Common Second Trimester Abortion Procedures a Second Trimester Abortion Occurs Between 16-20 Weeks' Gestation. in Iowa Aborti
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
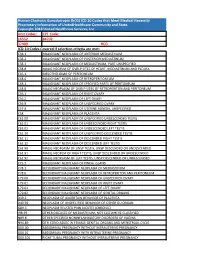
Human Chorionic Gonadotropin (Hcg) ICD 10 Codes That Meet Medical Necessity Proprietary Information of Unitedhealthcare Community and State
Human Chorionic Gonadotropin (hCG) ICD 10 Codes that Meet Medical Necessity Proprietary Information of UnitedHealthcare Community and State. Copyright 2018 United Healthcare Services, Inc Unit Codes: CPT Code: 16552 84702 37409 HCG ICD-10 Codes Covered if selection criteria are met: C38.1 MALIGNANT NEOPLASM OF ANTERIOR MEDIASTINUM C38.2 MALIGNANT NEOPLASM OF POSTERIOR MEDIASTINUM C38.3 MALIGNANT NEOPLASM OF MEDIASTINUM, PART UNSPECIFIED C38.8 MALIG NEOPLM OF OVRLP SITES OF HEART, MEDIASTINUM AND PLEURA C45.1 MESOTHELIOMA OF PERITONEUM C48.0 MALIGNANT NEOPLASM OF RETROPERITONEUM C48.1 MALIGNANT NEOPLASM OF SPECIFIED PARTS OF PERITONEUM C48.8 MALIG NEOPLASM OF OVRLP SITES OF RETROPERITON AND PERITONEUM C56.1 MALIGNANT NEOPLASM OF RIGHT OVARY C56.2 MALIGNANT NEOPLASM OF LEFT OVARY C56.9 MALIGNANT NEOPLASM OF UNSPECIFIED OVARY C57.4 MALIGNANT NEOPLASM OF UTERINE ADNEXA, UNSPECIFIED C58 MALIGNANT NEOPLASM OF PLACENTA C62.00 MALIGNANT NEOPLASM OF UNSPECIFIED UNDESCENDED TESTIS C62.01 MALIGNANT NEOPLASM OF UNDESCENDED RIGHT TESTIS C62.02 MALIGNANT NEOPLASM OF UNDESCENDED LEFT TESTIS C62.10 MALIGNANT NEOPLASM OF UNSPECIFIED DESCENDED TESTIS C62.11 MALIGNANT NEOPLASM OF DESCENDED RIGHT TESTIS C62.12 MALIGNANT NEOPLASM OF DESCENDED LEFT TESTIS C62.90 MALIG NEOPLASM OF UNSP TESTIS, UNSP DESCENDED OR UNDESCENDED C62.91 MALIG NEOPLM OF RIGHT TESTIS, UNSP DESCENDED OR UNDESCENDED C62.92 MALIG NEOPLASM OF LEFT TESTIS, UNSP DESCENDED OR UNDESCENDED C75.3 MALIGNANT NEOPLASM OF PINEAL GLAND C78.1 SECONDARY MALIGNANT NEOPLASM OF MEDIASTINUM C78.6 SECONDARY -

HB 1429 Dismemberment Abortion SPONSOR(S): Grall and Others TIED BILLS: IDEN./SIM
HOUSE OF REPRESENTATIVES STAFF ANALYSIS BILL #: HB 1429 Dismemberment Abortion SPONSOR(S): Grall and others TIED BILLS: IDEN./SIM. BILLS: SB 1890 REFERENCE ACTION ANALYST STAFF DIRECTOR or BUDGET/POLICY CHIEF 1) Health Quality Subcommittee 9 Y, 6 N McElroy McElroy 2) Judiciary Committee 3) Health & Human Services Committee SUMMARY ANALYSIS Dilation and evacuation (D&E) abortions commonly involve the dismemberment of the fetus as part of the evacuation procedure. This dismemberment is performed on a living fetus unless the abortion provider has induced fetal demise prior to initiating the evacuation procedure. HB 1429 prohibits a physician from knowingly performing a dismemberment abortion. The bill defines a dismemberment abortion as: An abortion in which a person, with the purpose of causing the death of an fetus, dismembers the living fetus and extracts the fetus one piece at a time from the uterus through the use of clamps, grasping forceps, tongs, scissors, or a similar instrument that, through the convergence of two rigid levers, slices, crushes, or grasps, or performs any combination of those actions on, a piece of the fetus’ body to cut or rip the piece from the body. The bill provides an exception to this prohibition under certain circumstances if a dismemberment abortion is necessary to save the life of a mother and no other medical procedure would suffice for that purpose. Any person who knowingly performs or actively participates in a dismemberment abortion commits a third degree felony. The bill exempts a woman upon whom a dismemberment abortion has been performed from prosecution for a conspiracy to violate this provision. -

