jaundice as well as newborns of breastfeeding Prevention; mothers, and ensure sufficient intervention is taken to help prevent further elevations in bilirubin levels. Hyperbilirubinemia; Interventions are likely to include evaluation for sepsis, education regarding feeding frequencies for both Neonatal massage breast- and bottle-fed neonates, reviewing maternal and hematologic risk factors for neonatal jaundice, and considering inborn errors of metabolism. An additional measure family physicians may consider is that of neonatal massage for those with elevated bilirubin levels. Neonatal massage, though not widely used, has been proven to promote excess bilirubin excretion, thus decreasing length of hospital stay; all the while, providing an intervention that allows parents to take an active role. r 2013 Elsevier Inc. All rights reserved. Introduction morbidity rate with bilirubin 4 20 mg/dL. “It has been estimated that the risk of kernicterus in infants with total Jaundice is a product of excess bilirubin (a product of serum bilirubin (TSB) greater than 30 mg/dL is about 1 in broken down red blood cells), which manifests as a 7 infants”.1 Less serious complications of hyperbilirubine- yellowing of the skin and eyes. -

INFORMED CARING JAUNDICE Neonatal Jaundice BILIARY
1 INFORMED CARING Situations with Adults and Children with Gallbladder, Liver and Pancreatic Disorders 2 JAUNDICE ä Does NOT mean hepatitis ä Increased breakdown of RBCs ä Altered bilirubin breakdown ä Impeded flow through liver or bile duct ä First seen in sclera, then skin 3 Neonatal Jaundice ä Not liver failure ä RBC breakdown ä Phototherapy 4 BILIARY ATRESIA ä Jaundice 2-3 weeks after birth ä Easy bruising ä Stools putty like ä Tea colored urine ä Abdominal/organ distension 5 4 F’s of Gallbladder ä Fair ä Fat X size of person X amount in diet ä Fertile X BCP X Multiparity ä Forty 6 Cholelithiasis ä Calculi within the duct or gallbladder ä Severe colicky, cramp-like pain X radiates to shoulder blade X Murphy's sign ä Cholecystitis: inflammation X Can be caused by trauma, fasting, TPN or abdominal surgery 7 Diagnostic Studies ä Ultrasound of abdomen 1 X not for the obese ä HIDA scan X nuclear medicine ä Cholangiograms X endoscopic X transvenous X intraoperative 8 Post-op Care ä High abdominal incision X respiratory compromise ä T-tube X patients need to know how to empty it X may clamp it prior to removal X caution not dislodged with movements ä NO Morphine X spasms of sphincter of Oddi 9 Post-op Nutrition ä Limited fat in diet X can have rapid transit times ä Potential fat soluble vitamin deficit X A, D, E and K ä Weight loss diet 10 LIVER FAILURE ä Cirrhosis ä Drug toxicity X acetaminophen, anesthetics, HCTZ, chemotherapy ä Infection ä Cancer ä ETOH is single most linked cause 11 LIVER FAILURE S/S ä Don’t show up until 80-90% failed -

Sleep Medicine Curriculum for Neurology Residents
Sleep Medicine Curriculum for Neurology Residents This curriculum, developed in collaboration with the AAN Consortium of Neurology Program Directors and Graduate Education Subcommittee, provides a comprehensive outline of the relevant educational goals for the future generation of adult neurologists learning sleep medicine during residency. The clinical scope of this curriculum is common and uncommon sleep disorders encountered in typical neurology practices. While the all-encompassing scope of this outline covers more than is expected to be learned by neurology residents on a given subspecialty rotation, the measurable objectives are included to provide program directors and other rotation developers the means of evaluating whether a minimum competence in sleep was attained in any combination of specific areas. Finally, as sleep medicine is a cross-disciplinary neurologic subspecialty, the curriculum ends with a table highlighting overlapping conditions between major sleep disorder categories and neurologic subspecialities. Authors: Lead Author Logan Schneider, MD [email protected] Stanford/VA Alzheimer’s Center Alon Avidan, MD, MPH, FAAN David Geffen School of Medicine at UCLA Muna Irfan, MD University of Minnesota Meena Khan, MD The Ohio State University Created: January 2020 Effective: February 2020 to February 2021 Approved by the American Academy of Neurology’s Graduate Education Subcommittee Sleep Medicine Curriculum for Neurology Residents Part I. General Clinical Approach Clinical evaluation: History Efficiently obtains a complete, relevant, and organized neurologic history Performs comprehensive review of systems pertinent to ICSD-3 sleep-wake disorder categories (sleep-related disordered breathing, hypersomnias, insomnias, parasomnias, sleep-related movement disorders, circadian disorders) Performs comprehensive review of systems probing medical conditions that are known to impact sleep-wake disorders (e.g. -

