IAS Durban Talk Lcorey July 19 Final Version
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The CAB Bulletin HIV Vaccines and the Community
The CAB Bulletin HIV Vaccines and the Community Planning for PrEP My First Time By Genevieve Meyer, HVTN Community Education Unit By Dino Martino, On November 23rd, 2010, the results of the iPrEx study were released. The Orlando, FL CAB member. 2,499-person study demonstrated that a daily dose of oral Truvada®, (a With nervous excitement I accepted combination of two antiretroviral medications, emtricitabine and tenofovir) could the offer to attend my first HVTN reduce new infections of HIV in gay men, transwomen and other men who have conference. As a member of the sex with men (MSM) by an average of 43.8%. The HVTN salutes the sponsors, newly formed CAB in Orlando, this study team, and volunteers in the 11 sites throughout Brazil, Ecuador, Peru, South Africa, Thailand and the United States who contributed to this study’s success. was another “first time” opportu- nity in a series of events that I have The results of the iPrEx study have added increased vigor to the HVTN’s search had the pleasure to be a part of in for a safe and effective HIV vaccine. One central question being asked at the HVTN support of the work of the HVTN. right now is what these results mean for participants in HVTN 505, a study which is also enrolling MSM and transwomen who are at risk of contracting HIV. As a pharmacist for nearly two de- cades, scientific conferences are not The Network has set up a working group to solicit feedback from community new to me; still, each one brings stakeholders about possible changes to HVTN 505 based on the iPrEx results. -
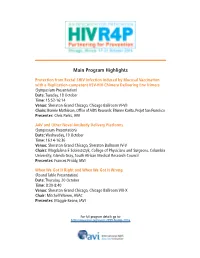
IAVI & Partners' Presentations at HIV R4P 2016
Main Program Highlights Protection from Rectal SHIV Infection Induced by Mucosal Vaccination with a Replication-competent VSV-HIV Chimera Delivering Env Trimers (Symposium Presentation) Date: Tuesday, 18 October Time: 15:52-16:14 Venue: Sheraton Grand Chicago, Chicago Ballroom VI-VII Chairs: Bonnie Mathieson, Office of AIDS Research; Etienne Karita, Projet San Francisco Presenter: Chris Parks, IAVI AAV and Other Novel Antibody Delivery Platforms (Symposium Presentation) Date: Wednesday, 19 October Time: 16:14-16:36 Venue: Sheraton Grand Chicago, Sheraton Ballroom IV-V Chairs: Magdalena E Sobieszczyk, College of Physicians and Surgeons, Columbia University; Glenda Gray, South African Medical Research Council Presenter: Frances Priddy, IAVI When We Got It Right and When We Got It Wrong (Round Table Presentation) Date: Thursday, 20 October Time: 8:30-8:40 Venue: Sheraton Grand Chicago, Chicago Ballroom VIII-X Chair: Mitchell Warren, AVAC Presenter: Maggie Keane, IAVI For full program details go to: http://www.iavi.org/events/599-hivr4p-2016 Satellite Symposium HIV Vaccine Design and Development Partnerships in Africa: Showcasing African-led Basic HIV Prevention Science Research Monday 17 October 2016, 8:30 - 12:30 Sheraton Grand Chicago, Chicago Ballroom IX Refreshments provided This session will bring together African and international scientists, policy makers, advocates and institutions involved in HIV prevention research. They will take a look at current design and development partnership models to identify success factors, gaps and opportunities for enhanced collaborations, as well as young scientists. Presenters and participants will be invited to share their ideas of the next priorities for African HIV prevention research. These will be discussed in a panel discussion on the way forward. -

