Appendix A: Dosing Regimens Modelled
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Old and New Challenges in Uveitis Associated with Behçet's Disease
Journal of Clinical Medicine Review Old and New Challenges in Uveitis Associated with Behçet’s Disease Julie Gueudry 1,* , Mathilde Leclercq 2, David Saadoun 3,4,5 and Bahram Bodaghi 6 1 Department of Ophthalmology, Hôpital Charles Nicolle, F-76000 Rouen, France 2 Department of Internal Medicine, Hôpital Charles Nicolle, F-76000 Rouen, France; [email protected] 3 Department of Internal Medicine and Clinical Immunology, AP-HP, Centre National de Références Maladies Autoimmunes et Systémiques Rares et Maladies Autoinflammatoires Rares, Groupe Hospitalier Pitié-Salpêtrière, F-75013 Paris, France; [email protected] 4 Sorbonne Universités, UPMC Univ Paris 06, INSERM, UMR S 959, Immunology-Immunopathology-Immunotherapy (I3), F-75005 Paris, France 5 Biotherapy (CIC-BTi), Hôpital Pitié-Salpêtrière, AP-HP, F-75651 Paris, France 6 Department of Ophthalmology, IHU FOReSIGHT, Sorbonne-AP-HP, Groupe Hospitalier Pitié-Salpêtrière, F-75013 Paris, France; [email protected] * Correspondence: [email protected]; Tel.: +33-2-32-88-80-57 Abstract: Behçet’s disease (BD) is a systemic vasculitis disease of unknown origin occurring in young people, which can be venous, arterial or both, classically occlusive. Ocular involvement is particularly frequent and severe; vascular occlusion secondary to retinal vasculitis may lead to rapid and severe loss of vision. Biologics have transformed the management of intraocular inflammation. However, the diagnosis of BD is still a major challenge. In the absence of a reliable biological marker, diagnosis is based on clinical diagnostic criteria and may be delayed after the appearance of the onset sign. However, therapeutic management of BD needs to be introduced early in order to control inflammation, to preserve visual function and to limit irreversible structural damage. -

Pharmacologic Considerations in the Disposition of Antibodies and Antibody-Drug Conjugates in Preclinical Models and in Patients
antibodies Review Pharmacologic Considerations in the Disposition of Antibodies and Antibody-Drug Conjugates in Preclinical Models and in Patients Andrew T. Lucas 1,2,3,*, Ryan Robinson 3, Allison N. Schorzman 2, Joseph A. Piscitelli 1, Juan F. Razo 1 and William C. Zamboni 1,2,3 1 University of North Carolina (UNC), Eshelman School of Pharmacy, Chapel Hill, NC 27599, USA; [email protected] (J.A.P.); [email protected] (J.F.R.); [email protected] (W.C.Z.) 2 Division of Pharmacotherapy and Experimental Therapeutics, UNC Eshelman School of Pharmacy, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] 3 Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-919-966-5242; Fax: +1-919-966-5863 Received: 30 November 2018; Accepted: 22 December 2018; Published: 1 January 2019 Abstract: The rapid advancement in the development of therapeutic proteins, including monoclonal antibodies (mAbs) and antibody-drug conjugates (ADCs), has created a novel mechanism to selectively deliver highly potent cytotoxic agents in the treatment of cancer. These agents provide numerous benefits compared to traditional small molecule drugs, though their clinical use still requires optimization. The pharmacology of mAbs/ADCs is complex and because ADCs are comprised of multiple components, individual agent characteristics and patient variables can affect their disposition. To further improve the clinical use and rational development of these agents, it is imperative to comprehend the complex mechanisms employed by antibody-based agents in traversing numerous biological barriers and how agent/patient factors affect tumor delivery, toxicities, efficacy, and ultimately, biodistribution. -

Interleukins in Therapeutics
67 ISSN: 2347 - 7881 Review Article Interleukins in Therapeutics Anjan Khadka Department of Pharmacology, AFMC, Pune, India [email protected] ABSTRACT Interleukins are a subset of a larger group of cellular messenger molecules called cytokines, which are modulators of cellular behaviour. On the basis of their respective cytokine profiles, responses to chemokines, and interactions with other cells, these T-cell subsets can promote different types of inflammatory responses. During the development of allergic disease, effector TH2 cells produce IL-4, IL- 5, IL-9, and IL-32. IL-25, IL- 31, and IL-33 contributes to TH2 responses and inflammation. These cytokines have roles in production of allergen-specific IgE, eosinophilia, and mucus. ILs have role in therapeutics as well as diagnosis and prognosis as biomarker in various conditions. Therapeutic targeting of the IL considered to be rational treatment strategy and promising biologic therapy. Keywords: Interleukins, cytokines, Interleukin Inhibitors, Advances INTRODUCTION meaning ‘hormones’. It was Stanley Cohen in Interleukins are group of cytokines that were 1974 who for the first time introduced the term first seen to be expressed by leucocytes and ‘‘cytokine’’. It includes lymphokines, they interact between cells of the immune monokines, interleukins, and colony stimulating systems. It is termed by Dr. Vern Paetkau factors (CSFs), interferons (IFNs), tumor (University of Victoria) in1979.Interleukins (IL) necrosis factor (TNF) and chemokines. The are able to promote cell growth, differentiation, majority of interleukins are synthesized by and functional activation. The question of how helper CD4 T lymphocytes as well as through diverse cell types communicate with each monocytes, macrophages, and endothelial cells. -