Review of Systems Health History Sheet Patient: ______DOB: ______Age: ______Gender: M / F
603 28 1/4 Road Grand Junction, CO 81506 (970) 263-2600 Review of Systems Health History Sheet Patient: _________________ DOB: ____________ Age: ______ Gender: M / F Please mark any symptoms you are experiencing that are related to your complaint today: Allergic/ Immunologic Ears/Nose/Mouth/Throat Genitourinary Men Only Frequent Sneezing Bleeding Gums Pain with Urinating Pain/Lump in Testicle Hives Difficulty Hearing Blood in Urine Penile Itching, Itching Dizziness Difficulty Urinating Burning or Discharge Runny Nose Dry Mouth Incomplete Emptying Problems Stopping or Sinus Pressure Ear Pain Urinary Frequency Starting Urine Stream Cardiovascular Frequent Infections Loss of Urinary Control Waking to Urinate at Chest Pressure/Pain Frequent Nosebleeds Hematologic / Lymphatic Night Chest Pain on Exertion Hoarseness Easy Bruising / Bleeding Sexual Problems / Irregular Heart Beats Mouth Breathing Swollen Glands Concerns Lightheaded Mouth Ulcers Integumentary (Skin) History of Sexually Swelling (Edema) Nose/Sinus Problems Changes in Moles Transmitted Diseases Shortness of Breath Ringing in Ears Dry Skin Women Only When Lying Down Endocrine Eczema Bleeding Between Shortness of Breath Increased Thirst / Growth / Lesions Periods When Walking Urination Itching Heavy Periods Constitutional Heat/Cold Intolerance Jaundice (Yellow Extreme Menstrual Pain Exercise Intolerance Gastrointestinal Skin or Eyes) Vaginal Itching, Fatigue Abdominal Pain Rash Burning or Discharge Fever Black / Tarry Stool Respiratory Waking to Urinate at Weight Gain (___lbs) Blood -

Running Head: COLORECTAL CANCER SCREENING 1
Running head: COLORECTAL CANCER SCREENING 1 COLORECTAL CANCER SCREENING IN A LARGE HEALTHCARE ORGANIZATION by Torica Todai Fuller Paper submitted in partial fulfillment of the requirements for the degree of Doctor of Nursing Practice East Carolina University College of Nursing July 22, 2019 COLORECTAL CANCER SCREENING 2 Acknowledgments First, I would like to give ALL Thanks and Praises to GOD who is the head of my life. I would like to thank Him for ordering my steps and leading me back to East Carolina University. As an adult student, I have grown and matured both professionally and spiritually. This learning experience has taught me to become a better person and better provider. Even with juggling my career, being a pastor’s wife and also a student, God still showed Himself strong in my life and I am truly thankful and honored to be used by God. This was a test, but it is now my testimony. My favorite scripture is: “I can do ALL things through CHRIST who strengthens ME” (Philippians 4:13). The journey has been filled with new friendships which have also blossomed into a tight- knit cohort family. Moreover, I am grateful to all for every word of encouragement and support. I would like to thank my colleagues for their support, Dr. Lori Haigler, the Interim Medical Director, Dr. Lan Tran-Phu, Dr. Krystle Vinson, my Site Champion, and Mr. Duane Holder, the Interim Health Director. As I close and reflect back on the last twenty-four months, I would like to applaud and thank Dr. Tracey Robertson-Bell, my DNP advisor for her words of encouragement, unwavering support and professional guidance. -