Mifepristone and Buccal Misoprostol Versus Mifepristone and Vaginal Misoprostol for Cervical Preparation in Second-Trimester Surgical Abortion
TITLE: A Randomized Double-blinded Comparison of 24-hour interval- Mifepristone and Buccal Misoprostol versus Mifepristone and Vaginal Misoprostol for Cervical Preparation in Second-Trimester Surgical Abortion PI: Frances Casey, MD, MPH NCT03134183 Unique Protocol ID: HM20005740 Document Approval Date: April 15, 2015 Document Type: Protocol and SAP A Randomized Double-blinded Comparison of 24-hour interval-Mifepristone and Buccal Misoprostol versus Mifepristone and Vaginal Misoprostol for Cervical Preparation in Second-Trimester Surgical Abortion Principal Investigator: Frances Casey, MD, MPH, Virginia Commonwealth University Medical Center Co-Investigators: Randi Falls, MD, Virginia League of Planned Parenthood 1. Abstract Patient preference for medications in place of osmotic dilators as cervical preparation is well known. Twenty-four to 48 hours following mifepristone, vaginal and buccal misoprostol have demonstrated equal efficacy in second-trimester medical abortion but have not been compared as cervical preparation for second-trimester surgical abortion. This study will randomize participants undergoing a second-trimester surgical abortion between 16 0/7-20 6/7 weeks gestation to 200mg mifepristone followed 20-24 hours later with 400mcg vaginal misoprostol and buccal placebo versus 400mcg buccal misoprostol and vaginal placebo 1-2 hours prior to the procedure. Primary outcome is intraoperative procedure time as measured by time of first instrument in the uterus (dilator if further dilation is required or forceps if no further dilation required) to last instrument out of the uterus. The study uses a superiority design and is powered to detect a 4-minute difference in procedure time from a baseline of 10±5 minutes with 90% power and two-tailed alpha of 0.05 requiring 33 participants in each arm. -

Dilation and Evacuation (D & E)
FACT SHEET FOR PATIENTS AND FAMILIES Dilation and Evacuation (D & E) What is D & E ? Dilation (dy-LAY-shun] and evacuation [ee-vak-you-AY-shun] (D & E) is a procedure to open (dilate) the cervix and surgically clear the contents of the uterus (evacuation). It is typically done before 15 weeks of pregnancy or after a miscarriage. Because it signals the end of a pregnancy, the choice whether to have a D & E can be difficult. D& E is a common and safe procedure that usually takes about 20 minutes. What happens before D & E? You’ll have an appointment with your healthcare provider before your D & E. At this visit: • You will review the procedure and have a chance to ask questions. Bring a list of all prescriptions, over- the-counter medicines (such as allergy pills or cough Use this handout as a guide when talking with your healthcare provider. Be sure to ask any questions syrup), patches, vitamins, and herbs that you take. you may have so that you understand what will You may need to stop taking some of these a few days happen before, during, and after your D & E. before your procedure. • Your healthcare provider will prepare your cervix for the D & E. Common ways to open the cervix include If you’re having a D &E in a hospital the use of: Follow all instructions from your healthcare provider – Laminaria [lam-uh-NAIR-ee-uh] or Dilapan [DIL-uh-pan] about eating and drinking on the day before your dilators. These are thin sticks that are placed in procedure. -