Review Anti-Cytokine Biologic Treatment Beyond Anti-TNF in Behçet's Disease
Review Anti-cytokine biologic treatment beyond anti-TNF in Behçet’s disease A. Arida, P.P. Sfikakis First Department of Propedeutic Internal ABSTRACT and thrombotic complications (1-3). Medicine Laikon Hospital, Athens, Unmet therapeutic needs in Behçet’s Treatment varies according to type and University Medical School, Greece. disease have drawn recent attention to severity of disease manifestations. Cor- Aikaterini Arida, MD biological agents targeting cytokines ticosteroids, interferon-alpha and con- Petros P. Sfikakis, MD other than TNF. The anti-IL-17 anti- ventional immunosuppressive drugs, Please address correspondence to: body secukinumab and the anti-IL-2 such as azathioprine, cyclosporine-A, Petros P. Sfikakis, MD, receptor antibody daclizumab were not cyclophosphamide and methotrexate, First Department of Propedeutic superior to placebo for ocular Behçet’s and Internal Medicine, are used either alone or in combination Laikon Hospital, in randomised controlled trials, com- for vital organ involvement. During the Athens University Medical School, prising 118 and 17 patients, respec- last decade there has been increased use Ag Thoma, 17, tively. The anti-IL-1 agents anakinra of anti-TNF monoclonal antibodies in GR-11527 Athens, Greece. and canakinumab and the anti-IL-6 patients with BD who were refractory E-mail: [email protected] agent tocilizumab were given to iso- to conventional treatment or developed Received on June 7, 2014; accepted in lated refractory disease patients, who life-threatening complications (4, 5). revised form on September 17, 2014. were either anti-TNF naïve (n=9) or Anti-TNF treatment has been shown to Clin Exp Rheumatol 2014; 32 (Suppl. 84): experienced (n=18). -

Challenges and Approaches for the Development of Safer Immunomodulatory Biologics
REVIEWS Challenges and approaches for the development of safer immunomodulatory biologics Jean G. Sathish1*, Swaminathan Sethu1*, Marie-Christine Bielsky2, Lolke de Haan3, Neil S. French1, Karthik Govindappa1, James Green4, Christopher E. M. Griffiths5, Stephen Holgate6, David Jones2, Ian Kimber7, Jonathan Moggs8, Dean J. Naisbitt1, Munir Pirmohamed1, Gabriele Reichmann9, Jennifer Sims10, Meena Subramanyam11, Marque D. Todd12, Jan Willem Van Der Laan13, Richard J. Weaver14 and B. Kevin Park1 Abstract | Immunomodulatory biologics, which render their therapeutic effects by modulating or harnessing immune responses, have proven their therapeutic utility in several complex conditions including cancer and autoimmune diseases. However, unwanted adverse reactions — including serious infections, malignancy, cytokine release syndrome, anaphylaxis and hypersensitivity as well as immunogenicity — pose a challenge to the development of new (and safer) immunomodulatory biologics. In this article, we assess the safety issues associated with immunomodulatory biologics and discuss the current approaches for predicting and mitigating adverse reactions associated with their use. We also outline how these approaches can inform the development of safer immunomodulatory biologics. Immunomodulatory Biologics currently represent more than 30% of licensed The high specificity of the interactions of immu- biologics pharmaceutical products and have expanded the thera- nomodulatory biologics with their relevant immune Biotechnology-derived peutic options available -

