HNA Summary 2017 Web.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RDA Riverina Overview 2011 RDA Riverina Connecting Communities, Business & Government to Projects, Programs, Services Funding and Other People
RDA Riverina Overview 2011 RDA Riverina connecting communities, business & government to projects, programs, services funding and other people. A NSW Government Initiative Vision RDA Riverina will be a region renowned for its excellence in all dimensions – economic, social and environmental with emphasis on innovation, life long learning, healthy living and an optimistic outward looking culture based on confidence, resilience and social inclusion. Mission RDA Riverina will build partnerships that facilitate the development of a sustainable region. Hillston CARRATHOOL New South Wales SYDNEY GRIFFITH Hillston COOTAMUNDRA HAY TEMORA CANBERRA LEETONCARRATHOOL New South Wales MURRUMBIDGEE NARRANDERA COOLAMON JUNEE SYDNEY GRIFFITH Wagga Wagga GUNDAGAI COOTAMUNDRA HAY TEMORA CANBERRA WAGGA LEETON LOCKHART WAGGA MURRUMBIDGEE NARRANDERA COOLAMON JUNEE Wagga Wagga GUNDAGAI WAGGA LOCKHART WAGGA www.rdariverina.org.au Contents • Introduction 03 • A message from the Chairman 05 • Organisational Structure 06 • About this Report - Sub Commiitee 07 • Infrastructure 08 • Business Development 10 • Promotion 12 • Environmental Sustainability 15 • All of Government Approach 17 • Building Capacity 21 03 Regional Development Australia Riverina Overview 2011 Introduction Who is Regional Development Australia? Regional Development Australia (RDA) is a Australia, Local Government, Arts & Sport) & the partnership between the Australian, state, State Minister (The Hon. Andrew Stoner MP, NSW territory and local governments to develop and Minster for Trade & Investment). Members have strengthen the regional communities in Australia. a broad and diverse skills base developing local RDA includes the Department of Regional solutions to local problems. Australia, Local Government, Arts & Sport, State In New South Wales there are 14 RDAs. RDA Departments as well as a national network of Riverina is composed of 13 local government 55 committees (RDAs) that were established areas (LGAs): Carrathool, Coolamon, in August 2009. -

Murrumbidgee Regional Fact Sheet
Murrumbidgee region Overview The Murrumbidgee region is home The river and national parks provide to about 550,000 people and covers ideal spots for swimming, fishing, 84,000 km2 – 8% of the Murray– bushwalking, camping and bird Darling Basin. watching. Dryland cropping, grazing and The Murrumbidgee River provides irrigated agriculture are important a critical water supply to several industries, with 42% of NSW grapes regional centres and towns including and 50% of Australia’s rice grown in Canberra, Gundagai, Wagga Wagga, the region. Narrandera, Leeton, Griffith, Hay and Balranald. The region’s villages Chicken production employs such as Goolgowi, Merriwagga and 350 people in the area, aquaculture Carrathool use aquifers and deep allows the production of Murray bores as their potable supply. cod and cotton has also been grown since 2010. Image: Murrumbidgee River at Wagga Wagga, NSW Carnarvon N.P. r e v i r e R iv e R v i o g N re r r e a v i W R o l g n Augathella a L r e v i R d r a W Chesterton Range N.P. Charleville Mitchell Morven Roma Cheepie Miles River Chinchilla amine Cond Condamine k e e r r ve C i R l M e a nn a h lo Dalby c r a Surat a B e n e o B a Wyandra R Tara i v e r QUEENSLAND Brisbane Toowoomba Moonie Thrushton er National e Riv ooni Park M k Beardmore Reservoir Millmerran e r e ve r i R C ir e e St George W n i Allora b e Bollon N r e Jack Taylor Weir iv R Cunnamulla e n n N lo k a e B Warwick e r C Inglewood a l a l l a g n u Coolmunda Reservoir M N acintyre River Goondiwindi 25 Dirranbandi M Stanthorpe 0 50 Currawinya N.P. -
Embracing Change Murray Irrigation Annual Report 2014
Embracing change Murray Irrigation Annual Report 2014 Murray Irrigation Contents At a glance 2 Chairman’s report 4 Chief Executive Officer’s report 6 Year in review 8 Company profile and management team 10 Chapters 01 Customers 12 02 Water availability, usage and efficiency 18 03 Infrastructure 22 04 Financial performance 28 05 Ancillary activities 32 06 People and governance 36 Directors’ report and financial statements 2013/14 44 Directors’ report 46 Financial statements 54 Directors’ declaration 80 Auditor’s independence declaration 81 Independent audit report 82 2014 Murray Irrigation Limited Annual Report The 2014 Murray Irrigation Limited Annual Report is a summary of operations and performance of the company from 1 July 2013 to 30 June 2014. Operations and performance for this period have been measured against the company’s key reporting areas as detailed in the Murray Irrigation Limited 2014 Strategic Plan in addition to meeting our statutory financial reporting responsibilities. The 2014 Murray Irrigation Limited Annual Report provides a concise and comprehensive summary. The objective of this report is to provide information to our shareholders to demonstrate our transparency, accountability and performance. The 2014 Murray Irrigation Limited Annual Report is distributed on request to all shareholders and is available electronically via our website, as per the requirements of our Constitution. Additional copies of the 2014 Murray Irrigation Limited Annual Report can be obtained via: • The Murray Irrigation Limited website www.murrayirrigation.com.au • Visiting the Murray Irrigation offices at Deniliquin and Finley. • Writing to Murray Irrigation Limited, PO Box 528, Deniliquin NSW 2710. Murray Irrigation is on a progressive change journey. -