Antibody Fc Effector Functions and Igg3 Associate with Decreased HIV-1 Risk
RESEARCH ARTICLE The Journal of Clinical Investigation Antibody Fc effector functions and IgG3 associate with decreased HIV-1 risk Scott D. Neidich,1 Youyi Fong,2,3,4 Shuying S. Li,2,3 Daniel E. Geraghty,5 Brian D. Williamson,4 William Chad Young,2 Derrick Goodman,1 Kelly E. Seaton,1 Xiaoying Shen,1 Sheetal Sawant,1 Lu Zhang,1 Allan C. deCamp,2 Bryan S. Blette,6 Mengshu Shao,2 Nicole L. Yates,1 Frederick Feely,1 Chul-Woo Pyo,3 Guido Ferrari,1,7,8 HVTN 505 Team,9 Ian Frank,10 Shelly T. Karuna,3 Edith M. Swann,11 John R. Mascola,12 Barney S. Graham,12 Scott M. Hammer,13 Magdalena E. Sobieszczyk,13 Lawrence Corey,3 Holly E. Janes,2,3,4 M. Juliana McElrath,3 Raphael Gottardo,2,3 Peter B. Gilbert,2,3,4 and Georgia D. Tomaras1,7,8,14 1Duke Human Vaccine Institute, Duke University, Durham, North Carolina, USA. 2Statistical Center for HIV/AIDS Research and Prevention, 3Vaccine and Infectious Disease Division, Fred Hutchinson Cancer Research Center, Seattle, Washington, USA. 4Department of Biostatistics, University of Washington, Seattle, Washington, USA. 5Clinical Research Division, Fred Hutchinson Cancer Research Center, Seattle, Washington, USA. 6Department of Biostatistics, University of North Carolina Gillings School of Global Public Health, Chapel Hill, North Carolina, USA. 7Department of Surgery and 8Department of Molecular Genetics and Microbiology, Duke University, Durham, North Carolina, USA. 9The HVTN 505 Team is detailed in the Supplemental Acknowledgments. 10Division of Infectious Diseases, Perelman School of Medicine, University of Pennsylvania, Philadelphia Pennsylvania, USA. 11Division of AIDS and 12Vaccine Research Center, National Institute of Allergy and Infectious Diseases (NIAID), NIH, Bethesda, Maryland, USA. -

Safety and Immunogenicity of a Recombinant Adenovirus Serotype
C S & lini ID ca A l f R o e l s Fuchs et al., J AIDS Clin Res 2015, 6:5 a e n a r r u c o h J AIDS & Clinical http://dx.doi.org/10.4172/2155-6113.1000461 ISSN: 2155-6113 Research Research Article Open Access Safety and Immunogenicity of a Recombinant Adenovirus Serotype 35-Vectored HIV-1 Vaccine in Adenovirus Serotype 5 Seronegative and Seropositive Individuals Jonathan D Fuchs1,2,*, Pierre-Alexandre Bart3, Nicole Frahm4, Cecilia Morgan4, Peter B Gilbert4, Nidhi Kochar4, Stephen C DeRosa4, Georgia D Tomaras5, Theresa M Wagner1, Lindsey R Baden6, Beryl A Koblin7, Nadine G Rouphael8, Spyros A Kalams9, Michael C Keefer10, Paul A Goepfert11, Magdalena E Sobieszczyk12, Kenneth H Mayer13, Edith Swann14, Hua-Xin Liao5, Barton F Haynes5, Barney S Graham15 and M Juliana McElrath4 for the NIAID HIV Vaccine Trials Network 1Population Health Division, San Francisco Department of Public Health, San Francisco, CA, USA 2Department of Medicine, University of California, San Francisco, San Francisco, USA 3Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland 4Vaccine and Infectious Disease Division, Fred Hutchinson Cancer Research Center, Seattle, WA, USA 5Human Vaccine Institute, Duke University, Durham, NC, USA 6Division of Infectious Disease, Brigham and Women’s Hospital, Boston, MA, USA 7Laboratory of Infectious Disease Prevention, New York Blood Center, New York, NY, USA 8The Hope Clinic, Division of Infectious Diseases, Emory University, Atlanta, GA, USA 9Infectious Diseases Division, Vanderbilt University School of Medicine, Nashville, -

(Sexpro) HIV Risk Prediction Model for Men Who Have Sex with Men in the United States