Histomorphological Study of Chorionic Villi in Products of Conception Following First Trimester Abortions
November, 2018/ Vol 4/ Issue 7 Print ISSN: 2456-9887, Online ISSN: 2456-1487 Original Research Article Histomorphological study of chorionic villi in products of conception following first trimester abortions Shilpa MD1, Supreetha MS2, Varshashree3 1Dr. Shilpa, MD, Assistant Professor, 2Dr. Supreetha, MS, Assistant Professor, 3Dr. Varshashree, Post graduate, all authors are affiliated with Department of Pathology, Sri Devaraj Urs Medical College, Tamaka, Kolar, Karnataka, India. Corresponding Author: Dr. Shilpa, MD, Assistant Professor, Department of Pathology, Sri Devaraj Urs Medical College, Tamaka, Kolar, Karnataka, India. Email id: [email protected] ………………………………………………………………………………………………………………………………... Abstract Background: The common problem which occurs in first trimester of pregnancy is miscarriage. Retained products of conception are commonly received specimen for histopathological examination. Apart from confirmation of pregnancy, a careful examination can provide some additional information about the cause or the conditions associated with abortion. Aim: 1. To study various histopathological changes occurring in chorionic villi in first trimester spontaneous abortions and to know the pathogenesis of abortions. Materials and methods: This was a cross sectional retrospective study carried out for over a period of 3 years from January 2015 to January 2018. A total of 235biopsies were obtained from patient with the diagnosis of the first trimester spontaneous abortions were included in this study. Results: In our study most common age group of the abortion was between 21-30 years (63%). Incomplete abortion was the commonest type of abortion (47.7%). Many dysmorphic features were observed in this study like hydropic change (67%), stromal fibrosis (62%), villi with reduced blood vessels (52.7%) and perivillous fibrin deposition. -

Medical Abortion Reference Guide INDUCED ABORTION and POSTABORTION CARE at OR AFTER 13 WEEKS GESTATION (‘SECOND TRIMESTER’) © 2017, 2018 Ipas
Medical Abortion Reference Guide INDUCED ABORTION AND POSTABORTION CARE AT OR AFTER 13 WEEKS GESTATION (‘SECOND TRIMESTER’) © 2017, 2018 Ipas ISBN: 1-933095-97-0 Citation: Edelman, A. & Mark, A. (2018). Medical Abortion Reference Guide: Induced abortion and postabortion care at or after 13 weeks gestation (‘second trimester’). Chapel Hill, NC: Ipas. Ipas works globally so that women and girls have improved sexual and reproductive health and rights through enhanced access to and use of safe abortion and contraceptive care. We believe in a world where every woman and girl has the right and ability to determine her own sexuality and reproductive health. Ipas is a registered 501(c)(3) nonprofit organization. All contributions to Ipas are tax deductible to the full extent allowed by law. For more information or to donate to Ipas: Ipas P.O. Box 9990 Chapel Hill, NC 27515 USA 1-919-967-7052 [email protected] www.ipas.org Cover photo: © Ipas The photographs used in this publication are for illustrative purposes only; they do not imply any particular attitudes, behaviors, or actions on the part of any person who appears in the photographs. Printed on recycled paper. Medical Abortion Reference Guide INDUCED ABORTION AND POSTABORTION CARE AT OR AFTER 13 WEEKS GESTATION (‘SECOND TRIMESTER’) Alison Edelman Senior Clinical Consultant, Ipas Professor, OB/GYN Oregon Health & Science University Alice Mark Associate Medical Director National Abortion Federation About Ipas Ipas works globally so that women and girls have improved sexual and reproductive health and rights through enhanced access to and use of safe abortion and contraceptive care. -

Miscarriage Or Early Pregnancy Loss- Diagnosis and Management (Version 5)
Miscarriage or early pregnancy loss- diagnosis and management (Version 5) Guideline Readership This guideline applies to all women diagnosed with miscarriage in early pregnancy (up to 13 completed weeks) within the Heart of England Foundation Trust and to attending clinicians, sonographers and nursing staff on Gynaecology ward and early pregnancy unit. All care is tailored to individual patient needs, with an in-depth discussion of the intended risks and benefits for any intervention offered to woman with early pregnancy loss. Guideline Objectives The objective of this guideline is to enable all clinicians to recognise the different types of miscarriages and to follow a recognised management pathway so that all women with actual or suspected miscarriage receive, an appropriate and individualised care. Other Guidance Ectopic pregnancy and miscarriage: diagnosis and initial management. NICE guidance Dec 2012 Ratified Date: Insert Date Launch Date: 16 March 2018 Review Date: 16 March 2021 Guideline Author: Dr Rajmohan, Dr Cheema Contents & page numbers: 1. Flowcharts Flowchart 1 – Management of complete miscarriage p3 Flowchart 2 – Management of incomplete miscarriage p4 Flowchart 3 – Management of Missed miscarriage p5 Flowchart 4 - Management of Early fetal demise p6 Flowchart 5 – Medical management of miscarriage p7 Flowchart 6 - Surgical management (SMM) pathway p8 2. Executive summary and Overview p9 3. Body of guideline Types of miscarriage p9 Threatened miscarriage p9 Complete miscarriage p9 Incomplete miscarriage p9 Missed miscarriage -

