Avelumab (Anti-PD-L1)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

List of Marginable OTC Stocks
List of Marginable OTC Stocks @ENTERTAINMENT, INC. ABACAN RESOURCE CORPORATION ACE CASH EXPRESS, INC. $.01 par common No par common $.01 par common 1ST BANCORP (Indiana) ABACUS DIRECT CORPORATION ACE*COMM CORPORATION $1.00 par common $.001 par common $.01 par common 1ST BERGEN BANCORP ABAXIS, INC. ACETO CORPORATION No par common No par common $.01 par common 1ST SOURCE CORPORATION ABC BANCORP (Georgia) ACMAT CORPORATION $1.00 par common $1.00 par common Class A, no par common Fixed rate cumulative trust preferred securities of 1st Source Capital ABC DISPENSING TECHNOLOGIES, INC. ACORN PRODUCTS, INC. Floating rate cumulative trust preferred $.01 par common $.001 par common securities of 1st Source ABC RAIL PRODUCTS CORPORATION ACRES GAMING INCORPORATED 3-D GEOPHYSICAL, INC. $.01 par common $.01 par common $.01 par common ABER RESOURCES LTD. ACRODYNE COMMUNICATIONS, INC. 3-D SYSTEMS CORPORATION No par common $.01 par common $.001 par common ABIGAIL ADAMS NATIONAL BANCORP, INC. †ACSYS, INC. 3COM CORPORATION $.01 par common No par common No par common ABINGTON BANCORP, INC. (Massachusetts) ACT MANUFACTURING, INC. 3D LABS INC. LIMITED $.10 par common $.01 par common $.01 par common ABIOMED, INC. ACT NETWORKS, INC. 3DFX INTERACTIVE, INC. $.01 par common $.01 par common No par common ABLE TELCOM HOLDING CORPORATION ACT TELECONFERENCING, INC. 3DO COMPANY, THE $.001 par common No par common $.01 par common ABR INFORMATION SERVICES INC. ACTEL CORPORATION 3DX TECHNOLOGIES, INC. $.01 par common $.001 par common $.01 par common ABRAMS INDUSTRIES, INC. ACTION PERFORMANCE COMPANIES, INC. 4 KIDS ENTERTAINMENT, INC. $1.00 par common $.01 par common $.01 par common 4FRONT TECHNOLOGIES, INC. -

Moderna Appoints Oncology Leader Dr. Stephen Kelsey As President of Onkaido
Moderna Appoints Oncology Leader Dr. Stephen Kelsey as President of Onkaido Former Genentech executive to lead Moderna’s first venture company, focused exclusively in novel biology for oncology drug development CAMBRIDGE, Mass., July 1, 2014— Moderna Therapeutics, the pioneer in developing messenger RNA (mRNA) TherapeuticsTM, a revolutionary treatment modality to enable the in vivo production of therapeutic proteins, announced today that Stephen Kelsey, M.D., will become president of Onkaido Therapeutics, Moderna’s oncology drug development company, effective July 21. Launched in January of this year, Onkaido is Moderna’s first venture company, focused exclusively on developing and commercializing mRNA-based oncology treatments. “As we continue to grow Moderna and perfect our mRNA Therapeutics platform, we are also focused on building a transformational oncology company that will benefit patients and society. This requires hiring the best oncology talent to lead Onkaido,” said Stéphane Bancel, president and founding chief executive officer, Moderna. “Steve brings a wealth of experience in oncology drug development to his new role. His knowledge and leadership, combined with the team of Onkaido scientists and Moderna’s innovative mRNA technology, will help speed a new class of cancer drugs to patients around the world.” Dr. Kelsey has extensive pharmaceutical industry experience in oncology. After 16 years as an academic clinician, he started his industry career at Sugen, and later was vice president of hematology/oncology at Genentech. While at Genentech, Dr. Kelsey played a significant role in the development of key products Perjeta®, Kadcyla® and Erivedge®, as well as other molecules in the company’s oncology portfolio. He left Genentech in 2009 to run Geron’s oncology division, where he served for four years as executive vice president, research and development, and chief medical officer helping to develop therapeutics and vaccines to fight cancer. -

