Gastrointestinal System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Abdominal Wall Defect
Abdominal wall defect Description An abdominal wall defect is an opening in the abdomen through which various abdominal organs can protrude. This opening varies in size and can usually be diagnosed early in fetal development, typically between the tenth and fourteenth weeks of pregnancy. There are two main types of abdominal wall defects: omphalocele and gastroschisis. Omphalocele is an opening in the center of the abdominal wall where the umbilical cord meets the abdomen. Organs (typically the intestines, stomach, and liver) protrude through the opening into the umbilical cord and are covered by the same protective membrane that covers the umbilical cord. Gastroschisis is a defect in the abdominal wall, usually to the right of the umbilical cord, through which the large and small intestines protrude (although other organs may sometimes bulge out). There is no membrane covering the exposed organs in gastroschisis. Fetuses with omphalocele may grow slowly before birth (intrauterine growth retardation) and they may be born prematurely. Individuals with omphalocele frequently have multiple birth defects, such as a congenital heart defect. Additionally, underdevelopment of the lungs is often associated with omphalocele because the abdominal organs normally provide a framework for chest wall growth. When those organs are misplaced, the chest wall does not form properly, providing a smaller than normal space for the lungs to develop. As a result, many infants with omphalocele have respiratory insufficiency and may need to be supported with a machine to help them breathe ( mechanical ventilation). Rarely, affected individuals who have breathing problems in infancy experience recurrent lung infections or asthma later in life. -

Hospital Readmission Among Infants with Gastroschisis
Journal of Perinatology (2011) 31, 546–550 r 2011 Nature America, Inc. All rights reserved. 0743-8346/11 www.nature.com/jp ORIGINAL ARTICLE Hospital readmission among infants with gastroschisis AP South1,2, JJ Wessel1,2, A Sberna1, M Patel1 and AL Morrow1 1Division of Neonatology, Perinatal Institute, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA and 2Intestinal Rehabilitation Program, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA Introduction Objective: Infants with gastroschisis have significant perinatal morbidity Gastroschisis is a congenital abdominal wall defect that results in including long hospitalizations and feeding intolerance. Two thirds are evisceration of the bowel into the amniotic space. The birth premature and 20% are growth restricted. Despite these known risk factors prevalence is increasing, affecting B4.5 per 10 000 births.1 While for post-natal complications, little is known about readmission for infants in-hospital morbidity and mortality are well described, there is with gastroschisis. Our objective was to determine the frequency and limited information regarding post-discharge outcomes. Infants indication for hospital readmission after initial discharge among infants with gastroschisis have multiple risk factors for poor long-term with gastroschisis. outcome, including prematurity in two thirds,2 and poor in utero Study Design: Retrospective cohort study. All surviving infants treated growth in 20%.3 Despite absence of extreme prematurity in most for gastroschisis at Cincinnati Children’s Hospital Medical Center, born cases, all infants with gastroschisis are at risk for the development between January 2006 and December 2008 were included. Main outcome of necrotizing enterocolitis with subsequent bowel injury or loss. -

11 Visceral and Parietal Anomalies
6505 BIOL 5720 − INTRODUCTION TO FETAL MEDICINE 11. VISCERAL AND PARIETAL ANOMALIES Arlet G. Kurkchubasche, M.D. Francois I. Luks, M.D. ABDOMINAL WALL DEFECTS Definitions - Omphalocele (also called exomphalos) § Defect is central, involving the umbilicus § Often covered by a membrane, “protecting” viscera; membrane may be ruptured § >30 % have associated anomalies - Chromosomal anomalies: trisomy 18 - “Upper midline” defects: Pentalogy of Cantrell (including heart, pericardium, pleural) - “Lower midline” defects: cloacal exstrophy § Etiology: depends on type; unclear - Gastroschisis (laparoschisis) § Defect is always too the side of an intact umbilicus; usually right of midline § Never covered by a membrane § Associated anomalies are rare, except (presumably secondary) intestinal ones (atresia) § Correlation with young maternal age § 4-5 times more common than omphalocele Diagnosis - Ultrasound very sensitive, and highly specific: § Position of defect and umbilical cord insertion (omphalocele vs. gastroschisis) § Difficult < 16 weeks; not possible < 12 weeks (‘physiologic’ omphalocele at 8-11 wk) § Importance of finding associated anomalies: - Chromosomal (amniocentesis) (omphalocele) - Heart, bladder, pelvis (exstrophy), limbs: omphalocele - Major limb/body wall deformities: rare form of severe amniotic band syndrome sometimes associated with gastroschisis – highly lethal 1 BIOL 6505 § Gastrointestinal anomalies: intestinal loop distension not specific/sensitive for atresia § Grading: “giant” omphalocele contains liver; small omphalocele = “hernia of the cord” - Alpha-fetoprotein (AFP) elevated (amniotic fluid and maternal serum): reflects ‘leakage’ of body proteins through any breach in fetal skin: gastroschisis, spina bifida Prenatal management - Alterations in time, place and mode of delivery § Decision to deliver in tertiary center (with neonatal ICU and surgical services) § C/Section:usually not necessary, except for giant omphalocele (liver trauma) § Early delivery: - Controversial. -