Transvaginal Administration of Intraamniotic Digoxin Prior to Dilation and Evacuation
UC Davis UC Davis Previously Published Works Title Transvaginal administration of intraamniotic digoxin prior to dilation and evacuation Permalink https://escholarship.org/uc/item/6vw7r4gd Journal Contraception, 87(1) Author Creinin, Mitchell David Publication Date 2013 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Contraception 87 (2013) 76–80 Original research article Transvaginal administration of intraamniotic digoxin prior to dilation and evacuation ⁎ Aileen M. Gariepya, , Beatrice A. Chenb, Heather L. Hohmannb, Sharon L. Achillesb, Jennefer A. Russob, Mitchell D. Creininc aDepartment of Obstetrics, Gynecology, and Reproductive Sciences, Yale University School of Medicine, New Haven, CT 06520, USA bDepartment of Obstetrics, Gynecology, and Reproductive Sciences, University of Pittsburgh School of Medicine, Pittsburgh, PA and the Center for Family Planning Research, Magee-Womens Research Institute, Pittsburgh, PA 15213, USA cDepartment of Obstetrics and Gynecology, University of California, Davis, Sacramento, CA 95817, USA Received 13 March 2012; revised 13 July 2012; accepted 27 July 2012 Abstract Background: Transabdominal injection of digoxin into the amniotic fluid or fetus to induce fetal demise before dilation and evacuation (D&E) abortion has become common practice since the passage of the Partial-Birth Abortion Ban Act in 2007. Study Design: We performed a prospective study to assess the feasibility of transvaginal administration of intraamniotic digoxin the day before D&E. All women between 18 0/7 and 23 5/7 weeks of gestation seeking termination from December 2009 to May 2011 were approached for study participation. Women who declined participation were asked to identify their primary rationale. For women declining study participation, transection of the umbilical cord during D&E was performed to meet the requirements of the ban. -

If You Are Pregnant: INFORMATION on FETAL DEVELOPMENT, ABORTION and ALTERNATIVES August 2019
If You Are Pregnant: INFORMATION ON FETAL DEVELOPMENT, ABORTION AND ALTERNATIVES August 2019 IF YOU ARE PREGNANT: INFORMATION ON FETAL DEVELOPMENT, ABORTION AND ALTERNATIVES If You Are Pregnant: Information on Fetal Development, Abortion and Alternatives Resources used by the Minnesota Department of Health for this publication are Human Embryology and Developmental Biology, Fifth Edition, 2014; Larsen’s Human Embryology, Fifth Edition, 2014; The Developing Human, 10th Edition, 2016; and In the Womb, 2006. The photographs in this booklet are credited to Lennart Nilsson/TT Images and are used by permission; except for week 38 copyright Minnesota Department of Health. The illustrations found throughout this booklet were created by Peg Gerrity, Houston, Texas. Copyright: http://www.peggerrity.com. Minnesota Department of Health Division of Child and Family Health PO Box 64882 St. Paul, MN 55164-0882 651-201-3580 Women's Right to Know (https://www.health.state.mn.us/people/wrtk/index.html) Upon request, this material will be made available in an alternative format such as large print, Braille or audio recording. Printed on recycled paper. 2 IF YOU ARE PREGNANT: INFORMATION ON FETAL DEVELOPMENT, ABORTION AND ALTERNATIVES Contents If You Are Pregnant: INFORMATION ON FETAL DEVELOPMENT, ABORTION AND ALTERNATIVES............................................................................................................................. 1 Introduction ............................................................................................................................... -