Print Layout 1
TECHNICAL PROGRAM Monday, March 19 5:00 – 8:00 pm Welcome Reception Tuesday, March 20 8:00 – 10:00 Session 1: Setting the Conference Context and Drivers Chair: Geoff Slaff (Amgen) Roger Perlmutter (Amgen) Conquering the Innovation Deficit in Drug Discovery Helen Winkle (CDER, FDA) Regulatory Modernization 10:00 – 10:30 Break Vendor and poster review 10:30 – 12:30 Session 2: Rapid Cell Line Development and Improved Expression System Development Chairs: Timothy Charlebois (Wyeth) and John Joly (Genentech) Amy Shen (Genentech) Stable Antibody Production Cell-Line Development with an Improved Selection Process and Accelerated Timeline Mark Leonard (Wyeth) High-Performing Cell-Line Development within a Rapid and Integrated Platform Process Control Pranhitha Reddy (Amgen) Applying Quality-by-Design to Cell Line Development Lin Zhang (Pfizer) Development of a Fully-Integrated Automated System for High-Throughput Screening and Selection of Single Cells Expressing Monoclonal Antibodies 12:30 – 2:00 Lunch Vendor and poster review 2:00 – 4:30 Session 3: High-Throughput Bulk Process Development Chairs: Brian Kelley (Wyeth) and Jorg Thommes (Biogen Idec) Colette Ranucci (Merck) Development of a Multi-Well Plate System for High-Throughput Process Development Min Zhang (SAFC Biosciences) CHO Media Library – an Efficient Platform for Rapid Development and Optimization of Cell Culture Media Supporting High Production of Pharmaceutical Proteins in Chinese Hamster Ovary Cells Nigel Titchener-Hooker The Use of Ultra-Scale-Down Approaches to Enable Rapid Investigation -

Genentech Tocilizumab Letter of Authority June 24 2021
June 24, 2021 Hoffmann-La Roche, Ltd. C/O Genentech, Inc. Attention: Dhushy Thambipillai Regulatory Project Management 1 DNA Way, Bldg 45-1 South San Francisco, CA 94080 RE: Emergency Use Authorization 099 Dear Ms. Thambipillai: This letter is in response to Genentech, Inc.’s (Genentech) request that the Food and Drug Administration (FDA) issue an Emergency Use Authorization (EUA) for the emergency use of Actemra1 (tocilizumab) for the treatment of coronavirus disease 2019 (COVID-19) in certain hospitalized patients, as described in the Scope of Authorization (Section II) of this letter, pursuant to Section 564 of the Federal Food, Drug, and Cosmetic Act (the Act) (21 U.S.C. §360bbb-3). On February 4, 2020, pursuant to Section 564(b)(1)(C) of the Act, the Secretary of the Department of Health and Human Services (HHS) determined that there is a public health emergency that has a significant potential to affect national security or the health and security of United States citizens living abroad, and that involves the virus that causes coronavirus disease 2019 (COVID-19).2 On the basis of such determination, the Secretary of HHS on March 27, 2020, declared that circumstances exist justifying the authorization of emergency use of drugs and biological products during the COVID-19 pandemic, pursuant to Section 564 of the Act (21 3 U.S.C. 360bbb-3), subject to terms of any authorization issued under that section. Actemra is a recombinant humanized monoclonal antibody that selectively binds to both soluble and membrane-bound human IL-6 receptors (sIL-6R and mIL-6R) and subsequently inhibits IL- 6-mediated signaling through these receptors. -

Current Sustaining Member Companies
CURRENT SUSTAINING MEMBER COMPANIES MEMBER FOR OVER: 10 Years 25 Years 50 Years Member Since (alphabetical order) 1976 3M Medical Markets Center 2010 Endo Pharmaceuticals 1963 Novartis Pharmaceuticals 2019 10-Square Solutions 2019 EMD Serono, Inc. 2019 Novo Nordisk, Inc. 1985 Abbott Laboratories, Inc. 2017 Exelixis 2019 Optinose 2013 AbbVie Inc. 2016 Express Scripts Federal Pharmacy 2018 Organogenesis 2017 ACADIA Pharmaceuticals, Inc. 2010 Federal Practitioner 2004 Otsuka America Pharmaceutical, Inc. 2019 Aimmune 2018 Foundation Medicine, Inc. 2018 Pacira BioSciences, Inc. 2003 Alcon Laboratories, Inc. 2006 Gilead Sciences 2018 Paratek Pharmaceuticals 2017 Alkermes, Inc. 1989 Genentech Inc. 1990 Pfizer Pharmaceuticals 2002 Allergan, Inc. 1983 GLAXOSMITHKLINE 2017 Pharmacyclics, LLC 2019 Almirall LLC 2013 Golden State Medical Supply, Inc. 2019 Portola Pharmaceuticals, Inc. 2019 Alnylam Pharmaceuticals 2019 Greenwich Biosciences 2019 Red One Medical 2019 Altarum Institute 2013 Gulf Coast Pharmaceuticals Plus, LLC 2009 Regenesis Biomedical, Inc. 2012 American Medical Depot 2008 Heritage Health Solutions, Inc. 2019 Relypsa, Inc. 2019 Aptive Resources LLC 2017 Hill-Rom Company 2011 Remund Group, LLC 2013 Arbor Pharmaceuticals, LLC 2018 Hu-Friedy Manufacturing Co 2018 Rigel Pharmaceuticals 2014 Argentum Medical, LLC 2019 Indivior 2016 Sage Products, LLC 2019 ASM Research, LLC 2019 ImmunoVation, LLC 2018 Sage Therapeutics 1986 Astellas Pharma US, Inc. 2019 Incyte Corporation 2000 Sanofi 1995 AstraZeneca 2015 Intercept Pharmaceuticals 2004 Siemens Medical Solutions 2018 Avanir Pharmaceuticals 2019 Ipsen Biopharmaceuticals, Inc. 2019 SK Life Science, Inc. 2017 Bausch Health Companies, Inc. 2018 IT Cadre 2002 Smith & Nephew, Inc. 1985 Baxter Healthcare Corporation 1989 J & J Health Care Systems, Inc. 2019 Sobi Inc. 1996 Bayer Corporation 2014 Jazz Pharmaceuticals Inc. -

