Platelet Structure and Function
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Two Faces of Thrombosis: Coagulation Cascade and Platelet Aggregation. Are Platelets the Main Therapeutic Target
Thrombosis and Circulation Open Access Cimmino et al., J Thrombo Cir 2017, 3:1 Review Article Open Access The Two Faces of Thrombosis: Coagulation Cascade and Platelet Aggregation. Are Platelets the Main Therapeutic Target? Giovanni Cimmino*, Salvatore Fischetti and Paolo Golino Department of Cardio-Thoracic and Respiratory Sciences, Section of Cardiology, University of Campania “Luigi Vanvitelli”, Naples, Italy *Corresponding author: Giovanni Cimmino, MD, PhD, Department of Cardio-Thoracic and Respiratory Sciences, Section of Cardiology, University of Campania “Luigi Vanvitelli”, via Leonardo Bianchi, 180131 Naples, Italy. Tel: +39-081-7064175, Fax: +39-081-7064234; E-mail: [email protected] Received date: Dec 28, 2016, Accepted date: Jan 27, 2017, Published date: Jan 31, 2017 Copyright: © 2017 Giovanni C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Acute thrombus formation is the pathophysiological substrate underlying several clinical conditions, such as acute coronary syndrome (ACS) and stroke. Activation of coagulation cascade is a key step of the thrombotic process: vessel injury results in exposure of the glycoprotein tissue factor (TF) to the flowing blood. Once exposed, TF binds factor VII/VIIa (FVII/FVIIa) and in presence of calcium ions, it forms a tertiary complex able to activate FX to FXa, FIX to FIXa, and FVIIa itself. The final step is thrombin formation at the site of vessel injury with subsequent platelet activation, fibrinogen to fibrin conversion and ultimately thrombus formation. Platelets are the key cells in primary hemostasis. -

RIASTAP®, Fibrinogen Concentrate (Human) Lyophilized Powder for Solution for Intravenous Injection
HIGHLIGHTS OF PRESCRIBING INFORMATION -------------------------------------CONTRAINDICATIONS ------------------------------------ These highlights do not include all the information needed to use RIASTAP • Known anaphylactic or severe systemic reactions to human plasma-derived products (4). safely and effectively. See full prescribing information for RIASTAP. ---------------------------------WARNINGS AND PRECAUTIONS---------------------------- RIASTAP®, Fibrinogen Concentrate (Human) • Monitor patients for early signs of anaphylaxis or hypersensitivity reactions and if necessary, discontinue administration and institute appropriate treatment (5.1). Lyophilized Powder for Solution for Intravenous Injection • Thrombotic events have been reported in patients receiving RIASTAP. Weigh the benefits of administration versus the risks of thrombosis (5.2). Initial U.S. Approval: 2009 • Because RIASTAP is made from human blood, it may carry a risk of transmitting ------------------------------------RECENT MAJOR CHANGES--------------------------------- infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent Indications and Usage (1) 06/2021 and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent (5.3). Dosage and Administration (2.2) 07/2020 -------------------------------------ADVERSE REACTIONS-------------------------------------- ----------------------------------INDICATIONS AND USAGE----------------------------------- • The most serious adverse reactions observed are thrombotic episodes (pulmonary RIASTAP, Fibrinogen -