Biological Therapies for Atopic Dermatitis: an Update (Review)
EXPERIMENTAL AND THERAPEUTIC MEDICINE 17: 1061-1067, 2019 Biological therapies for atopic dermatitis: An update (Review) DIANA DELEANU1-3 and IRENA NEDELEA1,2 1Allergology and Immunology Discipline, ‘Iuliu Hatieganu’ University of Medicine and Pharmacy, 400058 Cluj-Napoca; Departments of 2Allergy and 3Internal Medicine, ‘Professor Doctor Octavian Fodor’ Regional Institute of Gastroenterology and Hepatology, 400162 Cluj-Napoca, Romania Received July 6, 2018; Accepted August 22, 2018 DOI: 10.3892/etm.2018.6989 Abstract. Severe atopic dermatitis, which affects both adults in low-income countries (3). Furthermore, the past decades and children, is a debilitating disorder with a significant decline brought a 2-3-fold increase in prevalence in industrialized of patients' quality of life. Although aetiopathogenic factors countries (3). Generally AD onset is in early childhood, as are currently a topic of study and interpretation, the main one of the first steps of the ‘atopic march’, which describes the features of atopic eczema are skin barrier disturbance and natural history of atopic manifestations, and it is character- immune dysregulation. Severe refractory disease that fails to ized by xerotic skin and acute flare-ups of intensely pruritic improve with conventional therapy may benefit from biologic eczematous lesions (4). Recent studies recognize a predilection therapy. Progress in understanding immunopathology of atopic of AD for persistence in adulthood, with a lifetime prevalence dermatitis have allowed identification of therapeutic molecular accounting for 34.1% (5). Early onset, allergic rhinitis and targets in the field of biological therapy. We reviewed the hand eczema in childhood are high-risk factors for persistent different biological treatments with a focus on novel targeted AD (5). -

Ilaris Canakinumab for Systemic Juvenile Idiopathic Arthritis SJIA
Subject: Ilaris (canakinumab) for Systemic Juvenile Original Effective Date: 4/24/2015 Idiopathic Arthritis (SJIA) Policy Number: MCP-246 Revision Date(s): Review Date(s): 12/15/2016; 6/22/2017 DISCLAIMER This Medical Policy is intended to facilitate the Utilization Management process. It expresses Molina's determination as to whether certain services or supplies are medically necessary, experimental, investigational, or cosmetic for purposes of determining appropriateness of payment. The conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Molina) for a particular member. The member's benefit plan determines coverage. Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Members and their providers will need to consult the member's benefit plan to determine if there are any exclusion(s) or other benefit limitations applicable to this service or supply. If there is a discrepancy between this policy and a member's plan of benefits, the benefits plan will govern. In addition, coverage may be mandated by applicable legal requirements of a State, the Federal government or CMS for Medicare and Medicaid members. CMS's Coverage Database can be found on the CMS website. The coverage directive(s) and criteria from an existing National Coverage Determination (NCD) or Local Coverage Determination (LCD) will supersede the contents of this Molina medical coverage policy (MCP) document and provide the directive for all Medicare members. SUMMARY This policy addresses the coverage of Ilaris (canakinumab) for the treatment of Systemic Juvenile Idiopathic Arthritis (SJIA) when appropriate criteria are met. -

Anticorps FR-EN 110X90.Indd
MONOCLONAL ANTIBODIES and Fc fusion proteins for therapeutic use DISTRIBUTION OF INTERNATIONAL NONPROPRIETARY NAMES BY INDICATION SOLID TUMORS RHUMATOLOGY PNEUMOLOGY Lung cancer bevacizumab Rheumatoid arthritis etanercept Allergic asthma omalizumab nivolumab infliximab Severe eosinophilic asthma mepolizumab necitumumab adalimumab reslizumab atezolizumab rituximab Colorectal cancer bevacizumab abatacept TRANSPLANTATION cetuximab tocilizumab Transplant rejection basiliximab panitumumab certolizumab pegol belatacept aflibercept golimumab Graft versus host disease inolimomab Bladder cancer atezolizumab Psoriatic arthritis etanercept Breast cancer trastuzumab adalimumab OPHTALMOLOGY bevacizumab infliximab Age related macular ranibizumab pertuzumab golimumab degeneration aflibercept trastuzumab entansine ustekinumab bevacizumab Gastric cancer trastuzumab certolizumab pegol Macular edema ranibizumab ramucirumab secukinumab aflibercept Head and neck cancer cetuximab Ankylosing spondylitis infliximab Myopic choroidal ranibizumab Ovarian cancer bevacizumab etanercept neovascularization aflibercept Fallopian tube cancer bevacizumab adalimumab Cervical cancer bevacizumab golimumab HAEMOSTASIS AND THROMBOSIS Kidney cancer bevacizumab certolizumab pegol nivolumab secukinumab Haemophilia A efmoroctocog α Melanoma ipilimumab Juvenile arthritis etanercept Haemophilia B eftrenonacog α nivolumab adalimumab Reversal of dabigatran idarucizumab Idiopathic thrombocytopenic pembrolizumab abatacept romiplostim Neuroblastoma dinutuximab tocilizumab purpura Malignant -
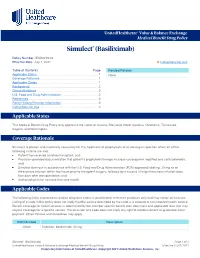
Simulect® (Basiliximab)
UnitedHealthcare® Value & Balance Exchange Medical Benefit Drug Policy Simulect® (Basiliximab) Policy Number: IEXD0219.02 Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Related Policies Applicable States ........................................................................... 1 None Coverage Rationale ....................................................................... 1 Applicable Codes .......................................................................... 1 Background.................................................................................... 2 Clinical Evidence ........................................................................... 2 U.S. Food and Drug Administration ............................................. 2 References ..................................................................................... 2 Policy History/Revision Information ............................................. 2 Instructions for Use ....................................................................... 3 Applicable States This Medical Benefit Drug Policy only applies to the states of Arizona, Maryland, North Carolina, Oklahoma, Tennessee, Virginia, and Washington. Coverage Rationale Simulect is proven and medically necessary for the treatment of prophylaxis of acute organ rejection when all of the following criteria are met: Patient has received a kidney transplant; and Physician provided documentation that patient’s prophylaxis therapy includes cyclosporine modified and corticosteroids; and Simulect -