Symptomatic Approach to Gas, Belching and Bloating 21
20 Osteopathic Family Physician (2019) 20 - 25 Osteopathic Family Physician | Volume 11, No. 2 | March/April, 2019 Gennaro, Larsen Symptomatic Approach to Gas, Belching and Bloating 21 Review ARTICLE to escape. This mechanism prevents the stomach from becoming IRRITABLE BOWEL SYNDROME (IBS) Symptomatic Approach to Gas, Belching and Bloating damaged by excessive dilation.2 IBS is abdominal pain or discomfort associated with altered with OMT Treatment Options Many patients with GERD report increased belching. Transient bowel habits. It is the most commonly diagnosed GI disorder lower esophageal sphincter (LES) relaxation is the major and accounts for about 30% of all GI referrals.7 Criteria for IBS is recurrent abdominal pain at least one day per week in the Carly Gennaro, DO1; Helaine Larsen, DO1 mechanism for both belching and GERD. Recent studies have shown that the number of belches is related to the number of last three months associated with at least two of the following: times someone swallows air. These studies have concluded that 1) association with defecation, 2) change in stool frequency, 1 Good Samaritan Hospital Medical Center, West Islip, NY patients with GERD swallow more air in response to heartburn and 3) change in stool form. Diagnosis should be made using these therefore belch more frequently.3 There is no specific treatment clinical criteria and limited testing. Common symptoms are for belching in GERD patients, so for now, physicians continue to abdominal pain, bloating, alternating diarrhea and constipation, treat GERD with proton pump inhibitors (PPIs) and histamine-2 and pain relief after defecation. Pain can be present anywhere receptor antagonists with the goal of suppressing heartburn and in the abdomen, but the lower abdomen is the most common KEYWORDS: ABSTRACT: Intestinal gas production is a normal physiologic progress. -
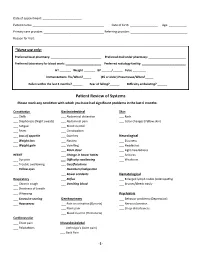
Patient Review of Systems Please Mark Any Condition with Which You Have Had Significant Problems in the Last 6 Months
Date of appointment: ________________________ Patient name: ____________________________________________ Date of birth: _________________ Age: ___________ Primary care provider: _____________________________________ Referring provider: ___________________________________ Reason for Visit: _____________________________________________________________________________________________ *Nurse use only: Preferred local pharmacy: _______________________________ Preferred mail order pharmacy: _______________________ Preferred laboratory for blood work: ______________________ Preferred radiology facility: ___________________________ HT _______ Weight _______ BP ______/______ Pulse ________ Immunizations: Flu/When?_____ (65 or older) Pneumovax/When?_____ Fallen within the last 3 months? ______ Fear of falling?______ Difficulty ambulating? ______ Patient Review of Systems Please mark any condition with which you have had significant problems in the last 6 months: Constitution Gastrointestinal Skin ___ Chills ___ Abdominal distention ___ Rash ___ Diaphoresis (Night sweats) ___ Abdominal pain ___ Color changes (Yellow skin) ___ Fatigue ___ Blood in stool ___ Fever ___ Constipation ___ Loss of appetite ___ Diarrhea Neurological ___ Weight loss ___ Nausea ___ Dizziness ___ Weight gain ___ Vomiting ___ Headaches ___ Black stool ___ Light-headedness HEENT ___ Change in bowel habits ___ Seizures ___ Eye pain ___ Difficulty swallowing ___ Weakness ___ Trouble swallowing ___ Gas/flatulence ___ Yellow eyes ___ Heartburn/indigestion ___ Bowel accidents Hematological -
Paramedic Instructional Guidelines Preparatory EMS Systems
National Emergency Medical Services Education Standards Paramedic Instructional Guidelines Preparatory EMS Systems Paramedic Education Standard Integrates comprehensive knowledge of EMS systems, safety/well being of the paramedic, and medical/legal and ethical issues, which is intended to improve the health of EMS personnel, patients, and the community. Paramedic-Level Instructional Guideline The Paramedic Instructional Guidelines in this section include all the topics and material at the AEMT level PLUS the following material: I. History of EMS A. EMS Prior to World War I 1. 1485 – Siege of Malaga, first recorded use of ambulance by military, no medical care provided 2. 1800s – Napoleon designated vehicle and attendant to head to battle field a. 1860 – first recorded use of medic and ambulance use in the United States b. 1865 – first civilian ambulance, Commercial Hospital of Cincinnati, Ohio c. 1869 – First ambulance service, Bellevue Hospital in New York, NY d. 1899 – Michael Reese Hospital in Chicago operates automobile ambulance B. EMS Between World War I and II 1. 1900s – Hospitals place interns on ambulances, first real attempt at quality scene and transport care 2. 1926 – Phoenix Fire Department enters EMS 3. 1928 – First rescue squad launched in Roanoke, VA. Squad implemented by Julien Stanley Wise and named Roanoke Life Saving Crew 4. 1940s a. Many hospital-based ambulance services shut down due to lack of manpower resulting from WWI b. City governments turn service over to police and fire departments c. No laws on minimum training d. Ambulance attendance became a form of punishment in many fire depts. C. Post-World War II 1.