Alberta Health Services Performance Review : Summary Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fairview Health Data and Summary
Alberta Health Primary Health Care - Community Profiles Community Profile: Fairview Health Data and Summary Primary Health Care Division February 2013 Alberta Health, Primary Health Care Division February 2013 Community Profile: Fairview Table of Contents Introduction .................................................................................................................................................. i Community Profile Summary .............................................................................................................. iii Zone Level Information .......................................................................................................................... 1 Map of Alberta Health Services North Zone ............................................................................................. 2 Population Health Indicators ..................................................................................................................... 3 Table 1.1 Zone versus Alberta Population Covered as at March 31, 2012 ........................................... 3 Table 1.2 Health Status Indicators for Zone versus Alberta Residents, 2010 and 2011 (BMI, Physical Activity, Smoking, Self-Perceived Mental Health) ............................................................................................... 3 Table 1.3 Zone versus Alberta Infant Mortality Rates (per 1,000 live births), Fiscal Years 2008/2009 to 2010/2011 ................................................................................... 4 Local -

Rocky Mountain House Health Data and Summary
Alberta Health Primary Health Care - Community Profiles Community Profile: Rocky Mountain House Health Data and Summary Primary Health Care Division February 2013 Alberta Health, Primary Health Care Division February 2013 Community Profile: Rocky Mountain House Table of Contents Introduction .................................................................................................................................................. i Community Profile Summary .............................................................................................................. iii Zone Level Information .......................................................................................................................... 1 Map of Alberta Health Services Central Zone .......................................................................................... 2 Population Health Indicators ..................................................................................................................... 3 Table 1.1 Zone versus Alberta Population Covered as at March 31, 2012 ........................................... 3 Table 1.2 Health Status Indicators for Zone versus Alberta Residents, 2010 and 2011 (BMI, Physical Activity, Smoking, Self-Perceived Mental Health) ............................................................................................... 3 Table 1.3 Zone versus Alberta Infant Mortality Rates (per 1,000 live births) Fiscal Years 2008/2009 to 2010/2011 .................................................................................. -

Hospital Services in Alberta – General Hospital (Active Treatment /Acute Care) JULY 2018
Alberta Health, Health Facilities Planning Branch For General Reference Purposes Only Hospital Services In Alberta – General Hospital (Active Treatment /Acute Care) JULY 2018 Hospital Services in Alberta – JULY 2018 General Hospital (Active Treatment / Acute Care) Auxiliary Hospital (Chronic/ Long Term Care) Alberta Health Services (AHS) New Zones: Zone 1 – South [ ] Zone 2 – Calgary [ ] Zone 3 – Central [ ] Zone 4 – Edmonton [ ] Zone 5 – North [ ] Legend: (1) Hospital Legal Name: Name appearing on M.O. #10/2011, as amended by M.O.s #10/2013, #42/2013, #33/2014, #31/2015 referencing the Consolidated Schedule of Approved Hospitals (CSAH). (2) Operator Type: Regional Health Authority (AHS) or Voluntary (VOL) (3) Operator Identity: Corporate organization name of the “hospital service operator”. (4) Sub-Acute Care (SAC): Some hospitals (highlighted) also operate a registered SAC service. Disclaimer: This list is compiled from registration information documented by the department as certified by Alberta Health Services (AHS). Facilities on the list may also provide health services or programs other than approved hospital services. This list is amended from time to time, as certified by Alberta Health Services, but may not be complete/accurate when it is read. Questions regarding specific facilities appearing on this list should be directed to Alberta Health Services. © 2018 Government of Alberta Page 1 of 24 Alberta Health, Health Facilities Planning Branch For General Reference Purposes Only Hospital Services In Alberta – General -
Fox Creek, Health Data and Summary, 4Th Edition
Alberta Health Primary, Community and Indigenous Health Community Profile: Fox Creek Health Data and Summary 4th Edition, December 2019 Alberta Health December 2019 Community Profile: Fox Creek Table of Contents Introduction .................................................................................................................................................. i Community Profile Summary .............................................................................................................. iii Zone Level Information ........................................................................................................................... 1 Map of Alberta Health Services North Zone .............................................................................................. 2 Population Health Indicators ...................................................................................................................... 3 Table 1.1 Zone versus Alberta Population Covered as at March 31, 2018 .............................................. 3 Table 1.2 Health Status Indicators for Zone versus Alberta Residents, 2013 and 2014 (Body Mass Index, Physical Activity, Smoking, Self-Perceived Mental Health)……………………………................3 Table 1.3 Zone versus Alberta Infant Mortality Rates (per 1,000 live births), Years 2016 – 2018…….. .. 4 Community Mental Health ........................................................................................................................... 5 Table 1.4 Zone versus Alberta Community Mental -