Supplementary Notice
Supplementary notice SUPPLEMENTARY WATER ACCESS FOR MURRUMBIDGEE 9 November 2020 Department of Planning, Industry & Environment - Water has issued access to supplementary water for the Murrumbidgee River and Yanco/Billabong Creek systems. Recent rainfall from coastal low event has led to elevated tributary inflows. In addition, regulated river (general security) access licence holders may take water during this period of supplementary flows, if the uncontrolled flow (UCF) limits of their accounts permit. Licence holders are reminded that all diversions count towards the annual usage limit of 100% of entitlement (excludes trades into accounts). Customers wishing to access supplementary water / uncontrolled flow must provide a START meter reading and place a complying water order using one of the following options: Accessing WWW.WaterNSW.com.au and registering or logging on to your iWAS account. Faxing your order to 1300 871 447 Emailing your order to [email protected] Telephoning your order to 1300 662 077 During business hours Water order forms are available from the Water NSW web site. Customers are reminded that with the conclusion of supplementary access an END meter reading must be provided, and as regulated flow conditions would resume water orders must be placed in accordance with their licence conditions. WaterNSW will continue to monitor the situation closely and further advice will be issued only if required, on or before Thursday 12 November 2020. For further information contact the Operations Officer, WaterNSW -

Flood Intelligence: What It Is, Why It Matters and How It Is Generated – Lessons from Lockhart and Urana Shire Floods 2010-2012
Floodplain Management Association National Conference 28-31 May 2013 Tweed Heads NSW FLOOD INTELLIGENCE: WHAT IT IS, WHY IT MATTERS AND HOW IT IS GENERATED – LESSONS FROM LOCKHART AND URANA SHIRE FLOODS 2010-2012 M Morgan1 S Yeo2, M Walsh3 1 NSW State Emergency Service, Wollongong, NSW 2 Independent flood risk management consultant, Sydney, NSW 3 Inland Flood Unit, Office of Environment and Heritage, Sydney, NSW Abstract Flood intelligence seeks to describe flood behaviour and its effects on the community. The NSW State Emergency Service (NSW SES) flood intelligence system includes a flood intelligence database, Local Flood Plans, a reference library and associated spatial data. Reliable intelligence is vital for informed decision-making during flood emergencies to minimise risks to the community. Data collection following flooding is a means both for generating new flood intelligence to improve future emergency response and for informing the floodplain management process. Between 2010 and 2012, many communities in South Western NSW experienced the highest floods in decades, if not on record. This provided an ideal opportunity to collect flood data. A case study from Lockhart and Urana Shires shows the benefits of this exercise both for an improved flood intelligence leading to an improved flood response and for input into Flood Studies and Floodplain Risk Management Studies and Plans. Strengths and weaknesses of the various sources of flood data including community questionnaires are outlined. Introduction Between September 2010 and March 2012, areas in South Western NSW experienced record rainfall, associated with a strong La Niña episode which resulted in extensive and frequent flooding through to May 2012. -