Platelet Surface Glycoproteins. Studies on Resting and Activated Platelets and Platelet Membrane Microparticles in Normal Subjec
Platelet surface glycoproteins. Studies on resting and activated platelets and platelet membrane microparticles in normal subjects, and observations in patients during adult respiratory distress syndrome and cardiac surgery. J N George, … , N Kieffer, P J Newman J Clin Invest. 1986;78(2):340-348. https://doi.org/10.1172/JCI112582. Research Article The accurate definition of surface glycoprotein abnormalities in circulating platelets may provide better understanding of bleeding and thrombotic disorders. Platelet surface glycoproteins were measured on intact platelets in whole blood and platelet membrane microparticles were assayed in cell-free plasma using 125I-monoclonal antibodies. The glycoproteins (GP) studied were: GP Ib and GP IIb-IIIa, two of the major intrinsic plasma membrane glycoproteins; GMP-140, an alpha- granule membrane glycoprotein that becomes exposed on the platelet surface following secretion; and thrombospondin (TSP), an alpha-granule secreted glycoprotein that rebinds to the platelet surface. Thrombin-induced secretion in normal platelets caused the appearance of GMP-140 and TSP on the platelet surface, increased exposure of GP IIb-IIIa, and decreased antibody binding to GP Ib. Patients with adult respiratory distress syndrome had an increased concentration of GMP-140 and TSP on the surface of their platelets, demonstrating in vivo platelet secretion, but had no increase of platelet microparticles in their plasma. In contrast, patients after cardiac surgery with cardiopulmonary bypass demonstrated changes consistent with membrane fragmentation without secretion: a decreased platelet surface concentration of GP Ib and GP IIb with no increase of GMP-140 and TSP, and an increased plasma concentration of platelet membrane microparticles. These methods will help to define acquired abnormalities of platelet surface glycoproteins. -

Factor V Leiden Thrombophilia
Factor V Leiden thrombophilia Description Factor V Leiden thrombophilia is an inherited disorder of blood clotting. Factor V Leiden is the name of a specific gene mutation that results in thrombophilia, which is an increased tendency to form abnormal blood clots that can block blood vessels. People with factor V Leiden thrombophilia have a higher than average risk of developing a type of blood clot called a deep venous thrombosis (DVT). DVTs occur most often in the legs, although they can also occur in other parts of the body, including the brain, eyes, liver, and kidneys. Factor V Leiden thrombophilia also increases the risk that clots will break away from their original site and travel through the bloodstream. These clots can lodge in the lungs, where they are known as pulmonary emboli. Although factor V Leiden thrombophilia increases the risk of blood clots, only about 10 percent of individuals with the factor V Leiden mutation ever develop abnormal clots. The factor V Leiden mutation is associated with a slightly increased risk of pregnancy loss (miscarriage). Women with this mutation are two to three times more likely to have multiple (recurrent) miscarriages or a pregnancy loss during the second or third trimester. Some research suggests that the factor V Leiden mutation may also increase the risk of other complications during pregnancy, including pregnancy-induced high blood pressure (preeclampsia), slow fetal growth, and early separation of the placenta from the uterine wall (placental abruption). However, the association between the factor V Leiden mutation and these complications has not been confirmed. Most women with factor V Leiden thrombophilia have normal pregnancies. -

Coagadex, Human Coagulation Factor X
26 July 2018 EMA/CHMP/455550/2018 Committee for Medicinal Products for Human Use (CHMP) CHMP extension of indication variation assessment report Coagadex International non-proprietary name: human coagulation factor X Procedure No. EMEA/H/C/003855/II/0007 Note Assessment report as adopted by the CHMP with all information of a commercially confidential nature deleted. 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2018. Reproduction is authorised provided the source is acknowledged. Table of contents 1. Background information on the procedure .............................................. 5 1.1. Type II variation .................................................................................................. 5 1.2. Steps taken for the assessment of the product ......................................................... 6 2. Scientific discussion ................................................................................ 6 2.1. Introduction......................................................................................................... 6 2.2. Non-clinical aspects .............................................................................................. 7 2.3. Clinical aspects .................................................................................................... 7 2.3.1. Introduction ..................................................................................................... -

