Dermatology Board Review by Dr. Rina Chabra
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group R01 (Nasal preparations) Table of Contents Page INTRODUCTION 5 DISCLAIMER 7 GLOSSARY OF TERMS USED IN THIS DOCUMENT 8 ACTIVE SUBSTANCES Cyclopentamine (ATC: R01AA02) 10 Ephedrine (ATC: R01AA03) 11 Phenylephrine (ATC: R01AA04) 14 Oxymetazoline (ATC: R01AA05) 16 Tetryzoline (ATC: R01AA06) 19 Xylometazoline (ATC: R01AA07) 20 Naphazoline (ATC: R01AA08) 23 Tramazoline (ATC: R01AA09) 26 Metizoline (ATC: R01AA10) 29 Tuaminoheptane (ATC: R01AA11) 30 Fenoxazoline (ATC: R01AA12) 31 Tymazoline (ATC: R01AA13) 32 Epinephrine (ATC: R01AA14) 33 Indanazoline (ATC: R01AA15) 34 Phenylephrine (ATC: R01AB01) 35 Naphazoline (ATC: R01AB02) 37 Tetryzoline (ATC: R01AB03) 39 Ephedrine (ATC: R01AB05) 40 Xylometazoline (ATC: R01AB06) 41 Oxymetazoline (ATC: R01AB07) 45 Tuaminoheptane (ATC: R01AB08) 46 Cromoglicic Acid (ATC: R01AC01) 49 2 Levocabastine (ATC: R01AC02) 51 Azelastine (ATC: R01AC03) 53 Antazoline (ATC: R01AC04) 56 Spaglumic Acid (ATC: R01AC05) 57 Thonzylamine (ATC: R01AC06) 58 Nedocromil (ATC: R01AC07) 59 Olopatadine (ATC: R01AC08) 60 Cromoglicic Acid, Combinations (ATC: R01AC51) 61 Beclometasone (ATC: R01AD01) 62 Prednisolone (ATC: R01AD02) 66 Dexamethasone (ATC: R01AD03) 67 Flunisolide (ATC: R01AD04) 68 Budesonide (ATC: R01AD05) 69 Betamethasone (ATC: R01AD06) 72 Tixocortol (ATC: R01AD07) 73 Fluticasone (ATC: R01AD08) 74 Mometasone (ATC: R01AD09) 78 Triamcinolone (ATC: R01AD11) 82 -

4. Antibacterial/Steroid Combination Therapy in Infected Eczema
Acta Derm Venereol 2008; Suppl 216: 28–34 4. Antibacterial/steroid combination therapy in infected eczema Anthony C. CHU Infection with Staphylococcus aureus is common in all present, the use of anti-staphylococcal agents with top- forms of eczema. Production of superantigens by S. aureus ical corticosteroids has been shown to produce greater increases skin inflammation in eczema; antibacterial clinical improvement than topical corticosteroids alone treatment is thus pivotal. Poor patient compliance is a (6, 7). These findings are in keeping with the demon- major cause of treatment failure; combination prepara- stration that S. aureus can be isolated from more than tions that contain an antibacterial and a topical steroid 90% of atopic eczema skin lesions (8); in one study, it and that work quickly can improve compliance and thus was isolated from 100% of lesional skin and 79% of treatment outcome. Fusidic acid has advantages over normal skin in patients with atopic eczema (9). other available topical antibacterial agents – neomycin, We observed similar rates of infection in a prospective gentamicin, clioquinol, chlortetracycline, and the anti- audit at the Hammersmith Hospital, in which all new fungal agent miconazole. The clinical efficacy, antibac- patients referred with atopic eczema were evaluated. In terial activity and cosmetic acceptability of fusidic acid/ a 2-month period, 30 patients were referred (22 children corticosteroid combinations are similar to or better than and 8 adults). The reason given by the primary health those of comparator combinations. Fusidic acid/steroid physician for referral in 29 was failure to respond to combinations work quickly with observable improvement prescribed treatment, and one patient was referred be- within the first week. -