R&D Update Call 2020
R&D Update Call 2020 Luciano Rossetti, Global Head of Research & Development Rehan Verjee, Head of the Global Innovative Medicine Franchises & President of EMD Serono Joern-Peter Halle, Head of Research Klaus Edvardsen, Head of Oncology Development September 25, 2020 Disclaimer Publication of Merck KGaA, Darmstadt, Germany. In the United States and Canada the group of companies affiliated with Merck KGaA, Darmstadt, Germany operates under individual business names (EMD Serono, Millipore Sigma, EMD Performance Materials). To reflect such fact and to avoid any misconceptions of the reader of the publication certain logos, terms and business descriptions of the publication have been substituted or additional descriptions have been added. This version of the publication, therefore, slightly deviates from the otherwise identical version of the publication provided outside the United States and Canada. 2 Disclaimer Cautionary Note Regarding Forward-Looking Statements and financial indicators This communication may include “forward-looking statements.” Statements that include words such as “anticipate,” “expect,” “should,” “would,” “intend,” “plan,” “project,” “seek,” “believe,” “will,” and other words of similar meaning in connection with future events or future operating or financial performance are often used to identify forward-looking statements. All statements in this communication, other than those relating to historical information or current conditions, are forward-looking statements. We intend these forward-looking statements to be covered by the safe harbor provisions for forward-looking statements in the Private Securities Litigation Reform Act of 1995. These forward-looking statements are subject to a number of risks and uncertainties, many of which are beyond control of Merck KGaA, Darmstadt, Germany, which could cause actual results to differ materially from such statements. -
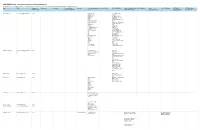
2020-2021 Cancer Communications Committee Disclosures All Relationships Are Considered Compensated
2020-2021 Cancer Communications Committee Disclosures All relationships are considered compensated. Relationships are self-held unless otherwise noted. I = Immediate Family Member, Inst = My Institution Name EMAIL Committee Employment Leadership Stock and Other Honoraria Consulting or Advisory Speakers' Bureau Research Funding Patents, Royalties, Other Expert Testimony Travel, Other Relationship (OPTIONAL) (OPTIONAL) Open Member Status Ownership Interests Role Intellectual Property Accommodations, Uncompensated Payments Link Expenses Relationships Neeraj Agarwal [email protected] Active Astellas Pharma Active Biotech (Inst) Astellas Pharma Amgen (Inst) AstraZeneca AstraZeneca (Inst) AstraZeneca Bavarian Nordic (Inst) AVEO Bayer (Inst) Bayer BN ImmunoTherapeutics Bristol-Myers Squibb (Inst) Calithera Biosciences Bristol-Myers Squibb (Inst) Eisai Calithera Biosciences EMD Serono (Inst) Exelixis Celldex (Inst) Foundation Medicine Eisai (Inst) Foundation One Inc Exelixis (Inst) Genentech Genentech (Inst) Janssen Oncology GlaxoSmithKline (Inst) Lilly Immunomedics (Inst) Lilly Janssen (Inst) lily Merck (Inst) Medivation/Astellas Newlink Genetics (Inst) MEI Pharma Novartis (Inst) Merck Pfizer (Inst) Nektar Prometheus (Inst) Novartis Rexahn Pharmaceuticals Pfizer (Inst) Pfizer Sanofi (Inst) Pharmacyclics Takeda (Inst) Seattle Genetics TRACON Pharma (Inst) Muhammad S. Beg muhammad.beg@utsouthwestern. Active Array BioPharma Agios (Inst) edu AstraZeneca/MedImmune ArQule (Inst) Cancer Commons AstraZeneca/MedImmune Ipsen (Inst) Legend Biotech -