Factor V Leiden Thrombophilia Jody Lynn Kujovich, MD
GENETEST REVIEW Genetics in Medicine Factor V Leiden thrombophilia Jody Lynn Kujovich, MD TABLE OF CONTENTS Pathogenic mechanisms and molecular basis.................................................2 Obesity ...........................................................................................................8 Prevalence..............................................................................................................2 Surgery...........................................................................................................8 Diagnosis................................................................................................................2 Thrombosis not convincingly associated with Factor V Leiden....................8 Clinical diagnosis..............................................................................................2 Arterial thrombosis...........................................................................................8 Testing................................................................................................................2 Myocardial infarction.......................................................................................8 Indications for testing......................................................................................3 Stroke .................................................................................................................8 Natural history and clinical manifestations......................................................3 Genotype-phenotype -
![PROTEIN C DEFICIENCY 1215 Adulthood and a Large Number of Children and Adults with Protein C Mutations [6,13]](https://docslib.b-cdn.net/cover/8040/protein-c-deficiency-1215-adulthood-and-a-large-number-of-children-and-adults-with-protein-c-mutations-6-13-1348040.webp)
PROTEIN C DEFICIENCY 1215 Adulthood and a Large Number of Children and Adults with Protein C Mutations [6,13]
Haemophilia (2008), 14, 1214–1221 DOI: 10.1111/j.1365-2516.2008.01838.x ORIGINAL ARTICLE Protein C deficiency N. A. GOLDENBERG* and M. J. MANCO-JOHNSON* *Hemophilia & Thrombosis Center, Section of Hematology, Oncology, and Bone Marrow Transplantation, Department of Pediatrics, University of Colorado Denver and The ChildrenÕs Hospital, Aurora, CO; and Division of Hematology/ Oncology, Department of Medicine, University of Colorado Denver, Aurora, CO, USA Summary. Severe protein C deficiency (i.e. protein C ment of acute thrombotic events in severe protein C ) activity <1 IU dL 1) is a rare autosomal recessive deficiency typically requires replacement with pro- disorder that usually presents in the neonatal period tein C concentrate while maintaining therapeutic with purpura fulminans (PF) and severe disseminated anticoagulation; protein C replacement is also used intravascular coagulation (DIC), often with concom- for prevention of these complications around sur- itant venous thromboembolism (VTE). Recurrent gery. Long-term management in severe protein C thrombotic episodes (PF, DIC, or VTE) are common. deficiency involves anticoagulation with or without a Homozygotes and compound heterozygotes often protein C replacement regimen. Although many possess a similar phenotype of severe protein C patients with severe protein C deficiency are born deficiency. Mild (i.e. simple heterozygous) protein C with evidence of in utero thrombosis and experience deficiency, by contrast, is often asymptomatic but multiple further events, intensive treatment and may involve recurrent VTE episodes, most often monitoring can enable these individuals to thrive. triggered by clinical risk factors. The coagulopathy in Further research is needed to better delineate optimal protein C deficiency is caused by impaired inactiva- preventive and therapeutic strategies. -
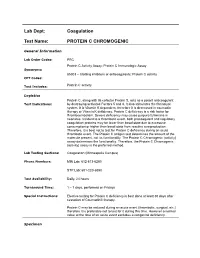
Lab Dept: Coagulation Test Name: PROTEIN C CHROMOGENIC
Lab Dept: Coagulation Test Name: PROTEIN C CHROMOGENIC General Information Lab Order Codes: PRC Protein C Activity Assay; Protein C Immunologic Assay Synonyms: 85303 – Clotting inhibitors or anticoagulants; Protein C activity CPT Codes: Test Includes: Protein C activity Logistics Protein C, along with its cofactor Protein S, acts as a potent anticoagulant Test Indications: by destroying activated Factors 5 and 8. It also stimulates the fibrinolytic system. It is Vitamin K dependent, therefore it is decreased in coumadin therapy or Vitamin K deficiency. Protein C deficiency is a risk factor for thromboembolism. Severe deficiency may cause purpura fulminans in neonates. Incident to a thrombotic event, both procoagulant and regulatory coagulation proteins may be lower than basal state due to excessive consumption or higher than basal state from reactive overproduction. Therefore, it is best not to test for Protein C deficiency during an acute thrombotic event. The Protein C antigen test determines the amount of the molecule present, not its functionality. The Protein C Chromogenic (activity) assay determines the functionality. Therefore, the Protein C Chromogenic (activity) assay is the preferred method. Lab Testing Sections: Coagulation (Minneapolis Campus) Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours Turnaround Time: 1 – 7 days, performed on Fridays Special Instructions: Elective testing for Protein C deficiency is best done at least 30 days after cessation of Coumadin® therapy. Protein C may be reduced during an acute event (thrombotic, surgical, etc.) therefore it is preferable not to test for it during this time. However a normal value at the time of an acute event excludes a congenital deficiency. -