Inflammatory Or Infectious Hair Disease? a Case of Scalp Eschar and Neck Lymph Adenopathy After a Tick Bite
Case Report ISSN: 2574 -1241 DOI: 10.26717/BJSTR.2021.35.005688 Adherent Serous Crust of the Scalp: Inflammatory or Infectious Hair Disease? A Case of Scalp Eschar and Neck Lymph Adenopathy after a Tick Bite Starace M1, Vezzoni R*2, Alessandrini A1 and Piraccini BM1 1Dermatology - IRCCS, Policlinico Sant’Orsola, Department of Specialized, Experimental and Diagnostic Medicine, Alma Mater Studiorum, University of Bologna, Italy 2Dermatology Clinic, Maggiore Hospital, University of Trieste, Italy *Corresponding author: Roberta Vezzoni, Dermatology Clinic, Maggiore Hospital, University of Trieste, Italy ARTICLE INFO ABSTRACT Received: Published: April 17, 2021 The appearance of a crust initially suggests inflammatory scalp diseases, although infectious diseases such as impetigo or insect bites should also be considered among April 27, 2021 the differential diagnoses. We report a case of 40-year-old woman presentedB. Burgdorferi to our, Citation: Starace M, Vezzoni R, Hair Disease Outpatient Service with an adherent serous crust on the scalp and lymphadenopathy of the neck. Serological tests confirmed the aetiology of while rickettsia infection was excluded. Lyme borreliosis can mimic rickettsia infection Alessandrini A, Piraccini BM. Adherent and may present as scalp eschar and neck lymphadenopathy after a tick bite (SENLAT). Serous Crust of the Scalp: Inflammatory Appropriate tests should be included in the diagnostic workup of patients with necrotic or Infectious Hair Disease? A Case of Scalp scalpKeywords: eschar in order to promptly set -

Skin Manifestation of SARS-Cov-2: the Italian Experience
Journal of Clinical Medicine Article Skin Manifestation of SARS-CoV-2: The Italian Experience Gerardo Cazzato 1 , Caterina Foti 2, Anna Colagrande 1, Antonietta Cimmino 1, Sara Scarcella 1, Gerolamo Cicco 1, Sara Sablone 3, Francesca Arezzo 4, Paolo Romita 2, Teresa Lettini 1 , Leonardo Resta 1 and Giuseppe Ingravallo 1,* 1 Section of Pathology, University of Bari ‘Aldo Moro’, 70121 Bari, Italy; [email protected] (G.C.); [email protected] (A.C.); [email protected] (A.C.); [email protected] (S.S.); [email protected] (G.C.); [email protected] (T.L.); [email protected] (L.R.) 2 Section of Dermatology and Venereology, University of Bari ‘Aldo Moro’, 70121 Bari, Italy; [email protected] (C.F.); [email protected] (P.R.) 3 Section of Forensic Medicine, University of Bari ‘Aldo Moro’, 70121 Bari, Italy; [email protected] 4 Section of Gynecologic and Obstetrics Clinic, University of Bari ‘Aldo Moro’, 70121 Bari, Italy; [email protected] * Correspondence: [email protected] Abstract: At the end of December 2019, a new coronavirus denominated Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) was identified in Wuhan, Hubei province, China. Less than three months later, the World Health Organization (WHO) declared coronavirus disease-19 (COVID-19) to be a global pandemic. Growing numbers of clinical, histopathological, and molecular findings were subsequently reported, among which a particular interest in skin manifestations during the course of the disease was evinced. Today, about one year after the development of the first major infectious foci in Italy, various large case series of patients with COVID-19-related skin Citation: Cazzato, G.; Foti, C.; manifestations have focused on skin specimens. -

Updates in Pediatric Dermatology
Peds Derm Updates ELIZABETH ( LISA) SWANSON , M D ADVANCED DERMATOLOGY COLORADO ROCKY MOUNTAIN HOSPITAL FOR CHILDREN [email protected] Disclosures Speaker Sanofi Regeneron Amgen Almirall Pfizer Advisory Board Janssen Powerpoints are the peacocks of the business world; all show, no meat. — Dwight Schrute, The Office What’s New In Atopic Dermatitis? Impact of Atopic Dermatitis Eczema causes stress, sleeplessness, discomfort and worry for the entire family Treating one patient with eczema is an example of “trickle down” healthcare Patients with eczema have increased risk of: ADHD Anxiety and Depression Suicidal Ideation Parental depression Osteoporosis and osteopenia (due to steroids, decreased exercise, and chronic inflammation) Impact of Atopic Dermatitis Sleep disturbances are a really big deal Parents of kids with atopic dermatitis lose an average of 1-1.5 hours of sleep a night Even when they sleep, kids with atopic dermatitis don’t get good sleep Don’t enter REM as much or as long Growth hormone is secreted in REM (JAAD Feb 2018) Atopic Dermatitis and Food Allergies Growing evidence that food allergies might actually be caused by atopic dermatitis Impaired barrier allows food proteins to abnormally enter the body and stimulate allergy Avoiding foods can be harmful Proper nutrition is important Avoidance now linked to increased risk for allergy and anaphylaxis Refer severe eczema patients to Allergist before 4-6 mos of age to talk about food introduction Pathogenesis of Atopic Dermatitis Skin barrier -