Guidelines with Regard to the Composition, Calculation and Management of the Index
INDEX METHODOLOGY Solactive Pharma Breakthrough Value Index Version 2.1 dated September 03, 2020 Contents Important Information 1. Index specifications 1.1 Short Name and ISIN 1.2 Initial Value 1.3 Distribution 1.4 Prices and Calculation Frequency 1.5 Weighting 1.6 Index Committee 1.7 Publication 1.8 Historical Data 1.9 Licensing 2. Composition of the Index 2.1 Selection of the Index Components 2.2 Ordinary Adjustment 2.3 Extraordinary Adjustment 3. Calculation of the Index 3.1 Index Formula 3.2 Accuracy 3.3 Adjustments 3.4 Dividends and other Distributions 3.5 Corporate Actions 3.6 Correction Policy 3.7 Market Disruption 3.8 Consequences of an Extraordinary Event 4. Definitions 5. Appendix 5.1 Contact Details 5.2 Calculation of the Index – Change in Calculation Method 2 Important Information This document (“Index Methodology Document”) contains the underlying principles and regulations regarding the structure and the operating of the Solactive Pharma Breakthrough Value Index. Solactive AG shall make every effort to implement regulations. Solactive AG does not offer any explicit or tacit guarantee or assurance, neither pertaining to the results from the use of the Index nor the Index value at any certain point in time nor in any other respect. The Index is merely calculated and published by Solactive AG and it strives to the best of its ability to ensure the correctness of the calculation. There is no obligation for Solactive AG – irrespective of possible obligations to issuers – to advise third parties, including investors and/or financial intermediaries, of any errors in the Index. -

Healthcare & Life Sciences Industry Update
Healthcare & Life Sciences Industry Update August 2011 Member FINRA/SIPC www.harriswilliams.com What We’ve Been Reading August 2011 • The biggest story from inside the Beltway over the last month was the battle and eventual deal to raise the U.S. debt ceiling to avoid an impending August 2nd default. The Budget Control Act of 2011 will raise the debt ceiling by $2.1-$2.4 trillion, while reducing spending by approximately $2.1 trillion over the next decade. In an interesting post-deal analysis, Michael Hiltzik of the Los Angeles Times notes that despite the protracted negotiations over a broad spectrum of cost-cutting measures, healthcare was not raised as a primary issue. Some have found this especially concerning, considering the outsized portion of the Federal Budget currently allocated to healthcare spending, which is forecast to rise in the coming years. A recent article in The Economist, entitled “Looking to Uncle Sam” makes this point and goes further to suggest that Centers for Medicare & Medicaid Services (CMS) actuaries may be underestimating future increases in Medicare and Medicaid spending. • One potential reason CMS actuaries may be underestimating the future costs of Medicare and Medicaid relates to healthcare reform’s effect on employee benefits, and specifically, the 2014 switch to subsidized exchange policies. A recent report by McKinsey & Company estimates that approximately 30% of employers will stop offering employer- sponsored insurance (ESI) when this switch is made, as opposed to the 7% estimated by the Congressional Budget Office. An ESI exodus of this magnitude could cause substantial strain on an already robust government healthcare budget. -

News Release Tel
Bayer Pharma AG 13342 Berlin Germany News Release Tel. +49 30 468-1111 Not intended for U.S. and UK Media www.bayerpharma.com Portola Pharmaceuticals Announces Initial Phase II Results Demonstrating Dose-Dependent Reversal of Bayer’s Xarelto® Anticoagulation Activity with Andexanet Alfa (PRT4445) Data set with additional dosing cohorts to be presented at 55th American Society of Hematology (ASH) Annual Meeting and Exposition Berlin, Germany, November 11, 2013 – Bayer HealthCare announced today that initial results from a Phase II proof-of-concept study of Portola Pharmaceuticals’ andexanet alfa, an investigational Factor Xa inhibitor antidote, in healthy volunteers who were administered Bayer’s novel oral anticoagulant Xarelto® (rivaroxaban) have been accepted for presentation at the 55th American Society of Hematology (ASH) Annual Meeting and Exposition, which is being held in New Orleans, LA, USA, from December 7-10, 2013. Initial results from the first two dosing cohorts of the study, submitted by Portola Pharmaceuticals and now published online on the ASH website, demonstrated that andexanet alfa is able to dose-dependently reverse the anticoagulant effects of Xarelto. In addition, no serious adverse events were reported. These data, as well as data from additional cohorts evaluating higher doses of andexanet alfa, will be presented in a poster session on December 9. “Xarelto is a highly effective anticoagulant, and in previous Phase III studies has been shown to significantly reduce the risk of the most concerning bleeding events compared to warfarin. In rare emergency situations when the normalization of blood clotting becomes necessary, stopping Xarelto would allow for normalization of coagulation parameters within one day – this is as effective as giving Vitamin K to patients receiving warfarin,” said Kemal Malik, M.D., Member of the Bayer HealthCare Executive Committee and Head of Global Development. -

