Neuropathic Pain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Scalp Dysesthesia. Case Report Disestesia Do Escalpo
BrJP. São Paulo, 2020 jan-mar;3(1):86-7 CASE REPORT Scalp dysesthesia. Case report Disestesia do escalpo. Relato de caso Letícia Arrais Rocha1, João Batista Santos Garcia1, Thiago Alves Rodrigues1 DOI 10.5935/2595-0118.20200016 ABSTRACT RESUMO BACKGROUND AND OBJECTIVES: Scalp dysesthesia is JUSTIFICATIVA E OBJETIVOS: A disestesia do escalpo ca- characterized by the presence of several localized or diffuse symp- racteriza-se pela presença de diversos sintomas localizados ou toms, such as burning, pain, pruritus or stinging sensations, wi- difusos, como queimação, dor, prurido ou sensações de picada, thout objective findings in the physical examination of the pa- sem achados objetivos no exame físico do paciente que possam tient that can explain and link the existing symptomatology to explicar e ligar os sintomas existentes à alguma outra etiologia. some other etiology. The aim of this study was to describe a case O objetivo deste estudo foi descrever um caso de disestesia de of scalp dysesthesia, from its clinical and laboratory investigation escalpo, desde a sua investigação clínica e laboratorial, até a con- and the conduct adopted. duta adotada. CASE REPORT: A 38-year-old male patient, first assigned to RELATO DO CASO: Paciente do sexo masculino, 38 anos. Pri- the Dermatology Service, with complaints of pruritus in the meiramente foi ao serviço de Dermatologia com queixa de pru- scalp for 5 years. In the consultation at the Pain Service, the pa- rido em couro cabeludo há cinco anos. Na consulta do Serviço tient complained of daily, intermittent and burning dysesthetic de Dor, o paciente queixava-se de sensações disestésicas como: sensations, such as tingling and pruritus in the bipariethoccipital formigamento e prurido em região biparieto-occipital que piora region, worsening with heat and associated with severe pain in com o calor, associada à dor de forte intensidade, diária, intermi- the cervical region. -

Pain and Dysesthesia in Patients with Spinal Cord Injury: a Postal Survey
Spinal Cord (2001) 39, 256 ± 262 ã 2001 International Medical Society of Paraplegia All rights reserved 1362 ± 4393/01 $15.00 www.nature.com/sc Original Article Pain and dysesthesia in patients with spinal cord injury: A postal survey NB Finnerup*,1, IL Johannesen2, SH Sindrup3, FW Bach1 and TS Jensen1 1Department of Neurology and Danish Pain Research Centre, University Hospital of Aarhus, Denmark; 2Department of Rheumatology, Viborg Hospital, Denmark; 3Department of Neurology, Odense University Hospital, Denmark Study design: A postal survey. Objectives: To assess the prevalence and characteristics of pain and dysesthesia in a community based sample of patients with spinal cord injury (SCI) with special focus on neuropathic pain. Setting: Community. Western half of Denmark. Methods: We mailed a questionnaire to all outpatients (n=436) of the Viborg rehabilitation centre for spinal cord injury. The questionnaire contained questions regarding cause and level of spinal injury and amount of sensory and motor function below this level. The words pain and unpleasant sensations were used to describe pain (P) and dysesthesia (D) respectively. Questions included location and intensity of chronic pain or dysesthesia, degree of interference with daily activity and sleep, presence of paroxysms and evoked pain or dysesthesia, temporal aspects, alleviating and aggravating factors, McGill Pain Questionnaire (MPQ) and treatment. Results: Seventy-six per cent of the patients returned the questionnaire, (230 males and 100 females). The ages ranged from 19 to 80 years (median 42.6 years) and time since spinal injury ranged from 0.5 to 39 years (median 9.3 years). The majority (475%) of patients had traumatic spinal cord injury. -