Prediction of Premature Termination Codon Suppressing Compounds for Treatment of Duchenne Muscular Dystrophy Using Machine Learning
Prediction of Premature Termination Codon Suppressing Compounds for Treatment of Duchenne Muscular Dystrophy using Machine Learning Kate Wang et al. Supplemental Table S1. Drugs selected by Pharmacophore-based, ML-based and DL- based search in the FDA-approved drugs database Pharmacophore WEKA TF 1-Palmitoyl-2-oleoyl-sn-glycero-3- 5-O-phosphono-alpha-D- (phospho-rac-(1-glycerol)) ribofuranosyl diphosphate Acarbose Amikacin Acetylcarnitine Acetarsol Arbutamine Acetylcholine Adenosine Aldehydo-N-Acetyl-D- Benserazide Acyclovir Glucosamine Bisoprolol Adefovir dipivoxil Alendronic acid Brivudine Alfentanil Alginic acid Cefamandole Alitretinoin alpha-Arbutin Cefdinir Azithromycin Amikacin Cefixime Balsalazide Amiloride Cefonicid Bethanechol Arbutin Ceforanide Bicalutamide Ascorbic acid calcium salt Cefotetan Calcium glubionate Auranofin Ceftibuten Cangrelor Azacitidine Ceftolozane Capecitabine Benserazide Cerivastatin Carbamoylcholine Besifloxacin Chlortetracycline Carisoprodol beta-L-fructofuranose Cilastatin Chlorobutanol Bictegravir Citicoline Cidofovir Bismuth subgallate Cladribine Clodronic acid Bleomycin Clarithromycin Colistimethate Bortezomib Clindamycin Cyclandelate Bromotheophylline Clofarabine Dexpanthenol Calcium threonate Cromoglicic acid Edoxudine Capecitabine Demeclocycline Elbasvir Capreomycin Diaminopropanol tetraacetic acid Erdosteine Carbidopa Diazolidinylurea Ethchlorvynol Carbocisteine Dibekacin Ethinamate Carboplatin Dinoprostone Famotidine Cefotetan Dipyridamole Fidaxomicin Chlormerodrin Doripenem Flavin adenine dinucleotide -

Erythema Marginatum
Figurative Erythemas Michelle Goedken, DO Affiliated Dermatology Scottsdale, AZ Figurative Erythemas • Erythema annulare centrifugum • Erythema marginatum • Erythema migrans • Erythema gyratum repens • Erythema multiforme Erythemas • Erythemas represent a change in the color of the skin that is due to the dilation of blood vessels, especially those in the papillary and reticular dermis • The color is blanchable and most last for days to months • Figurative erythemas have an annular, arciform or polycyclic appearance ERYTHEMA ANNULARE CENTRIFUGUM ERYTHEMA ANNULARE CENTRIFUGUM • Pathogenesis: EAC represents a reaction pattern or hypersensitivity to one of many antigens – IL-2 and TNF-alpha may have a role – Most patients do not have an underlying disease identified ERYTHEMA ANNULARE CENTRIFUGUM • Associated with: – Infection » Dermatophytes and other fungi (Candida and Penicillium in blue cheese) » Viruses: poxvirus, EBV, VZV, HIV » Parasites and ectoparasites – Drugs: diuretics, antimalarials, gold, NSAIDs, finasteride, amitriptyline, etizolam, Ustekinumab (2012) ERYTHEMA ANNULARE CENTRIFUGUM – Foods – Autoimmune endocrinopathies – Neoplasms (lymphomas and leukemias) – Pregnancy – Hypereosinophilic syndrome – Lupus (2014) ERYTHEMA ANNULARE CENTRIFUGUM http://www.dermaamin.com Rongioletti, F., Fausti, V., & Parodi, A ERYTHEMA ANNULARE CENTRIFUGUM • 2 major forms: – Superficial: classic trailing scale, may have associated pruritus – Deep: infiltrated borders, usually no scale, edges are elevated, usually not pruritic ERYTHEMA ANNULARE CENTRIFUGUM -