Title: Development and Validation of the Personalized Sexual Health Promotion (SexPro) HIV Risk Prediction Model for Men Who Have Sex with Men in the United States. Authors Title Email Site Hyman Scott [email protected] Bridge HIV, San Francisco Department of (corresponding) Public Health, San Francisco, California Eric Vittinghoff [email protected] University of California, San Francisco, San Francisco, CA Risha Irvin [email protected] John’s Hopkins School of Medicine, Baltimore, Maryland Albert Liu [email protected] Bridge HIV, San Francisco Department of Public Health, San Francisco, CA LaRon Nelson [email protected] University of Rochester. Rochester, New er.edu York Carlos Del Rio [email protected] Emory University, Atlanta, Georgia Manya Magnus [email protected] George Washington University, Washington, District of Columbia Sharon [email protected] Columbia University, New York, New Mannheimer York Sheldon Fields [email protected] Charles Drew School of Medicine, Los Angeles, California Irene Kuo [email protected] George Washington University, Washington, District of Columbia Steve Shoptow [email protected] University of California, Los Angeles, California Beatrice [email protected] Instituto de Pesquisa Clinica Evandro Grinsztejn Chagas (IPEC), Rio de Janeiro, Brazil Jorge Sanchez [email protected] Asociacion Civil Impacta Salud y Educacion, Lima, Peru Steven [email protected] Fred Hutchinson Cancer Research Center, Wakefield Seattle, Washington Jonathan Fuchs [email protected] -

Advancing Toward HIV-1 Vaccine Efficacy Through the Intersections of Immune Correlates
Vaccines 2014, 2, 15-35; doi:10.3390/vaccines2010015 OPEN ACCESS vaccines ISSN 2076-393X www.mdpi.com/journal/vaccines Review Advancing Toward HIV-1 Vaccine Efficacy through the Intersections of Immune Correlates Georgia D. Tomaras 1,* and Barton F. Haynes 2 1. Departments of Surgery, Immunology, and Molecular Genetics and Microbiology, Duke Human Vaccine Institute, Durham, NC 27710, USA 2. Departments of Medicine and Immunology, Duke Human Vaccine Institute, Durham, NC 27710, USA * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +1-919-681-5598; Fax: +1-919-684-5230. Received: 29 October 2013; in revised form: 29 October 2013 / Accepted: 9 December 2013 / Published: 27 December 2013 Abstract: Interrogating immune correlates of infection risk for efficacious and non-efficacious HIV-1 vaccine clinical trials have provided hypotheses regarding the mechanisms of induction of protective immunity to HIV-1. To date, there have been six HIV-1 vaccine efficacy trials (VAX003, Vaxgen, Inc., San Francisco, CA, USA), VAX004 (Vaxgen, Inc.), HIV-1 Vaccine Trials Network (HVTN) 502 (Step), HVTN 503 (Phambili), RV144 (sponsored by the U.S. Military HIV Research Program, MHRP) and HVTN 505). Cellular, humoral, host genetic and virus sieve analyses of these human clinical trials each can provide information that may point to potentially protective mechanisms for vaccine-induced immunity. Critical to staying on the path toward development of an efficacious vaccine is utilizing information from previous human and non-human primate studies in concert with new discoveries of basic HIV-1 host-virus interactions. One way that past discoveries from correlate analyses can lead to novel inventions or new pathways toward vaccine efficacy is to examine the intersections where different components of the correlate analyses overlap (e.g., virus sieve analysis combined with humoral correlates) that can point to mechanistic hypotheses. -

The CAB Bulletin HIV Vaccines and the Community in This Issue: S