Small Bowel Obstruction After Laparoscopic Roux-En-Y Gastric Bypass Presenting As Acute Pancreatitis: a Case Report
Netherlands Journal of Critical Care Submitted January 2018; Accepted April 2018 CASE REPORT Small bowel obstruction after laparoscopic Roux-en-Y gastric bypass presenting as acute pancreatitis: a case report N. Henning1, R.K. Linskens2, E.E.M. Schepers-van der Sterren3, B. Speelberg1 Department of 1Intensive Care, 2Gastroenterology and Hepatology, and 3Surgery, Sint Anna Hospital, Geldrop, the Netherlands. Correspondence N. Henning - [email protected] Keywords - Roux-en-Y, gastric bypass, pancreatitis, pancreatic enzymes, small bowel obstruction, biliopancreatic limb obstruction. Abstract Small bowel obstruction is a common and potentially life-threatening bowel obstruction within this complication after laparoscopic Roux-en-Y gastric bypass surgery. population, because misdiagnosis We describe a 30-year-old woman who previously underwent can have disastrous outcomes.[1,3-5,7] gastric bypass surgery. She was admitted to the emergency In this report we describe the department with epigastric pain and elevated serum lipase levels. difficulty of diagnosing small Conservative treatment was started for acute pancreatitis, but she bowel obstruction in post- showed rapid clinical deterioration due to uncontrollable pain and LRYGB patients and why frequent excessive vomiting. An abdominal computed tomography elevated pancreatic enzymes scan revealed small bowel obstruction and surgeons performed can indicate an obstruction in an exploratory laparotomy with adhesiolysis. Our patient quickly these patients. The purpose of improved after surgery and could be discharged home. This case this manuscript is to emphasise report emphasises that in post-bypass patients with elevated Figure 1. Roux-en-Y gastric bypass that in post-bypass patients with pancreatic enzymes, small bowel obstruction should be considered ©Ethicon, Inc. -
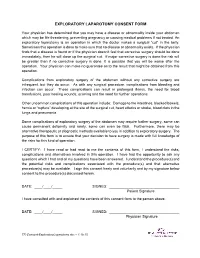
Exploratory Laparotomy.Docx
EXPLORATORY LAPAROTOMY CONSENT FORM Your physician has determined that you may have a disease or abnormality inside your abdomen which may be life threatening, preventing pregnancy or causing medical problems if not treated. An exploratory laparotomy is an operation in which the doctor makes a surgical “cut” in the belly. Sometimes this operation is done to make sure that no disease or abnormality exists. If the physician finds that a disease is found or if the physician doesn’t feel that corrective surgery should be done immediately, then he will close up the surgical cut. If major corrective surgery is done the risk will be greater than if no corrective surgery is done. It is possible that you will be worse after the operation. Your physician can make no guarantee as to the result that might be obtained from this operation. Complications from exploratory surgery of the abdomen without any corrective surgery are infrequent, but they do occur. As with any surgical procedure, complications from bleeding and infection can occur. These complications can result in prolonged illness, the need for blood transfusions, poor healing wounds, scarring and the need for further operations. Other uncommon complications of this operation include: Damage to the intestines, blocked bowels, hernia or “rupture” developing at the site of the surgical cut, heart attacks or stroke, blood clots in the lungs and pneumonia. Some complications of exploratory surgery of the abdomen may require further surgery, some can cause permanent deformity and rarely, some can even be fatal. Furthermore, there may be alternative therapeutic or diagnostic methods available to you in addition to exploratory surgery. -