Racism Survey: 'Murray and Far West' Statistical Division
Regional response profile- Racism Survey: ‘Murray and Far West’ Statistical Division This page contains information on the attitudes, experiences and demographics of the ‘Murray and Far West’ Statistical Division. There are also links that provide a description of the groupings in this Statistical Division, suggested anti-racism initiatives, and details about the survey. LGAs Albury, Balranald, Broken Hill, Berrigan, Central Darling, Conargo, Corowa Shire, Deniliquin, Greater Hume Shire, Jerilderie, Murray, Tumbarumba, Unincorporated NSW, Urana, Wakool, Wentworth. Grouping A characterisation of the above LGAs is provided through the links above. These characterisations describe the mix of attitudes, demographics and experiences of residents in those areas. The descriptions are followed by a list of suggested anti-racism initiatives which may be useful in those areas. Sample size The sample size for the ‘Murray and Far West’ SD was 84 respondents. This represents 2.6% of the survey respondents from New South Wales (3217) and 0.7% of respondents from all of Australia (12512). 1 1. Racist attitude indicators Table 1.1: Comparison of racist attitudes, ‘Murray and Far West’ Statistical Divisions with total New South Wales and Australian survey, 2001. % of SD Total Total Australia Variation Variation from Nation respondents New South Wales survey% from State survey % Anti-cultural difference1 7.1 8.1 6.5 -1 0.6 Insecurity with difference2 11.9 11.0 9.4 0.9 2.5 Diversity = weak nation3 46.4 46.1 41.1 0.3 5.3 Self identify as racist4 14.3 12.9 -

Boree Creek's Wool Artist the Story of Doris Golder
Boree Creek’s Wool Artist The Story of Doris Golder K-6 Students Boree Creek Public School Creative Catchment Kids Creative Catchment Kids is an initiative of Wirraminna Environmental Education Centre. It aims to improve engagement between our funding partners and school students by providing opportunities for positive and authentic ventures that encourage students to develop creative solutions to agriculture and natural resource management issues. www.wirraminna.org/creative-catchment-kids/ Wirraminna Environmental Education Centre The Wirraminna Environmental Education Centre is located in Burrumbuttock, north of Albury in southern NSW. Since 1995, the centre, which is adjacent to Burrumbuttock Public School, has provided opportunities for discovery and learning about the natural environment, the ecology of the local woodlands and the beauty of native plants. www.wirraminna.org Enviro-Stories Enviro-Stories is an innovative literacy education program that inspires learning about natural resource and catchment management issues. Developed by PeeKdesigns, this program provides students with an opportunity to publish their own stories that have been written for other kids to support learning about their local area. www.envirostories.com.au Boree Creek’s Wool Artist The Story of Doris Golder Authors: Clare Ratcliffe, Luke Westblade, Hannah Patey, Martin Steele, Jock Ratcliffe, Michael Barker-Smith, Lachlan Routley Teacher: Elissa Routley School: : Boree Creek Public School Local Land Heroes - Securing Our Region In 2015, students involved in the Creative Catchment Kids program researched and wrote stories about their ‘Local Land Heroes’ who are involved in pest management in the Murray and Murrumbidgee regions. These heroes are local individuals, couples, a business or industries that have made a difference in their local community by contributing to the management of pest animals and plants. -

Yanco Technical Advisory Group Meeting 3, 12 March 2020, Jerilderie
Yanco Community Advisory Group This project is delivered under the Murray–Darling Basin Plan by the NSW Government, through funding from the Australian Government Department of Agriculture, Water and the Environment. Meeting 3, 12 March 2020, Jerilderie The Yanco Community Advisory Group (YCAG) discussed planning for two Sustainable Diversion Limit Adjustment Mechanism (SDLAM) projects associated with the Yanco Creek System that aim to deliver equivalent environmental outcomes using less water. Yanco Creek Offtake Project Modernising Supply Systems For Effluent Creeks - Murrumbidgee River Project Attended by an independent Chair (Norm McAllister) and representatives from the Yanco Creek and Tributaries Advisory Council (YACTAC) (Tanya Thompson, Bob Crawford), Leeton Shire Council (Jackie Kruger), Narrandera Shire Council (Deputy Mayor David Fahey), Federation Council (Mayor Patrick Bourke), Murrumbidgee Council (Mayor Ruth McRae), Edward River Council (Mayor Norm Brennan), Creek Country Alliance (Richard Sleigh), Colombo Ski Club (Jim Morgan), Murrumbidgee Field Naturalists (Nella Smith) and NSW Farmers Association (Richard Coughlin). Department of Planning, Industry and Environment staff present included David Leslie (Principal Project Officer), David Clarke (Senior Project Officer) and Rod Hardwick (Senior Project Officer). Meeting summary Acknowledgement of Country Presentation and discussion on the Options Evaluation Framework (OEF). The OEF will identify a short list of options for detailed investigation considerate of project objectives, environmental, economic, social and cultural values. The categories, criteria and potential weightings of each was discussed. A visioning exercise was completed for environmental, economic, social and cultural values. This exercise is intended to help determine appropriate weightings and potential new sub- categories in the OEF. The group discussed how best to approach consultation so the community may propose new, and review existing, project options. -