The CAB Bulletin HIV Vaccines and the Community In this Issue: S. Africa CAB Retreat 2 CROI, GCAB Elections 3 Full Group Meeting 4-5 Honors & Awards 6-7 Calls & Announcements 8 From Unique Paths, Hope Takes Action— The Community Education Unit Reflections on the U.S./Swiss CAB Retreat Welcomes Niles Eaton By Reese Aaron Isbell, San Francisco CAB member Those who attended the Full Group Editor’s note on the CAB Retreats: From April 9-11, 2010 the CEU conducted a Meeting were introduced to the new U.S./Swiss CAB Retreat in Seattle, Washington. It was similar in format to the manager of the HVTN Community South African CAB retreat (see article by Siyabonga Nzimande in this issue): a Education Unit (CEU), Niles Eaton. train-the-trainer approach where CAB members worked with staff from the CEU to Niles may be new to the CEU but he present on topics such as an Introduction to Vaccinology, Introduction to Research is certainly not new to community Ethics, How to Read a Protocol, Vaccine-Induced Seropositivity, and many more. education or to the HVTN. Niles has Originally scheduled for June, 2010, the Latin American and Caribbean CAB spent the last seven years as a Clinical Retreat will take place in late Trials Manager and is incredibly 2010 or early 2011. “We all had two important knowledgeable about site operations We arrived separately and things in common: we were and structures. we ranged in age, race, Prior to joining creed and color. We were volunteers, and we were the HVTN, Niles gay, bi, straight, single, part of a world-wide effort to spent seven married (legally and eradicate HIV/AIDS.” years as a study one-day-soon-to-be). -

HVTN CAB Bulletin HIV Vaccines and the Community
HVTN CAB Bulletin HIV Vaccines and the Community In this Issue: Cape Town CAB Member Gets Published 2 HVAD Around the World 3 HVTN Conference Highlights 4 Welcome Jim Maynard! The Global CAB Welcomes David The Community Galetta as New Co-Chair Education Unit By Carrie Schonwald, Community Education Unit welcomed Jim Maynard as the new Associate Director We would like to announce the election of for Community Reverend David Galetta as International Development GCAB Co-Chair. David is currently the and Recruitment CAB Chairperson of the Desmond Tutu (overseeing both HIV Foundation in Cape Town, South Jim Maynard, Associ- ate Director for Com- Community Education Africa, where he has been a CAB member munity Development and Communications) since 2004. Rev. Galetta graduated with a & Recruitment. on May 16. Prior to the Post Graduate Diploma in International HVTN, Jim spent over Research Ethics from the University of Cape David Galetta, new international GCAB 12 years at the Fenway Institute (part Town in 2009 and serves on their Human Co-Chair. of Fenway Health) where he served as Sciences Research Ethics Committee as the Associate Director for Community …continues on page 7 Engagement. Jim brings a wealth of knowledge and experience gained during his years working with HVTN trials HVTN 505 Expands in Size and Scope as well as the HIV Prevention Trials Network (HPTN), the Microbicide Trials By Rick Church, Rich Trevino, Coco Alinsug, Jason Roberts (Community Network (MTN) and the Adolescent Trials members of the HVTN 505 protocol team) and Gail Broder, HVTN Community Network (ATN). His team leadership, Education Unit site perspective, depth of experience, and relentlessly positive energy will be a welcome addition the Core team. -

Ongoing and Planned Trials of Preventive Hiv/Aids Vaccines (May 2012)