Low Discontinuation Rate and Side-Effect Burden After Switching to Cladribine Tablets: Canadian Experience from the Advevatm Patient Support Program
Low discontinuation rate and side-effect burden after switching to cladribine tablets: Canadian experience from the advevaTM patient support program Jiwon Oh1, Paul Giacomini2, Virginia Devonshire3, Fraser Clift4, Caroline Lemieux5, Meritxell Sabidó6, Arthur Allignol6, Mark S. Freedman7 1Division of Neurology, Department of Medicine, St Michael's Hospital, University of Toronto, Toronto, ON, Canada. 2Department of Neurology, Montreal Neurological Institute, McGill University, Montreal, QC, Canada. 3Division of Neurology, Department of Medicine, University of British Columbia MS/NMO Center, Vancouver, BC, Canada. 4Department of Neurology, Memorial University of Newfoundland, St. John's, Newfoundland and Labrador, Canada. 5EMD Inc., Mississauga, Canada; a business of Merck KGaA, Darmstadt, Germany. 6Global Epidemiology Department, Merck KGaA, Darmstadt, Germany. 7Department of Medicine, Division of Neurology, Ottawa Hospital Research Institute, University of Ottawa, Ottawa, ON, Canada. ACTRIMS-ECTRIMS 2020 Virtual Congress | 11-13 September DISCLOSURES This study was sponsored by EMD Inc., Canada (a business of Merck KGaA, Darmstadt, Germany), who reviewed and provided feedback on the poster. The authors had full control of the poster, and provided their final approval of all content Jiwon Oh has received research support from Biogen-Idec, Roche, and EMD Serono and has received personal compensation for consulting from EMD Serono, Sanofi-Genzyme, Biogen-Idec, Roche, Celgene, and Novartis Paul Giacomini has received research or educational -

Adding Cetuximab to Paclitaxel and Carboplatin for First-Line
www.nature.com/bjc ARTICLE Clinical Study Adding cetuximab to paclitaxel and carboplatin for first-line treatment of carcinoma of unknown primary (CUP): results of the Phase 2 AIO trial PACET-CUP Gunnar Folprecht1, Karolin Trautmann1, Alexander Stein2, Gerdt Huebner3, Michael Stahl4, Stefan Kasper5, Albrecht Kretzschmar6, Claus-Henning Köhne7, Viktor Grünwald 8,9, Ralf-Dieter Hofheinz10, Katharina Schütte1, Harald Löffler11, Carsten Bokemeyer2, Alwin Krämer12 and Arbeitsgemeinschaft Internistische Onkologie (AIO) - CUP Group BACKGROUND: Patients with carcinoma of unknown primary (CUP) have a dismal prognosis, even when treated with multi-agent chemotherapy. We hypothesised that adding the epidermal growth-factor receptor (EGFR) inhibitor cetuximab to standard first-line chemotherapy with paclitaxel and carboplatin would improve PFS and RR in unfavourable CUP. METHODS: This open-labelled, multicentre Phase 2 study included patients with unfavourable, untreated adeno- or undifferentiated CUP. Patients were randomised to receive either paclitaxel/carboplatin (group A) or paclitaxel/carboplatin plus cetuximab (group B) every 3 weeks for a maximum of 6 cycles followed by cetuximab maintenance in group B. The primary endpoint was PFS in the two groups. Secondary endpoints were RR, toxicity and overall survival (OS). RESULTS: One-hundred-and-fifty patients were randomised (group A = 72, group B = 78). The median PFS and OS for all patients were 3.8 and 8.1 months (95% confidence interval (CI): 2.9–4.8 and 6.8–9.5). There was no significant difference in PFS (3.7 vs 4.6 months, HR 0.98) or OS (8.1 vs 7.4, HR 1.1) between the two treatment groups.