Chemotherapy-Induced Neuropathy and Diabetes: a Scoping Review
Review Chemotherapy-Induced Neuropathy and Diabetes: A Scoping Review Mar Sempere-Bigorra 1,2 , Iván Julián-Rochina 1,2 and Omar Cauli 1,2,* 1 Department of Nursing, University of Valencia, 46010 Valencia, Spain; [email protected] (M.S.-B.); [email protected] (I.J.-R.) 2 Frailty Research Organized Group (FROG), University of Valencia, 46010 Valencia, Spain * Correspondence: [email protected] Abstract: Although cancer and diabetes are common diseases, the relationship between diabetes, neuropathy and the risk of developing peripheral sensory neuropathy while or after receiving chemotherapy is uncertain. In this review, we highlight the effects of chemotherapy on the onset or progression of neuropathy in diabetic patients. We searched the literature in Medline and Scopus, covering all entries until 31 January 2021. The inclusion and exclusion criteria were: (1) original article (2) full text published in English or Spanish; (3) neuropathy was specifically assessed (4) the authors separately analyzed the outcomes in diabetic patients. A total of 259 papers were retrieved. Finally, eight articles fulfilled the criteria, and four more articles were retrieved from the references of the selected articles. The analysis of the studies covered the information about neuropathy recorded in 768 cancer patients with diabetes and 5247 control cases (non-diabetic patients). The drugs investigated are chemotherapy drugs with high potential to induce neuropathy, such as platinum derivatives and taxanes, which are currently the mainstay of treatment of various cancers. The predisposing effect of co-morbid diabetes on chemotherapy-induced peripheral neuropathy depends on the type of symptoms and drug used, but manifest at any drug regimen dosage, although greater neuropathic signs are also observed at higher dosages in diabetic patients. -

Diabetic Neuropathy: a Position Statement by the American
136 Diabetes Care Volume 40, January 2017 Diabetic Neuropathy: A Position Rodica Pop-Busui,1 Andrew J.M. Boulton,2 Eva L. Feldman,3 Vera Bril,4 Roy Freeman,5 Statement by the American Rayaz A. Malik,6 Jay M. Sosenko,7 and Dan Ziegler8 Diabetes Association Diabetes Care 2017;40:136–154 | DOI: 10.2337/dc16-2042 Diabetic neuropathies are the most prevalent chronic complications of diabetes. This heterogeneous group of conditions affects different parts of the nervous system and presents with diverse clinical manifestations. The early recognition and appropriate man- agement of neuropathy in the patient with diabetes is important for a number of reasons: 1. Diabetic neuropathy is a diagnosis of exclusion. Nondiabetic neuropathies may be present in patients with diabetes and may be treatable by specific measures. 2. A number of treatment options exist for symptomatic diabetic neuropathy. 3. Up to 50% of diabetic peripheral neuropathies may be asymptomatic. If not recognized and if preventive foot care is not implemented, patients are at risk for injuries to their insensate feet. 4. Recognition and treatment of autonomic neuropathy may improve symptoms, POSITION STATEMENT reduce sequelae, and improve quality of life. Among the various forms of diabetic neuropathy, distal symmetric polyneurop- athy (DSPN) and diabetic autonomic neuropathies, particularly cardiovascular au- tonomic neuropathy (CAN), are by far the most studied (1–4). There are several 1 atypical forms of diabetic neuropathy as well (1–4). Patients with prediabetes may Division of Metabolism, Endocrinology & Diabe- – tes, Department of Internal Medicine, University also develop neuropathies that are similar to diabetic neuropathies (5 10). -

Neuromyotonia with Polyneuropathy, Prominent Psychoorganic Syndrome
Ehler and Meleková Journal of Medical Case Reports (2015) 9:101 DOI 10.1186/s13256-015-0581-0 JOURNAL OF MEDICAL CASE REPORTS CASE REPORT Open Access Neuromyotonia with polyneuropathy, prominent psychoorganic syndrome, insomnia, and suicidal behavior without antibodies: a case report Edvard Ehler* and Alena Meleková Abstract Introduction: Peripheral nerve hyperexcitability disorders are characterized by constant muscle fiber activity. Acquired neuromyotonia manifests clinically in cramps, fasciculations, and stiffness. In Morvan’s syndrome the signs of peripheral nerve hyperexcitability are accompanied by autonomic symptoms, sensory abnormalities, and brain disorders. Case presentation: A 70-year-old Caucasian man developed, in the course of 3 months, polyneuropathy with unpleasant dysesthesia of lower extremities and gradually increasing fasciculations, muscle stiffness and fatigue. Subsequently, he developed a prominent insomnia with increasing psychological changes and then he attempted a suicide. Electromyography confirmed a sensory-motor polyneuropathy of a demyelinating type. The findings included fasciculations as well as myokymia, doublets and multiplets, high frequency discharges, and afterdischarges, following motor nerve stimulation. No auto-antibodies were found either in his blood or cerebrospinal fluid. Magnetic resonance imaging of his brain showed small, unspecific, probably postischemic changes. A diagnosis of Morvan’s syndrome was confirmed; immunoglobulin (2g/kg body weight) was applied intravenously, and, subsequently, -