ONGOING AND PLANNED TRIALS OF PREVENTIVE HIV/AIDS VACCINES (MAY 2012) Vaccine Sponsor/Funder/ Number of Status / Expected Trial 1 Phase Start Date Vaccine(s) 3 Trial Site 2 Clade abbreviation 3 Developer 2 Participants Completion Phase IIb (safety and efficacy) US (Nashville, TN; Birmingham, AL; Los Angeles, CA; San Francisco, CA; Denver, CO; Orlando, FL; Atlanta, VRC-HIVDNA016-00-VP; GA; Chicago, IL; DNA VRC-HIVADV014-00-VP Bethesda, MD; Boston, Ongoing / Expected HVTN 505 Phase IIb June 2009 DAIDS, NIAID, VRC 2,200 A, B, C Ad5 Prime: VRC-HIVDNA016- MA; New York, NY; 2013 00-VP Rochester, NY; Cleveland, OH; Philadelphia, PA; Dallas, TX; Houston, TX; Annandale, VA; Seattle, WA) Phase II (safety, adherence, acceptability, feasibility) ANRS 149 September DNA GTU-MultiHIV B DNA and Planned / Expected Phase II ANRS France (Créteil) 105 B LIGHT 2012 Lipopeptide LIPO-5 vaccines December 2014 ALVAC-HIV (vCP1521) U.S. Army Medical Canarypox Priming With VaxGen RV 305 Phase II March 2012 Research and Thailand (Chon Buri) 162 Ongoing / June 2013 gp120 B/E (AIDSVAX B/E) gp120 Materiel Command Boosting JS7 plasmid DNA and MVA62B vaccine Peru (Lima), US Ongoing, fully enrolled administered as (1) DNA January DNA DAIDS, GeoVax Labs (Birmingham, AL; San / August 2012, long- HVTN 205 Phase IIa at months 0 and 2 and 299 B 2009 Inc. Francisco, CA; New York, term follow-up Aug MVA MVA at months 4 and 6 NY; Seattle, WA) 2014 or (2) MVA at months 0, 2 and 6 Phase I/II and Ib (safety, adherence, acceptability, feasibility) January Modified Vaccinia Karolinska -

Intentions to Use Pre-‐Exposure Prophylaxis Among Current Phase
Intentions to use pre-exposure prophylaxis among current phase 2B preventive HIV-1 vaccine efficacy trial participants Jonathan D. Fuchs, MD, MPH,1,2 Magdalena E. Sobieszczyk, MD, MPH,3 Tamra Madenwald, MA, MPH,4 Doug Grove,5 Shelly T. Karuna, MD,4 Michele Andrasik, PhD,4 Adam Sherwat, MD,6 Gail Broder,4 Kenneth Mayer, MD,7 Beryl Koblin, PhD,8 and Scott Hammer, MD3 ; HVTN 505 Protocol Team 1San Francisco Department of Public Health 2Department of Medicine, University of California, San Francisco 3Dept. of Medicine, Division of Infectious Diseases, Columbia University College of Physicians and Surgeons 4HIV Vaccine Trials Network, Fred Hutchinson Cancer Research Center 5Statistical Center for HIV/AIDS Research and Prevention, Fred Hutchinson Cancer Research Center 6National Institutes of Allergy and Infectious Diseases, Bethesda, Maryland 7 Fenway Health and the Division of Infectious Diseases, Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School 8Laboratory of Infectious Disease Prevention, Lindsley F. Kimball Research Institute, New York Blood Center Correspondence and request for reprints: Jonathan Fuchs, MD, MPH, San Francisco Department of Public Health, 25 Van Ness Ave. Suite 100, San Francisco, CA 94102, Email: tel. (415) 437-7409, fax (415) 431-7029; email: [email protected] Preliminary analyses were presented at AIDS Vaccine 2011, Bangkok, Thailand Conflicts of Interest and Source of Funding: The HVTN is supported through a cooperative agreement with the National Institute of Allergy and Infectious Diseases (AI068614AI068635) which supports TM, DG, SK, MA, and GB. JF is supported under a Division of AIDS CTU award (UO1AI069496); MS and SH are supported under CTU and CTSA awards (UO1AI69470, UL1RR024156); KM is supported under CTU awards (UM1AI069480-05 and UO1AI069412) and unrestricted research grant support from Gilead Sciences, Inc. -

The HVTN: Strategic Accomplishments of the First Decade and Beyond Tracey Day, Cecilia Morgan, Adi Ferrara, and Jim Kublin