August Newsletter
Yanco Agricultural High School As you sow, so shall you reap Newsletter Private Mail Bag Telephone: 02 69511500 UPCOMING th Friday, 15 August 2014 YANCO, NSW 2703 Fax: 02 69557180 EVENTS Term 3, Week 5 Email: [email protected] 14th August Buses depart NSW CHS RUGBY LEAGUE - AUSTRALIAN CHAMPIONSHIPS DESI weekend th 18 August Buses return from DESI th 19 August Classes resume 22nd -23rd August Condobolin Show nd th 22 - 24 August Hook Line and Sinker @ Hillston 23rd August Ganmain Show th 28 August Supplementary Zac Saddler - NSW CHS photo Day Under 15’s Rugby League team – 29th - 31st August played in the Australian Championships recently Dubbo Allbreeds Heifer Show. YEAR 11 CANDIDATES FOR PREFECT POSITIONS 2015 Fishing Club to Hillston. 30th August Barellan Show 3rd September West Wyalong Show 5th - 7th September CHS Athletics 6th September Narrandera Show 6th - 7th September Shooting group @ Bowral 7th September Condobolin Show 10th September Year 11 Preliminary Exams commence 18th September Year 12 Graduation 2015 st Boys: Sam Larsen, Jock McPherson, Jock Ward, Damian Johnston, Luke Horrobin, Wed 31 January Nathan Morris, Harry Beal, Will Peterson, Mitchell Ryan, Darcy Booth All students return Girls: Natalia Henderson, Rebecca Ritchie, Skye Bensley, Colleen Head, Heidi Johnston, to school. Rose Nevinson, Laura Harris, Georgia Howard, Marnie Whytcross, Jane Arndt, Breanna Carr, Elly Pratt, Elizabeth Moran-Turner PRINCIPAL’S REPORT week in Griffith. The students were very well received at both events It is with great pleasure that I formally announce the successful students who have been elected as the • Our Open and Under 16 Girls Rugby Union 2015 School Prefects. -