Ectopic Pregnancy Management: Tubal and Interstitial SIGNS / SYMPTOMS DIAGNOSIS
8/29/19njm Ectopic Pregnancy Management: Tubal and interstitial SIGNS / SYMPTOMS Pain and vaginal bleeding are the hallmark symptoms of ectopic pregnancy. Pain is almost universal; it is generally lower abdominal and unilateral. Bleeding is also very common following a short period of amenorrhea. Physical exam may reveal a tender adnexal mass, often mentioned in texts, but noted clinically only 20 percent of the time. Furthermore, it may easily be confused with a tender corpus luteum of a normal intrauterine pregnancy. Finally signs and symptoms of hemoperitoneum and shock can occur, including a distended, silent, “doughy” abdomen, shoulder pain, bulging cul de sac into the posterior fornix of the vagina, and hypotension. DIAGNOSIS Initially, serum hCG rises, but then usually plateaus or falls. Transvaginal ultrasound scanning is a key diagnostic tool and can rapidly make these diagnoses: 1. Ectopic is ruled out by the presence of an intrauterine pregnancy with the exception of rare heterotopic pregnancy 2. Ectopic is proven when a gestational sac and an embryo with a heartbeat is seen outside of the uterus 3. Ectopic is highly likely if ANY adnexal mass distinct from the corpus luteum or a significant amount of free pelvic fluid is seen. When ultrasound is not definitive, correlation of serum hCG levels is important. If the hCG is above the “discriminatory zone” of 3000 mIU/ml IRP, a gestational sac should be visible on transvaginal ultrasound. The discriminatory zone varies by ultrasound machine and sonographer. If an intrauterine gestational sac is not visible by the time the hCG is at, or above, this threshold, the pregnancy has a high likelihood of being ectopic. -

Whole Woman's Health V. Paxton
Case: 17-51060 Document: 00515984856 Page: 1 Date Filed: 08/18/2021 United States Court of Appeals United States Court of Appeals for the Fifth Circuit Fifth Circuit FILED August 18, 2021 No. 17-51060 Lyle W. Cayce Clerk Whole Woman’s Health, on behalf of itself, its staff, physicians and patients; Planned Parenthood Center for Choice, on behalf of itself, its staff, physicians, and patients; Planned Parenthood of Greater Texas Surgical Health Services, on behalf of itself, its staff, physicians, and patients; Planned Parenthood South Texas Surgical Center, on behalf of itself, its staff, physicians, and patients; Alamo City Surgery Center, P.L.L.C., on behalf of itself, its staff, physicians, and patients, doing business as Alamo Women’s Reproductive Services; Southwestern Women’s Surgery Center, on behalf of itself, its staff, physicians, and patients; Curtis Boyd, M.D., on his own behalf and on behalf of his patients; Jane Doe, M.D., M.A.S., on her own behalf and on behalf of her patients; Bhavik Kumar, M.D., M.P.H., on his own behalf and on behalf of his patients; Alan Braid, M.D., on his own behalf and on behalf of his patients; Robin Wallace, M.D., M.A.S., on her own behalf and on behalf of her patients, Plaintiffs—Appellees, versus Ken Paxton, Attorney General of Texas, in his official capacity; Sharen Wilson, Criminal District Attorney for Tarrant County, in her official capacity; Barry Johnson, Criminal District Attorney for McLennan County, in his official capacity, Defendants—Appellants. Case: 17-51060 Document: 00515984856 Page: 2 Date Filed: 08/18/2021 Appeal from the United States District Court for the Western District of Texas USDC No. -

Abortion at Or Over 20 Weeks' Gestation
Abortion At or Over 20 Weeks’ Gestation: Frequently Asked Questions Matthew B. Barry, Coordinator Section Research Manager April 30, 2018 Congressional Research Service 7-5700 www.crs.gov R45161 Abortion At or Over 20 Weeks’ Gestation: Frequently Asked Questions Summary Legislation at the federal and state levels seeking to limit or ban abortions in midpregnancy has focused attention on the procedure and the relatively small number of women who choose to undergo such an abortion. According to the Guttmacher Institute, about 926,200 abortions were performed in 2014; 1.3% of abortions were performed at or over 21 weeks’ gestation in 2013. A 2018 National Academies of Sciences, Engineering, and Medicine study found that most women who have abortions are unmarried (86%), are poor or low-income (75%), are under age 30 (72%), and are women of color (61%). Stages of Pregnancy and Abortion Procedures A typical, full-term pregnancy spans 40 weeks, separated into trimesters: first trimester (week 1 through week 13), second trimester (week 14 through week 27), and third trimester (week 28 through birth). Abortion in the second trimester can be performed either by using a surgical procedure or by using drugs to induce labor. According to the Centers for Disease Control and Prevention (CDC), in 2014 a surgical method was used for 98.8% of U.S. abortions at 14-15 weeks’ gestation, 98.4% at 16-17 weeks, 96.6% at 18-20 weeks, and 90.2% at 21 weeks or later. Proposed Legislation Related to Abortion Legislation in the 115th Congress, the Pain-Capable Unborn Child Protection Act (H.R.