Chronic Cryptogenic Sensory Polyneuropathy Clinical and Laboratory Characteristics
ORIGINAL CONTRIBUTION Chronic Cryptogenic Sensory Polyneuropathy Clinical and Laboratory Characteristics Gil I. Wolfe, MD; Noel S. Baker, MD; Anthony A. Amato, MD; Carlayne E. Jackson, MD; Sharon P. Nations, MD; David S. Saperstein, MD; Choon H. Cha, MD; Jonathan S. Katz, MD; Wilson W. Bryan, MD; Richard J. Barohn, MD Background: Chronic sensory-predominant polyneu- duration of symptoms of 62.9 months. Symptoms al- ropathy (PN) is a common clinical problem confronting most always started in the feet and included distal numb- neurologists. Even with modern diagnostic approaches, ness or tingling in 86% of patients and pain in 72% of many of these PNs remain unclassified. patients. Despite the absence of motor symptoms at pre- sentation, results of motor nerve conduction studies were Objective: To better define the clinical and laboratory abnormal in 60% of patients, and electromyographic evi- characteristics of a large group of patients with crypto- dence of denervation was observed in 70% of patients. genic sensory polyneuropathy (CSPN) evaluated in 2 uni- Results of laboratory studies were consistent with axo- versity-based neuromuscular clinics. nal degeneration. Patients with and without pain were similar regarding physical findings and laboratory test ab- Design: Medical record review of patients evaluated normalities. Only a few patients (,5%) had no evi- for PN during a 2-year period. We defined CSPN on dence of large-fiber dysfunction on physical examina- the basis of pain, numbness, and tingling in the distal tion or electrophysiologic studies. All 66 patients who extremities without symptoms of weakness. Sensory had follow-up examinations (mean, 12.5 months) re- symptoms and signs had to evolve for at least 3 mained ambulatory. -

Pharmacologic Management of Chronic Neuropathic Pain Review of the Canadian Pain Society Consensus Statement
Clinical Review Pharmacologic management of chronic neuropathic pain Review of the Canadian Pain Society consensus statement Alex Mu MD FRCPC Erica Weinberg MD Dwight E. Moulin MD PhD Hance Clarke MD PhD FRCPC Abstract Objective To provide family physicians with EDITOR’S KEY POINTS a practical clinical summary of the Canadian • Gabapentinoids and tricyclic antidepressants play an important role in Pain Society (CPS) revised consensus first-line management of neuropathic pain (NeP). Evidence published statement on the pharmacologic management since the 2007 Canadian Pain Society consensus statement on treatment of neuropathic pain. of NeP shows that serotonin-norepinephrine reuptake inhibitors should now also be among the first-line agents. Quality of evidence A multidisciplinary • Tramadol and opioids are considered second-line treatments owing to their interest group within the CPS conducted a increased complexity of follow-up and monitoring, plus their potential for systematic review of the literature on the adverse side effects, medical complications, and abuse. Cannabinoids are current treatments of neuropathic pain in currently recommended as third-line agents, as sufficient-quality studies are drafting the revised consensus statement. currently lacking. Recommended fourth-line treatments include methadone, anticonvulsants with lesser evidence of efficacy (eg, lamotrigine, lacosamide), tapentadol, and botulinum toxin. There is some support for analgesic Main message Gabapentinoids, tricyclic combinations in selected NeP conditions. antidepressants, and serotonin-norepinephrine reuptake inhibitors are the first-line agents • Many of these pharmacologic treatments are off-label for pain or for treating neuropathic pain. Tramadol and on-label for specific pain conditions, and these issues should be clearly other opioids are recommended as second- conveyed and documented. -