Outback NSW Regional
TO QUILPIE 485km, A THARGOMINDAH 289km B C D E TO CUNNAMULLA 136km F TO CUNNAMULLA 75km G H I J TO ST GEORGE 44km K Source: © DEPARTMENT OF LANDS Nindigully PANORAMA AVENUE BATHURST 2795 29º00'S Olive Downs 141º00'E 142º00'E www.lands.nsw.gov.au 143º00'E 144º00'E 145º00'E 146º00'E 147º00'E 148º00'E 149º00'E 85 Campground MITCHELL Cameron 61 © Copyright LANDS & Cartoscope Pty Ltd Corner CURRAWINYA Bungunya NAT PK Talwood Dog Fence Dirranbandi (locality) STURT NAT PK Dunwinnie (locality) 0 20 40 60 Boonangar Hungerford Daymar Crossing 405km BRISBANE Kilometres Thallon 75 New QUEENSLAND TO 48km, GOONDIWINDI 80 (locality) 1 Waka England Barringun CULGOA Kunopia 1 Region (locality) FLOODPLAIN 66 NAT PK Boomi Index to adjoining Map Jobs Gate Lake 44 Cartoscope maps Dead Horse 38 Hebel Bokhara Gully Campground CULGOA 19 Tibooburra NAT PK Caloona (locality) 74 Outback Mungindi Dolgelly Mount Wood NSW Map Dubbo River Goodooga Angledool (locality) Bore CORNER 54 Campground Neeworra LEDKNAPPER 40 COUNTRY Region NEW SOUTH WALES (locality) Enngonia NAT RES Weilmoringle STORE Riverina Map 96 Bengerang Check at store for River 122 supply of fuel Region Garah 106 Mungunyah Gundabloui Map (locality) Crossing 44 Milparinka (locality) Fordetail VISIT HISTORIC see Map 11 elec 181 Wanaaring Lednapper Moppin MILPARINKA Lightning Ridge (locality) 79 Crossing Coocoran 103km (locality) 74 Lake 7 Lightning Ridge 30º00'S 76 (locality) Ashley 97 Bore Bath Collymongle 133 TO GOONDIWINDI Birrie (locality) 2 Collerina NARRAN Collarenebri Bullarah 2 (locality) LAKE 36 NOCOLECHE (locality) Salt 71 NAT RES 9 150º00'E NAT RES Pokataroo 38 Lake GWYDIR HWY Grave of 52 MOREE Eliza Kennedy Unsealed roads on 194 (locality) Cumborah 61 Poison Gate Telleraga this map can be difficult (locality) 120km Pincally in wet conditions HWY 82 46 Merrywinebone Swamp 29 Largest Grain (locality) Hollow TO INVERELL 37 98 For detail Silo in Sth. -
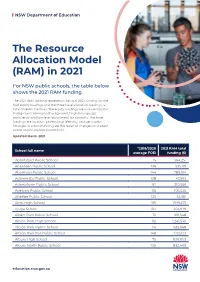
The Resource Allocation Model (RAM) in 2021
NSW Department of Education The Resource Allocation Model (RAM) in 2021 For NSW public schools, the table below shows the 2021 RAM funding. The 2021 RAM funding represents the total 2021 funding for the four equity loadings and the three base allocation loadings, a total of seven loadings. The equity loadings are socio-economic background, Aboriginal background, English language proficiency and low-level adjustment for disability. The base loadings are location, professional learning, and per capita. Changes in school funding are the result of changes to student needs and/or student enrolments. Updated March 2021 *2019/2020 2021 RAM total School full name average FOEI funding ($) Abbotsford Public School 15 364,251 Aberdeen Public School 136 535,119 Abermain Public School 144 786,614 Adaminaby Public School 108 47,993 Adamstown Public School 62 310,566 Adelong Public School 116 106,526 Afterlee Public School 125 32,361 Airds High School 169 1,919,475 Ajuga School 164 203,979 Albert Park Public School 111 251,548 Albion Park High School 112 1,241,530 Albion Park Public School 114 626,668 Albion Park Rail Public School 148 1,125,123 Albury High School 75 930,003 Albury North Public School 159 832,460 education.nsw.gov.au NSW Department of Education *2019/2020 2021 RAM total School full name average FOEI funding ($) Albury Public School 55 519,998 Albury West Public School 156 527,585 Aldavilla Public School 117 681,035 Alexandria Park Community School 58 1,030,224 Alfords Point Public School 57 252,497 Allambie Heights Public School 15 -

Fixing Country Roads Round Two Successful
Fixing Country Roads Rounds 2 & 2.5 Successful Projects List Fixing Country Roads Round 2 Local Government Area(s) Project Name Funding Amount Armidale Dumaresq Council Armidale Dumaresq Council Level 3 Bridge (Now Armidale Regional $95,000 Inspections Council) Bellingen Shire Timber Bridge Capacity Bellingen Shire Council $135,000 Assessment Bombala Shire Council (now Rosemeath Road Widening and Pavement Snowy Monaro Regional $375,000 Strengthening Council) Bombala Shire Council (now Snowy Monaro Regional Upgrade of Regional Tantawangalo Road $150,000 Council) MR 241 Murringo Road Pavement Widening Boorowa Council (now at 3.25-3.75km and 8-8.9km West of Lachlan $461,000 Hilltops Council) Valley Way Boorowa Council (now MR 380 Cunningar Road Pavement $960,000 Hilltops Council) Rehabilitation and Widening Eyre/Comstock and Comstock//Patton Street Broken Hill City Council $700,000 Intersection Concrete Upgrade Clarence Valley Council Jacks Bridge Replacement $40,000 Clarence Valley Council Kinghorn Bridge Replacement $175,000 Clarence Valley Council Romiaka Channel Bridge Replacement $1,731,000 Cobar Shire Council Seal extension Wilga Downs Road (SR26) $800,000 Coffs Harbour City Council Rebuilding Taylors Bridge $180,000 Validation of maximum load limits for Coffs Coffs Harbour City Council $175,000 Harbour City Council Regional Road Bridges Coolamon Shire Council Ardlethan Grain Hub Connectivity Project $666,300 Cooma Monaro Shire Council (now Snowy Monaro Cooma Monaro Shire Bridge Assessment $184,000 Regional Council) Cooma Monaro Shire