Assessing Plasmin Generation in Health and Disease
International Journal of Molecular Sciences Review Assessing Plasmin Generation in Health and Disease Adam Miszta 1,* , Dana Huskens 1, Demy Donkervoort 1, Molly J. M. Roberts 1, Alisa S. Wolberg 2 and Bas de Laat 1 1 Synapse Research Institute, 6217 KD Maastricht, The Netherlands; [email protected] (D.H.); [email protected] (D.D.); [email protected] (M.J.M.R.); [email protected] (B.d.L.) 2 Department of Pathology and Laboratory Medicine and UNC Blood Research Center, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] * Correspondence: [email protected]; Tel.: +31-(0)-433030693 Abstract: Fibrinolysis is an important process in hemostasis responsible for dissolving the clot during wound healing. Plasmin is a central enzyme in this process via its capacity to cleave fibrin. The ki- netics of plasmin generation (PG) and inhibition during fibrinolysis have been poorly understood until the recent development of assays to quantify these metrics. The assessment of plasmin kinetics allows for the identification of fibrinolytic dysfunction and better understanding of the relationships between abnormal fibrin dissolution and disease pathogenesis. Additionally, direct measurement of the inhibition of PG by antifibrinolytic medications, such as tranexamic acid, can be a useful tool to assess the risks and effectiveness of antifibrinolytic therapy in hemorrhagic diseases. This review provides an overview of available PG assays to directly measure the kinetics of plasmin formation and inhibition in human and mouse plasmas and focuses on their applications in defining the role of plasmin in diseases, including angioedema, hemophilia, rare bleeding disorders, COVID- 19, or diet-induced obesity. -

Coagulation Simplified…
Coagulation Simplified… Published by ACKNOWLEDGEMENTS CONTENTS We gratefully acknowledge the support and funding provided by the Ontario Ministry of Health 1. The Basics of Coagulation and Clot Breakdown . 4–7 and Long-Term Care. 2. Routine Coagulation Tests . 8–17 Special thanks to the following people and organizations who provided their expertise in Evaluating coagulation in the laboratory . 8 reviewing the content of this handbook: Sample collection for coagulation testing . 9 Prothrombin Time (PT) . 10 L Gini Bourner (QMP-LS Hematology Committee) International Normalized Ratio (INR) . 11 L Dr. Jeannie Callum Activated Partial Thromboplastin Time (APTT) . 12 L Dr. Allison Collins Thrombin Time (TT) . 13 Fibrinogen . 14 L Dr. William Geerts D-dimer . 15 L Dr. Alejandro Lazo-Langner Anti-Xa assay . 16 L Dr. Ruth Padmore (QMP-LS Hematology Committee) Summary . 17 L Anne Raby (QMP-LS Hematology Committee) 3. Anticoagulant Drugs . 18–25 L Dr. Margaret Rand Unfractionated Hepari n (UFH) . 18 L Dr. Alan Tinmouth Low Molecular Weight Heparins (LMWHs) . 19 Fondaparinux . 20 Warfarin . 21 Thanks also to: Direct Thrombin Inhibitors (DTI) . 23 L Dale Roddick, photographer, Sunnybrook Health Sciences Centre Direct Xa Inhibitors . 25 L Reena Manohar, graphic artist, Sunnybrook Health Sciences Centre 4. Evaluating Abnormal Coagulation Tests . 26–29 L The ECAT Foundation Prolonged PT / INR with normal APTT . 26 CLOT-ED Images used or modified with permission from Prolonged APTT with normal PT / INR . 27 the ECAT Foundation, The Netherlands. Prolonged APTT and PT / INR . 28 Prolonged Thrombin Time (TT) with normal or prolonged APTT and PT / INR . 29 March 2013 5. Approach to the Evaluation of the Bleeding Patient . -