NMDA Receptor Antagonists for the Treatment of Neuropathic Pain Compared to Placebo: a Systematic Review and Meta-Analysis
Open Journal of Dentistry and Oral Medicine 5(4): 59-71, 2017 http://www.hrpub.org DOI: 10.13189/ojdom.2017.050401 NMDA Receptor Antagonists for the Treatment of Neuropathic Pain Compared to Placebo: A Systematic Review and Meta-analysis Byron Larsen1, Kristin Mau1, Mariela Padilla2, Reyes Enciso3,* 1Master of Science Program in Orofacial Pain and Oral Medicine, Herman Ostrow School of Dentistry, University of Southern California, USA 2Division of Periodontology, Diagnostic Sciences and Dental Hygiene, Herman Ostrow School of Dentistry, University of Southern California, USA 3Division of Dental Public Health and Pediatric Dentistry, Herman Ostrow School of Dentistry, University of Southern California, USA Copyright©2017 by authors, all rights reserved. Authors agree that this article remains permanently open access under the terms of the Creative Commons Attribution License 4.0 International License Abstract The objective of this study is to evaluate the Neuropathic pain has been linked to structural and efficacy of N-Methyl-D-aspartate (NMDA) receptor functional somatosensory nervous system alternations that antagonists on neuropathic pain disorders that can occur in produce spontaneous pain and pathologically intensified the orofacial region. These disorders included: Postherpetic reactions to noxious and innocuous stimuli [1]. It is Neuralgia (PHN), Complex Regional Pain Syndrome suggested that different mechanisms are at play regarding (CRPS), Atypical Odontalgia, Temporomandibular Joint orofacial neuropathic pain due to the diverse clinical (TMJ) Arthralgia and facial neuropathies. Materials and manifestations in disorders of various etiologies [2]. More Methods: Three databases (Medline through PubMed, Web specifically, involvement pertains to both peripheral and of Science, and Cochrane library) were searched on January central sensitization mechanisms [3]. -

The Journal of Rheumatology Volume 75, No. Is Fibromyalgia a Neuropathic Pain Syndrome?
The Journal of Rheumatology Volume 75, no. Is fibromyalgia a neuropathic pain syndrome? Michael C Rowbotham J Rheumatol 2005;75;38-40 http://www.jrheum.org/content/75/38 1. Sign up for TOCs and other alerts http://www.jrheum.org/alerts 2. Information on Subscriptions http://jrheum.com/faq 3. Information on permissions/orders of reprints http://jrheum.com/reprints_permissions The Journal of Rheumatology is a monthly international serial edited by Earl D. Silverman featuring research articles on clinical subjects from scientists working in rheumatology and related fields. Downloaded from www.jrheum.org on September 24, 2021 - Published by The Journal of Rheumatology Is Fibromyalgia a Neuropathic Pain Syndrome? MICHAEL C. ROWBOTHAM ABSTRACT. The fibromyalgia syndrome (FM) seems an unlikely candidate for classification as a neuropathic pain. The disorder is diagnosed based on a compatible history and the presence of multiple areas of musculoskeletal tenderness. A consistent pathology in either the peripheral or central nervous system (CNS) has not been demonstrated in patients with FM, and they are not at higher risk for diseases of the CNS such as multiple sclerosis or of the peripheral nervous system such as peripheral neuropathy. A large proportion of FM suf- ferers have accompanying symptoms and signs of uncertain etiology, such as chronic fatigue, sleep distur- bance, and bowel/bladder irritability. With the exception of migraine headaches and possibly irritable bowel syndrome, the accompanying disorders are clearly not neurological in origin. The impetus to classify the FM as a neuropathic pain comes from multiple lines of research suggesting widespread pain and tenderness are associated with chronic sensitization of the CNS. -

Neuropathic Pain (E Eisenberg, Section Editor)
Curr Pain Headache Rep (2017) 21: 28 DOI 10.1007/s11916-017-0629-5 NEUROPATHIC PAIN (E EISENBERG, SECTION EDITOR) Neuropathic Pain: Central vs. Peripheral Mechanisms Kathleen Meacham1,2 & Andrew Shepherd1,2 & Durga P. Mohapatra1,2 & Simon Haroutounian1,2 Published online: 21 April 2017 # Springer Science+Business Media New York 2017 Abstract identify potentially self-sustaining infra-slow CNS oscillatory Purpose of Review Our goal is to examine the processes— activity that may be unique to pNP patients. both central and peripheral—that underlie the development of Summary While new preclinical evidence supports and ex- peripherally-induced neuropathic pain (pNP) and to highlight pands upon the key role of central mechanisms in neuropathic recent evidence for mechanisms contributing to its mainte- pain, clinical evidence for an autonomous central mechanism nance. While many pNP conditions are initiated by damage remains relatively limited. Recent findings from both preclin- to the peripheral nervous system (PNS), their persistence ap- ical and clinical studies recapitulate the critical contribution of pears to rely on maladaptive processes within the central ner- peripheral input to maintenance of neuropathic pain. Further vous system (CNS). The potential existence of an autonomous clinical investigations on the possibility of standalone central pain-generating mechanism in the CNS creates significant im- contributions to pNP may be assisted by a reconsideration of plications for the development of new neuropathic pain treat- the agreed terms or criteria for diagnosing the presence of ments; thus, work towards its resolution is crucial. Here, we central sensitization in humans. seek to identify evidence for PNS and CNS independently generating neuropathic pain signals. -