Inflammatory Conditions – Kevzara™ (Sarilumab for Subcutaneous Injection)
Cigna National Formulary Coverage Policy Prior Authorization Inflammatory Conditions – Kevzara® (sarilumab for subcutaneous injection) Table of Contents Product Identifier(s) National Formulary Medical Necessity ................ 1 59231 Conditions Not Covered....................................... 2 Background .......................................................... 2 References .......................................................... 3 Revision History ................................................... 3 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may contain a specific exclusion related to a topic addressed in a Coverage Policy. In the event of a conflict, a customer’s benefit plan document always supersedes the information in the Coverage Policies. In the absence of a controlling federal or state coverage mandate, benefits are ultimately determined by the terms of the applicable benefit plan document. Coverage determinations in each specific instance require consideration of 1) the terms of the applicable benefit plan document in effect on the date of service; 2) any applicable laws/regulations; 3) any relevant collateral source materials including Coverage Policies and; 4) the specific facts of the particular situation. -

761037Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 761037Orig1s000 OTHER REVIEW(S) --------------------------------------------------------------------------------------------------------- This is a representation of an electronic record that was signed electronically and this page is the manifestation of the electronic signature. --------------------------------------------------------------------------------------------------------- /s/ ---------------------------------------------------- CHRISTINE H FORD 05/19/2017 Reference ID: 4100987 Continuation of Question 4 Additional data or analysis required for a previously submitted or expected study/clinical trial (provide explanation) Meta-analysis or pooled analysis of previous studies/clinical trials Immunogenicity as a marker of safety Other (provide explanation) Agreed upon: Quality study without a safety endpoint (e.g., manufacturing, stability) Pharmacoepidemiologic study not related to safe drug use (e.g., natural history of disease, background rates of adverse events) Clinical trials primarily designed to further define efficacy (e.g., in another condition, different disease severity, or subgroup) that are NOT required under Subpart H/E Dose-response study or clinical trial performed for effectiveness Nonclinical study, not safety-related (specify) Other 5. Is the PMR/PMC clear, feasible, and appropriate? Does the study/clinical trial meet criteria for PMRs or PMCs? Are the objectives clear from the description of the PMR/PMC? Has the applicant adequately justified the choice -

September 2017 ~ Resource #330909
−This Clinical Resource gives subscribers additional insight related to the Recommendations published in− September 2017 ~ Resource #330909 Medications Stored in the Refrigerator (Information below comes from current U.S. and Canadian product labeling and is current as of date of publication) Proper medication storage is important to ensure medication shelf life until the manufacturer expiration date and to reduce waste. Many meds are recommended to be stored at controlled-room temperature. However, several meds require storage in the refrigerator or freezer to ensure stability. See our toolbox, Medication Storage: Maintaining the Cold Chain, for helpful storage tips and other resources. Though most meds requiring storage at temperatures colder than room temperature should be stored in the refrigerator, expect to see a few meds require storage in the freezer. Some examples of medications requiring frozen storage conditions include: anthrax immune globulin (Anthrasil [U.S. only]), carmustine wafer (Gliadel [U.S. only]), cholera (live) vaccine (Vaxchora), dinoprostone vaginal insert (Cervidil), dinoprostone vaginal suppository (Prostin E2 [U.S.]), varicella vaccine (Varivax [U.S.]; Varivax III [Canada] can be stored in the refrigerator or freezer), zoster vaccine (Zostavax [U.S.]; Zostavax II [Canada] can be stored in the refrigerator or freezer). Use the list below to help identify medications requiring refrigerator storage and become familiar with acceptable temperature excursions from recommended storage conditions. Abbreviations: RT = room temperature Abaloparatide (Tymlos [U.S.]) Aflibercept (Eylea) Amphotericin B (Abelcet, Fungizone) • Once open, may store at RT (68°F to 77°F • May store at RT (77°F [25°C]) for up to Anakinra (Kineret) [20°C to 25°C]) for up to 30 days.