Abdominal Exploratory and Closure
Abdominal exploratory and closure 10.1 Diagnostic procedures 10.1.1 Paracentesis 10.1.1.1 Paracentesis technique 10.1.2 Enterocentesis 10.1.2.1 Enterocentesis technique 10.2 Opening of the abdominal cavity 10.2.1 Introduction 10.2.2 Position of the animal 10.2.3 Location of incision 10.2.4 Type of incision 10.2.4.1 Through-and-through incision 10.2.4.2 Complete grid Incision 10.2.4.3 Partial grid incision 10.2.5 Laparotomy in the bovine 10.2.5.1 Indications 10.2.5.2 Through-and-through incision 10.2.5.3 Partial grid incision 10.2.5.4 Complete grid incision 10.2.6 Laparotomy in small ruminants Chapter 10 10.2.7 Laparotomy in the horse 10.2.7.1 Indications 10.2.7.2 The median coeliotomy 10.2.7.3 The paramedian laparotomy 10.2.8 Coeliotomy in the dog and the cat 10.2.8.1 Indications 10.2.8.2 The median coeliotomy 10.2.8.3 The flank or paracostal incision 10.3 Minimally invasive techniques 10.4 Abdominal procedures 10.4.1 The rumen (bovine, small ruminants) 10.4.1.1 Introduction 10.4.1.2 Rumenotomy 10.4.2 The abomasum (bovine) 10.4.3 The stomach (horse, dog and cat) 10.4.3.1 Introduction 10.4.3.2 Gastrotomy in the dog and the cat 10.4.4 The small- and large intestines 10.4.4.1 Introduction 10.4.4.1.1 Simple mechanical ileus 10.4.4.1.2 Strangulating ileus 10.4.4.1.3 Paralytic ileus 10.4.4.2 Diagnostics 10.4.4.3 Therapy 10.4.4.3.1 Enterotomy 10.4.4.3.2 Enterectomy 10.4.5 The bladder 10.4.5.1 Introduction 10.4.5.2 Urolithiasis in bovine and equine 10.4.5.3 Cystotomy in the horse 10.4.5.3.1 Laparocystotomy 10.4.5.3.2 Pararectal cystotomy 10.4.5.4 Urolithiasis in the dog and the cat 10.4.5.5 Cystotomy in the dog and the cat 10.4.6 The uterus 10.4.6.1 Opening and closing of the uterus 10.4.6.2 Ovariectomy and ovariohysterectomy in dog and cat Chapter 10 176 Chapter 10 Abdominal exploratory and closure 10.1 Diagnostic procedures 10.1.1 Paracentesis paracentesis Paracentesis is the puncturing of the abdominal cavity. -

Gastroschisis and Omphalocele
Gastroschisis and Omphalocele The two most common congenital abdominal wall At delivery, the ABC (airway, breathing, circulation) rule defects are gastroschisis and omphalocele. Both involve should be followed for babies with gastroschisis or incomplete closure of the abdominal wall during fetal omphalocele. Immediately afterward, protection of the development, and for both, their cause is unknown. A herniated contents and management of evaporative loss gastroschisis is usually an isolated congenital defect, should be accomplished. Abdominal contents should be whereas a baby with an omphalocele often has chromo- wrapped in warm, saline-soaked gauze and covered with some anomalies, cardiac conditions, and other major birth plastic wrap. Alternatively, the baby should be placed in defects. a sterile bowel bag up to the nipple line. Preventing evap- orative fluid loss is particularly important for the baby A gastroschisis is a herniation of abdominal contents with gastroschisis because of the lack of the protective through a defect in the abdominal wall, usually just to the membranous covering of the abdominal contents. Dili- right of the umbilicus. An omphalocele is a herniation of gent observation of the color and perfusion of the abdom- abdominal contents into the umbilical cord itself. The con- inal contents of a baby with gastroschisis is imperative. tents of a gastroschisis are directly exposed to amniotic The baby should be placed on his or her right side with fluid, whereas the contents of an omphalocele are usually abdominal contents supported with additional gauze or covered with a protective membranous sac. blankets to prevent kinking of the mesentery blood ves- sels. An echocardiogram also should be considered to rule out potential cardiac anomalies (Escobar & Caty, 2016). -