Upper Limb Pain and Paresthesia in a Post-Stroke Patient Treated With
02 Brain Neurorehabil. 2018 Mar;11(1):e1 https://doi.org/10.12786/bn.2018.11.e1 pISSN 1976-8753·eISSN 2383-9910 Brain & NeuroRehabilitation Case Upper Limb Pain and Paresthesia in a Post-Stroke Patient Treated with Ultrasound-Guided Electrical Twitch-Obtaining Intramuscular Stimulation(ETOIMS) of Scalene Muscles Je Shik Nam, Yeo-Reum Choe, Seo Yeon Yoon, Tae Im Yi Received: Sep 1, 2017 Highlights Revised: Sep 29, 2017 Accepted: Oct 2, 2017 • Disputed thoracic outlet syndrome (TOS) can be one of the possible causes of post-stroke Correspondence to pain. Tae Im Yi • Ultrasound-guided electrical twitch-obtaining intramuscular stimulation can be used as a Departments of Rehabilitation Medicine, safe and minimally invasive technique for the treatment of the disputed TOS. Bundang Jesaeng General Hospital, • Large-scale randomized controlled studies are needed to confirm its therapeutic efficacy. 20 Seohyeon-ro 180 beon-gil, Bundang-gu, Seongnam 13590, Korea. E-mail: [email protected] Copyright © 2018. Korea Society for Neurorehabilitation i 02 Brain Neurorehabil. 2018 Mar;11(1):e1 https://doi.org/10.12786/bn.2018.11.e1 pISSN 1976-8753·eISSN 2383-9910 Brain & NeuroRehabilitation Case Upper Limb Pain and Paresthesia in a Post-Stroke Patient Treated with Ultrasound-Guided Electrical Twitch-Obtaining Intramuscular Stimulation(ETOIMS) of Scalene Muscles Je Shik Nam , Yeo-Reum Choe , Seo Yeon Yoon , Tae Im Yi Department of Rehabilitation Medicine, Bundang Jesaeng General Hospital, Seongnam, Korea Received: Sep 1, 2017 ABSTRACT Revised: Sep 29, 2017 Accepted: Oct 2, 2017 In post-stroke patients, the pain or paresthesia of the affected limb is common. -
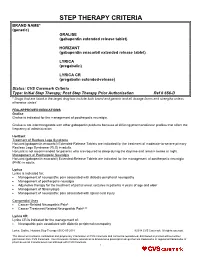
STEP THERAPY CRITERIA BRAND NAME* (Generic) GRALISE (Gabapentin Extended Release Tablet)
STEP THERAPY CRITERIA BRAND NAME* (generic) GRALISE (gabapentin extended release tablet) HORIZANT (gabapentin enacarbil extended release tablet) LYRICA (pregabalin) LYRICA CR (pregabalin extended-release) Status: CVS Caremark Criteria Type: Initial Step Therapy; Post Step Therapy Prior Authorization Ref # 656-D * Drugs that are listed in the target drug box include both brand and generic and all dosage forms and strengths unless otherwise stated FDA-APPROVED INDICATIONS Gralise Gralise is indicated for the management of postherpetic neuralgia. Gralise is not interchangeable with other gabapentin products because of differing pharmacokinetic profiles that affect the frequency of administration. Horizant Treatment of Restless Legs Syndrome Horizant (gabapentin enacarbil) Extended-Release Tablets are indicated for the treatment of moderate-to-severe primary Restless Legs Syndrome (RLS) in adults. Horizant is not recommended for patients who are required to sleep during the daytime and remain awake at night. Management of Postherpetic Neuralgia Horizant (gabapentin enacarbil) Extended-Release Tablets are indicated for the management of postherpetic neuralgia (PHN) in adults. Lyrica Lyrica is indicated for: Management of neuropathic pain associated with diabetic peripheral neuropathy Management of postherpetic neuralgia Adjunctive therapy for the treatment of partial onset seizures in patients 4 years of age and older Management of fibromyalgia Management of neuropathic pain associated with spinal cord injury Compendial Uses Cancer-Related Neuropathic Pain6 Cancer Treatment Related Neuropathic Pain6,12 Lyrica CR Lyrica CR is indicated for the management of: Neuropathic pain associated with diabetic peripheral neuropathy Lyrica, Gralise, Horizant Step Therapy 656-D 05-2018 ©2018 CVS Caremark. All rights reserved. This document contains confidential and proprietary information of CVS Caremark and cannot be reproduced, distributed or printed without written permission from CVS Caremark.