I. Introduction II. Factor X in the Coagulation Cascade III. Medical Conditions Treated with Anticoagulants V. Structure of A
Coagulation Factor X and Apixaban St. Dominic Middle School SMART Team Jennifer Austin, Mia Bando, Christopher Brzozowski, Giovanni Faraciano, Caroline Flyke, Nicholas Hilbert, Isabella Huschitt, Thomas Hyde, Elizabeth Klingsporn, Janna Lieungh Emily Maslowski, Kaitlyn O’Hair, Mary Rose Otten, Isabelle Phan, Sophia Pittman, Ryan Reilly, Alex Reinbold, Catherine Simmons, Michael Sohn, Emma Urban, Rachel Vasan Teacher: Donna LaFlamme St. Dominic Catholic School 18105 W. Capitol Drive, Brookfield, WI 53045 Mentors: Michael Pickart, Ph.D. and Xiaoang Xing Concordia University School of Pharmacy, 12800 N. Lake Shore Dr., Mequon WI 53097 I. Introduction VI. Apixaban versus Warfarin Factor X is a clotting protein that is made in the liver and found in the blood. Pharmaceutical companies have recently developed new oral anticoagulants (NOACs) that inhibit Factor X, such as apixaban (Eliquis), to treat IV. Catalytic Domain of Activated Factor X In the September 15, 2011 issue of The New England Journal of Medicine, Christopher B. and prevent life threatening blood clots. An older anticoagulant, warfarin, is extremely difficult to dose, Granger et. al. reported on the Aristotle Clinical Trials involving over 18,000 patients with requires constant blood level monitoring, and has many drug and food interactions. Apixaban has none of Bound to Apixaban atrial fibrillation. Apixaban was found to be superior to warfarin in preventing stroke or these drawbacks, but it does lack an antidote to stop bleeding in emergencies. Our mentors are using zebrafish systemic embolism, caused less bleeding, and resulted in lower mortality. (Funded by The blood-clotting protein Factor X is composed of a heavy protein chain and a light protein chain. -

Relationship Between Circulating Tumor Cells and Tissue
ANTICANCER RESEARCH 37 : 1787-1791 (2017) doi:10.21873/anticanres.11512 Relationship Between Circulating Tumor Cells and Tissue Plasminogen Activator in Patients with Early Breast Cancer BRANISLAV BYSTRICKY 1,2 , SILVIA JURISOVA 1,3 , MARIAN KARABA 3,4 , GABRIEL MINARIK 5, JURAJ BENCA 3,6 , TATIANA SEDLÁCKOVÁ 5, LUBOMIRA TOTHOVA 5, BARBORA VLKOVA 5, ZUZANA CIERNA 7, PAVOL JANEGA 7,8 , DENISA MANASOVA 9, PAULINA GRONESOVA 10 , DANIEL PINDAK 3,4 , JOZEF MARDIAK 1,3 , PETER CELEC 5 and MICHAL MEGO 1,3,9 1Second Department of Medical Oncology, 5Institute of Molecular Biomedicine, 7Department of Pathology, and 9Translational Research Unit, Faculty of Medicine, Comenius University, Bratislava, Slovakia; 2Department of Oncology, Faculty Hospital Trencin, Trencin, Slovakia; 3National Cancer Institute, Bratislava, Slovakia; 4Department of Surgery, Slovak Medical University, Bratislava, Slovakia; 6Department of Medicine, St. Elizabeth University, Bratislava, Slovakia; 8Institute of Normal and Pathological Physiology, Bratislava, Slovakia; 10 Cancer Research Institute, Slovak Academy of Sciences, Bratislava, Slovakia Abstract. Aim: Cancer increases the risk of venous significance. There was no association of plasma tPA with thromboembolism (VTE) and circulating tumor cells (CTCs) any of the observed patient or tumor characteristics. are associated with an increased risk of VTE and, thus, with Conclusion: Even though the blood coagulation pathway may increased D-dimers as a product of fibrinolysis. Tissue be activated in more aggressive disease related to an elevated plasminogen activator (tPA) is one of the key enzymes in the CTC count, in this study, we did not find any association fibrinolytic pathway. Its activity is crucial in maintaining the between CTCs and plasma concentrations of tPA.