Yellowhead East Health Advisory Council Continues Recruitment for Members
David Thompson/ Yellowhead East Meeting Summary January 22, 2020 / 5:00 p.m. – 8:00 p.m. / Telehealth Introducing your Health Advisory Council members: In attendance David Thompson: Carole Tkach (Chair), Deryl Comeau (Vice Chair), Marie Cornelson, Gerald Johnston, Dawn Konelsky, Phyllis Loewen, Shelagh Slater Regrets: Geraldine Greschner, Melanie Hassett, Peggy Makofka, Selena Redel Yellowhead East: Cyndy Heslin (Chair), Sarah Hissett (Vice Chair), Glenys Reeves, Lesley Binning, Stephanie Munro, Taneen Rudyk Regrets: Deborah McMann, John Erkelenes Alberta Health Services: Sherie Allen, Maya Atallah, Leanne Grant, Debora Okrainetz, Janice Stewart, Marlene Young Community Input Two members of the public were in attendance and shared the following: Community members from Coronation expressed concern about response times of ambulances, as a result of being held up in emergency departments. The feeling is it would be more efficient to have hospital staff assigned to a patient when Emergency Medical Services (EMS) drops them off so ambulances are free to respond to calls. Lara Harries, consultant with Rural Health Professions Action Plan (RhPAP), shared information on the Rhapsody Awards for 2020, and the Building a Better Community Rural Workshop it is hosting. She shared that May 25-29, 2020 is Alberta Rural Health Week and is a great opportunity to host appreciation events/efforts in communities. She encourages attendees to sign up for the monthly and weekly newsletter to be kept up to date on events and news. AHS Presentation Central -
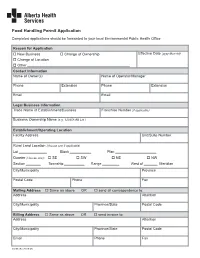
Food Handling Permit Application
Food Handling Permit Application Completed applications should be forwarded to your local Environmental Public Health Office Reason for Application o New Business o Change of Ownership Effective Date (yyyy-Mon-dd) o Change of Location o Other Contact Information Name of Owner(s) Name of Operator/Manager Phone Extension Phone Extension Email Email Legal Business Information Trade Name of Establishment/Business Franchise Number (if applicable) Business Ownership Name (e.g. 123456 AB Ltd.) Establishment/Operating Location Facility Address Unit/Suite Number Rural Land Location (choose one if applicable) Lot Block Plan Quarter (choose one): o SE o SW o NE o NW Section Township Range West of Meridian City/Municipality Province Postal Code Phone Fax Mailing Address o Same as above OR o send all correspondence to: Address Attention City/Municipality Province/State Postal Code Billing Address o Same as above OR o send invoice to: Address Attention City/Municipality Province/State Postal Code Email Phone Fax 03298 (Rev2018-08) Food Handling Permit Application Base of Operation/Storage Location - Mobile Units and Water Haulers Only Base of Operation Address Rural Land Location (choose one if applicable) Lot Block Plan Quarter (choose one): o SE o SW o NE o NW Section Township Range West of Meridian City/Municipality Vehicle Identification Number Tank ID License Plate AHS Decal Number (if known) Has the water hauling truck been used to haul any products other than potable water? o Yes o No Tank Capacity o Litres o Imperial Gallons o US Gallons Please include information for additional units on an additional page and submit it with this application. -