Abdominal Wall Defects—Current Treatments
children Review Abdominal Wall Defects—Current Treatments Isabella N. Bielicki 1, Stig Somme 2, Giovanni Frongia 3, Stefan G. Holland-Cunz 1 and Raphael N. Vuille-dit-Bille 1,* 1 Department of Pediatric Surgery, University Children’s Hospital of Basel (UKBB), 4056 Basel, Switzerland; [email protected] (I.N.B.); [email protected] (S.G.H.-C.) 2 Department of Pediatric Surgery, University Children’s Hospital of Colorado, Aurora, CO 80045, USA; [email protected] 3 Section of Pediatric Surgery, Department of General, Visceral and Transplantation Surgery, 69120 Heidelberg, Germany; [email protected] * Correspondence: [email protected]; Tel.: +41-61-704-27-98 Abstract: Gastroschisis and omphalocele reflect the two most common abdominal wall defects in newborns. First postnatal care consists of defect coverage, avoidance of fluid and heat loss, fluid administration and gastric decompression. Definitive treatment is achieved by defect reduction and abdominal wall closure. Different techniques and timings are used depending on type and size of defect, the abdominal domain and comorbidities of the child. The present review aims to provide an overview of current treatments. Keywords: abdominal wall defect; gastroschisis; omphalocele; treatment 1. Gastroschisis Citation: Bielicki, I.N.; Somme, S.; 1.1. Introduction Frongia, G.; Holland-Cunz, S.G.; Gastroschisis is one of the most common congenital abdominal wall defects in new- Vuille-dit-Bille, R.N. Abdominal Wall borns. Children born with gastroschisis have a full-thickness paraumbilical abdominal Defects—Current Treatments. wall defect, which is associated with evisceration of bowel and sometimes other organs Children 2021, 8, 170. -

Human Milk Versus Formula After Gastroschisis Repair: Effects on Time to Full Feeds and Time to Discharge
Journal of Perinatology (2013) 33, 627–630 & 2013 Nature America, Inc. All rights reserved 0743-8346/13 www.nature.com/jp ORIGINAL ARTICLE Human milk versus formula after gastroschisis repair: effects on time to full feeds and time to discharge JA Kohler Sr, AM Perkins and WT Bass OBJECTIVE: To determine if the choice of enteral feeds after gastroschisis repair relates to the time to achieve full feeds and time to discharge. STUDY DESIGN: A retrospective study of infants with gastroschisis from 2000 to 2010 examined demographics, days at closure, days at initiation of feeds, days to full feeds, time to discharge and length of stay. RESULT: Ninety infants were identified, 22 received (human milk) HM exclusively, 15 were fed 450% HM, 16 were fed o50% HM and 26 were fed only cow milk-based formulas. Infants fed exclusively HM had significantly shorter times to full enteral feedings (median 5 days versus 7 days, P ¼ 0.03). The time from initiation of feedings to hospital discharge, which accounts for initiation age, significantly favored the exclusively HM-fed infants (median 7 days versus 10 days, P ¼ 0.01). CONCLUSION: Exclusive HM feeding after gastroschisis repair decreases time to achieve full enteral feeds and time to discharge. Journal of Perinatology (2013) 33, 627–630; doi:10.1038/jp.2013.27; published online 21 March 2013 Keywords: total parenteral nutrition; parenteral nutrition-associated liver disease; intestinal permeability INTRODUCTION METHODS Gastroschisis is a congenital defect of the ventral abdominal wall. Study population The lesion consists of a small full-thickness periumbilical cleft This retrospective study included all patients who were admitted to the usually to the right of the umbilicus, which allows for the neonatal intensive care unit of the Children’s Hospital of The King’s herniation of abdominal contents into the amniotic sac. -