Belly Button…
KNOWLEDGE TO PRACTICE DES CONNAISSANCES À LA PRATIQUE Diagnostic Challenge A “ticklish” belly button… Tahira Daya*; Conor McKaigney, MD† CASE HISTORY A 42-year-old woman presented to the emergency department (ED) with acute onset periumbilical pain and erythema, which started that morning. She felt nauseated but denied vomiting. Her bowel movements were regular and non-bloody. She did not have a fever. She had no significant prior medical history, no recent trauma, and had no previous surgeries. In the ED, she appeared uncomfortable from pain but was not in acute distress. Vital signs upon initial presentation included a heart rate of 120 beats/min, a blood pressure of 145/111 mm Hg, respiratory rate of 16 breaths/min, temperature of 36.8°C (98.2°F), and an oxygen saturation of 99% on room air. Her vital signs two hours later after a fluid challenge and analgesics had improved to a heart rate of 74 beats/min and blood pressure of 132/83 mm Hg, and the remaining vitals were the same. Her abdomen demonstrated periumbilical erythema, with a central clearing; the area was tender to Figure 1. Periumbilical rash with central clearing. palpation, and warm to touch. Images of her periumbilical region are shown in Figure 1. The rest of the abdomen was soft and non-tender, with no masses or organomegaly. An ED ultrasound was performed to assess for possible b) Cellulitis subcutaneous abscess, which was not seen. Cardiovascular and respiratory exams were unremarkable. c) Lyme disease d) Subcutaneous abscess e) Erythema multiforme QUESTION For the answer to this challenge, see next page. -

Lyme Disease Diagnostic Support Tool
1 / 11 For further details, click on the DIAGNOSTIC SUPPORT TOOL underlined words. Localized and disseminated stages of Lyme disease This diagnostic support tool is intended mainly for primary care clinicians. It is provided for information purposes only and should not replace the judgement of the clinician who performs the activities reserved under a statute or regulation. The recommendations in this tool were developed using a systematic process and are supported by the scientific literature and the knowledge and experience of Québec health professionals, experts and patients. For further details, go to the “Publications” section of INESSS’s website inesss.qc.ca. This tool does not deal with other tick-borne infections or with the much-debated form of Lyme disease, which is sometimes referred to as the chronic form. WHAT IS LYME DISEASE ? WHAT ARE THE DIFFERENT STAGES OF THE DISEASE? GENERAL INFORMATION • Lyme disease is an infectious disease caused by bacterial Localized stage (sometimes called the early stage): Beginning Patient with a tick genospecies of Borrelia burgdorferi, which are transmitted of the infection before dissemination of the bacteria in the • If tick is attached, refer to the procedure for removing it. to humans by black-legged ticks that are carriers. bloodstream. • Refer to the tick surveillance procedure. • Main manifestation observed: • It is a notifiable disease (MADO) • Consult the decision support tool or the Québec’s national and is on the increase in Québec. Not always present or noticed. medical protocol on post-exposure prophylaxis. • It can affect several anatomical systems at the same time. If present, usually appears • Identifying the tick and obtaining proof that it carries of Lym 3 to 30 days after infection or e d B. -