a Publication of the HIV Vaccine Trials Network VOLUME 3, ISSUE 2 | MARCH, 2012 Welcome to a new edition of the Our featured article in this issue is a HVTNews, the newsletter of the HIV look back at the Network’s achieve- Vaccine Trials Network. Our newslet- ments in 12 years of operation, and ter’s mission is to provide timely up- the impact it had on the HIV vaccine dates on the science of HIV vaccines, field. and the science of the HVTN. To that end, this issue features discussions that The search for an HIV vaccine is as include innate immunity studies at relevant and urgent today as it was at the HVTN, the possible impact of the the outset of the epidemic. We hope RV144 Correlates Analyses on future this issue gives you a glimpse of the vaccine trials, and the Network’s myriad ways in which the HVTN ongoing commitment to its study par- pursues our ultimate goal -- eradica- ticipants via our VISP testing service. tion with vaccination. Post RV144 Selection of gp120 [p. 8]. Figure of HIV-1 gp120 Env protein (red), bound to CD4 (yellow) and 17b antibody (blue) provided by Jonathan Stuckey, Vaccine Research Center, NIAID, NIH. The HVTN: Strategic Accomplishments of the First Decade and Beyond Tracey Day, Cecilia Morgan, Adi Ferrara, and Jim Kublin The development of an effective HIV Streamlined Protocol has been streamlining the protocol vaccine is one of humanity’s greatest Development Process development and implementation scientific challenges. In acknowledg- process. This has been achieved largely ing that the path to an effective HIV Before a clinical trial can begin, a through efforts to bring stakeholders vaccine will likely require numerous trial protocol outlining the protocol’s to the table at the appropriate time iterative steps, the HVTN has aimed objectives, target population, and con- and ensure that all support opera- to improve the process of designing, duct must be approved. -

2012 NIAID Jordan Report
THE JORDAN REPORT ACCELERATED DEVELOPMENT OF VACCINES 2012 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health National Institute of Allergy and Infectious Diseases Images on cover, from the top: Courtesy of the US Centers for Disease Control and Prevention; istock.com; Courtesy of the National Library of Medicine; Courtesy of MedImmune THE JORDAN REPORT ACCELERATED DEVELOPMENT OF VACCINES 2012 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health National Institute of Allergy and Infectious Diseases NIH Publication No. 11-7778 January 2012 www.niaid.nih.gov ADDITIONAL RESOURCES National Institute of Allergy and Infectious Diseases, www.niaid.nih.gov Vaccines.gov: your best shot at good health, www.vaccines.gov Centers for Disease Control and Prevention: Immunization Schedules, www.cdc.gov/vaccines/recs/schedules/ Table of Contents INTRODUCTION VACCINE UPDATES Foreword by Anthony S. Fauci, M.D. ......................................... 3 Dengue M. Cristina Cassetti, Ph.D. .......................................................... 95 Tribute by Carole A. Heilman, Ph.D. ......................................... 5 HIGHLIGHT BOX Vaccine Against Chikungunya Virus in Development EXPERT ARTICLES Gary J. Nabel, M.D., Ph.D. and Ken Pekoc ......................... 97 Vaccinomics and Personalized Vaccinology Severe Acute Respiratory Syndrome Gregory A. Poland, M.D., Inna G. Ovsyannikova, Ph.D. and Frederick J. Cassels, Ph.D. ............................................................ 98 Robert M. Jacobson, M.D. .............................................................11 HIGHLIGHT BOX Sex Differences in Immune Responses to Vaccines Vaccine Delivery Technologies Col. Renata J. M. Engler, M.D. and Mary M. Klote, M.D. ....... 19 Martin H. Crumrine, Ph.D. ................................................. 105 Immunization and Pregnancy West Nile Virus Flor M. Munoz, M.D. .................................................................. 27 Patricia M. Repik, Ph.D.