Gastroschisis
Gastroschisis This guideline was updated in May 2015 by Dr Renuka Bhat with input from members of the New Zealand Maternal Fetal Medicine Network. Background Fetal gastroschisis is usually often diagnosed at Nuchal translucency or routine anomaly scan. Underlying cause is still unknown, but is believed to be related to vascular compromise of the omphalomesenteric artery during embryonic development. Numerous studies have reported a rising incidence of gastroschisis. Risk factors include young maternal age, smoking and use of vasoactive agents. A survival rate of liveborn infants with gastroschisis is 90 – 95%. The risk of intra-uterine fetal death is about 10% and its association with fetal distress is well known. Once the diagnosis is clarified (where possible) options can be discussed with the woman and her support. If the woman continues the pregnancy, continued care with fetal medicine input/ LMC is indicated. The follow-up will depend on the situation. 2015 May Gastroschisis: Objective To guide the accurate diagnosis, investigation and management of women presenting with fetal gastroschisis. To provide a consistent approach to the care of women with fetal gastroschisis which takes into consideration individual women’s views and wishes regarding care plan. 2 Definition • Fetal gastroschisis is defined as full thickness anterior abdominal wall defect with bowel protruding through the defect • It usually occurs on the right side of a normally inserting umbilical cord • The defect is not covered by membrane Differential Diagnosis • Omphalocele and associated syndromes (e.g. Beckwith-Wiedermann, pentalogy of Cantrell) • Amniotic banding • Limb- body wall complex Important History • Age and ethnicity Gastroschisis: May 2015 May Gastroschisis: • Any drug use particularly vaso-active drugs • Past obstetric history, any anomalies / syndromes • Any family history of note. -

Exploratory Laparotomy Following Penetrating Abdominal Injuries: a Cohort Study from a Referral Hospital in Erbil, Kurdistan Region in Iraq
Exploratory laparotomy following penetrating abdominal injuries: a cohort study from a referral hospital in Erbil, Kurdistan region in Iraq Research protocol 1 November 2017 FINAL version Table of Contents Protocol Details .............................................................................................................. 3 Signatures of all Investigators Involved in the Study .................................................... 4 Summary ........................................................................................................................ 5 List of Abbreviations ..................................................................................................... 6 List of Definitions .......................................................................................................... 7 Background .................................................................................................................... 8 Justification .................................................................................................................... 9 Aim of Study .................................................................................................................. 9 Investigation Plan ......................................................................................................... 10 Study Population .......................................................................................................... 10 Data ............................................................................................................................. -

Digestive Endoscopy in Five Decades
■ COLLEGE LECTURES Digestive endoscopy in five decades Peter B Cotton ABSTRACT – The world of gastroenterology scopy. So-called semi-flexible gastroscopes were changed forever when flexible endoscopes cumbersome and used infrequently by only a few became available in the 1960s. Diagnostic and enthusiasts. therapeutic techniques proliferated and entered the mainstream of medicine, not without some Diagnostic endoscopy controversy. Success resulted in a huge service demand, with the need to train more endo- The first truly flexible gastroscope was developed in 1 This paper is scopists and to organise large endoscopy units the USA, following pioneering work on fibre-optic 2 based on the Lilly and teams of staff. The British health service light transmission in the UK by Harold Hopkins. Lecture given at struggled with insufficient numbers of consul- However, commercial production of endoscopes was the Royal College tants, other staff and resources, and British rapidly dominated by Japanese companies, building of Physicians on endoscopy fell behind that of most other devel- on their earlier expertise with intragastric cameras. 12 April 2005 by oped countries. This situation is now being My involvement began in 1968, whilst doing bench Peter B Cotton addressed aggressively, with many local and research with Dr Brian Creamer at St Thomas’ MD FRCP FRCS, national initiatives aimed at improving access and Hospital, London. An expert in coeliac disease (and Medical Director, choice, and at promoting and documenting jejunal biopsy), he opined that gastroscopy might Digestive Disease quality. Many more consultants are needed and become useful and legitimate only if it became pos- Center, Medical some should be relieved of their internal medi- sible to take target biopsy specimens – since no one University of South Carolina, cine commitment to focus on their specialist seriously believed what endoscopists said that they Charleston, USA skills.