Diagnosis, Classification, and Management of Erythema
Arch Dis Child 2000;83:347–352 347 Diagnosis, classification, and management of Arch Dis Child: first published as 10.1136/adc.83.4.347 on 1 October 2000. Downloaded from erythema multiforme and Stevens–Johnson syndrome C Léauté-Labrèze, T Lamireau, D Chawki, J Maleville, A Taïeb Abstract become widely accepted that EM and SJS, as Background—In adults, erythema multi- well as toxic epidermal necrolysis, are all part of forme (EM) is thought to be mainly a single “EM spectrum”. In both EM and SJS, related to herpes infection and Stevens– pathological changes in the earliest skin lesion Johnson syndrome (SJS) to drug reac- consist of the accumulation of mononuclear tions. cells around the superficial dermal blood Aims—To investigate this hypothesis in vessels; epidermal damage is more characteris- children, and to review our experience in tic of EM with keratinocyte necrosis leading to the management of these patients. multilocular intraepidermal blisters.5 In fact, Methods—A retrospective analysis of 77 there is little clinical resemblance between paediatric cases of EM or SJS admitted to typical EM and SJS, and recently some authors the Children’s Hospital in Bordeaux be- have proposed a reconsideration of the “spec- tween 1974 and 1998. trum” concept and a return to the original Results—Thirty five cases, inadequately description.15–17 According to these authors, the documented or misdiagnosed mostly as term EM should be restricted to acrally urticarias or non-EM drug reactions were distributed typical targets or raised oedema- excluded. Among the remaining 42 pa- tous papules. Depending on the presence or tients (14 girls and 28 boys), 22 had EM (11 absence of mucous membrane erosions the EM minor and 11 EM major), 17 had SJS, cases may be classified as EM major or EM 16 and three had isolated mucous membrane minor. -
EAR, NOSE and OROPHARYNX Updated: October 2020
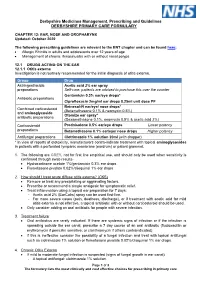
Derbyshire Medicines Management, Prescribing and Guidelines DERBYSHIRE PRIMARY CARE FORMULARY CHAPTER 12: EAR, NOSE AND OROPHARYNX Updated: October 2020 The following prescribing guidelines are relevant to the ENT chapter and can be found here: • Allergic Rhinitis in adults and adolescents over 12 years of age • Management of chronic rhinosinusitis with or without nasal polyps 12.1 DRUGS ACTING ON THE EAR 12.1.1 Otitis externa Investigation is not routinely recommended for the initial diagnosis of otitis externa. Group Drug Astringent/acidic Acetic acid 2% ear spray preparations Self-care: patients are advised to purchase this over the counter Gentamicin 0.3% ear/eye drops* Antibiotic preparations Ciprofloxacin 2mg/ml ear drops 0.25ml unit dose PF Betnesol-N ear/eye/ nose drops* Combined corticosteroid (Betamethasone 0.1% & neomycin 0.5%) and aminoglycoside Otomize ear spray* antibiotic preparations (Dexamethasone 0.1%, neomycin 0.5% & acetic acid 2%) Corticosteroid Prednisolone 0.5% ear/eye drops Lower potency preparations Betamethasone 0.1% ear/eye/ nose drops Higher potency Antifungal preparations Clotrimazole 1% solution 20ml (with dropper) * In view of reports of ototoxicity, manufacturers contra-indicate treatment with topical aminoglycosides in patients with a perforated tympanic membrane (eardrum) or patent grommet. 1. The following are GREY, not for first line empirical use, and should only be used when sensitivity is confirmed through swab results- • Hydrocortisone acetate 1%/gentamicin 0.3% ear drops • Flumetasone pivalate 0.02%/clioquinol 1% ear drops 2. How should I treat acute diffuse otitis externa? (CKS) • Remove or treat any precipitating or aggravating factors. • Prescribe or recommend a simple analgesic for symptomatic relief. -

Fundamentals of Dermatology Describing Rashes and Lesions
Dermatology for the Non-Dermatologist May 30 – June 3, 2018 - 1 - Fundamentals of Dermatology Describing Rashes and Lesions History remains ESSENTIAL to establish diagnosis – duration, treatments, prior history of skin conditions, drug use, systemic illness, etc., etc. Historical characteristics of lesions and rashes are also key elements of the description. Painful vs. painless? Pruritic? Burning sensation? Key descriptive elements – 1- definition and morphology of the lesion, 2- location and the extent of the disease. DEFINITIONS: Atrophy: Thinning of the epidermis and/or dermis causing a shiny appearance or fine wrinkling and/or depression of the skin (common causes: steroids, sudden weight gain, “stretch marks”) Bulla: Circumscribed superficial collection of fluid below or within the epidermis > 5mm (if <5mm vesicle), may be formed by the coalescence of vesicles (blister) Burrow: A linear, “threadlike” elevation of the skin, typically a few millimeters long. (scabies) Comedo: A plugged sebaceous follicle, such as closed (whitehead) & open comedones (blackhead) in acne Crust: Dried residue of serum, blood or pus (scab) Cyst: A circumscribed, usually slightly compressible, round, walled lesion, below the epidermis, may be filled with fluid or semi-solid material (sebaceous cyst, cystic acne) Dermatitis: nonspecific term for inflammation of the skin (many possible causes); may be a specific condition, e.g. atopic dermatitis Eczema: a generic term for acute or chronic inflammatory conditions of the skin. Typically appears erythematous,