Peace Welcome to FAIRVIEW About Fairview & Welcome! Area
Heartof the Peace WELCOME TO FAIRVIEW ABOUT fairviEW & WELCOME! AREA • Originally settled by explorers and fur traders who came up the Peace River. Peace Country residents pride • The Peace Country produces canola, oats, peas, themselves on being self-reliant and hardy folk. They barley as well as honey and cattle ranching. It also will go out of their way to help a neighbor out accounts for 14% of Canada’s bison herd. Other • Fairview & area residents love their local hockey team - industries include oil & gas and forestry The Fairview Flyers. Come out for a game at the Fairplex • Fairview & area residents love music and boast Arena and cheer them on numerous music festivals each year. The most • Residents love outdoor activities. From sports to popular music is folk, country, Celtic, bluegrass and swimming, kayaking, canoeing, horseback riding, gospel boating, biking, skiing, running, walking, golfing, • Fairview & area has a vibrant arts community – the camping, quadding, skidooing, hunting, fishing, Fairview Fine Arts Centre as well as homemade gardening, barbecuing or just sitting around a campfire crafts and natural products, which are featured with good friends and family with homegrown local food and goodies at the Fairview Farmers’ Market, held at the Legion most Wednesdays WWW.FAIRVIEW.CA Heartof the SO siT BACK AND ENJOY A SLOWER PACE OF LifE WITH frESH air AND BEAUTifUL Peace NATUraL SCENERY. PiCK UP A NEW HOBBY OR ACTiviTY AND BEFORE YOU KNOW IT, FairviEW WILL FEEL LIKE HOME. GET CONNECTED WEBSITES www.fairview.ca - Fairview community information, resources, events calendar www.heartofthepeace.com - business development POSTER BOARDS AROUND TOWN resources Numerous organizations put up their event posters www.fairviewfcss.com - social support resources in and they are located at the Mall on Main, Canada Fairview & area Post Office, Freson Bros. -

Fairview Health Data and Summary
Alberta Health Primary Health Care - Community Profiles Community Profile: Fairview Health Data and Summary Version 2, March 2015 Alberta Health, Primary Health Care March 2015 Community Profile: Fairview Table of Contents Introduction .................................................................................................................................................. i Community Profile Summary .............................................................................................................. iii Zone Level Information .......................................................................................................................... 1 Map of Alberta Health Services North Zone ............................................................................................. 2 Population Health Indicators ..................................................................................................................... 3 Table 1.1 Zone versus Alberta Population Covered as at March 31, 2014 ............................................ 3 Table 1.2 Health Status Indicators for Zone versus Alberta Residents, 2012 and 2013 (BMI, Physical Activity, Smoking, Self-Perceived Mental Health) ............................................................................................... 3 Table 1.3 Zone versus Alberta Infant Mortality Rates (per 1,000 live births), Years 2011 – 2013 ................................................................................................................. 4 Local Geographic Area Level -

Beaverlodge Health Data and Summary
Alberta Health Primary Health Care - Community Profiles Community Profile: Beaverlodge Health Data and Summary Version 2, March 2015 Alberta Health, Primary Health Care March 2015 Community Profile: Beaverlodge Table of Contents Introduction .................................................................................................................................................. i Community Profile Summary .............................................................................................................. iii Zone Level Information .......................................................................................................................... 1 Map of Alberta Health Services North Zone ............................................................................................. 2 Population Health Indicators ..................................................................................................................... 3 Table 1.1 Zone versus Alberta Population Covered as at March 31, 2014 ............................................ 3 Table 1.2 Health Status Indicators for Zone versus Alberta Residents, 2012 and 2013 (BMI, Physical Activity, Smoking, Self-Perceived Mental Health) ............................................................................................... 3 Table 1.3 Zone versus Alberta Infant Mortality Rates (per 1,000 live births), Years 2011 – 2013 ................................................................................................................. 4 Local Geographic Area -

Westlock Health Data and Summary
Alberta Health Primary Health Care - Community Profiles Community Profile: Westlock Health Data and Summary Version 2, March 2015 Alberta Health, Primary Health Care March 2015 Community Profile: Westlock Table of Contents Introduction .................................................................................................................................................. i Community Profile Summary .............................................................................................................. iii Zone Level Information .......................................................................................................................... 1 Map of Alberta Health Services North Zone ............................................................................................. 2 Population Health Indicators ..................................................................................................................... 3 Table 1.1 Zone versus Alberta Population Covered as at March 31, 2014 ............................................ 3 Table 1.2 Health Status Indicators for Zone versus Alberta Residents, 2012 and 2013 (BMI, Physical Activity, Smoking, Self-Perceived Mental Health) ............................................................................................... 3 Table 1.3 Zone versus Alberta Infant Mortality Rates (per 1,000 live births), Years 2011 – 2013 ................................................................................................................. 4 Local Geographic Area Level -

Getting to Know Your Cancer Centre
Programs & Services at the Programs & Services at the Bonnyville Community Cancer Centre Cross Cancer Institute (CCI) in Edmonton Cancer Patient Navigator Look Good, Feel Better Cancer Patient Navigators are registered nurses This free workshop helps women manage the Getting to Know Your who can support you in understanding more appearance-related side effects of cancer. Tips, Cancer Centre about the next steps in your treatment and guide techniques and tools about skin care and how you in finding the right supports and resources to manage side effects are presented. you need throughout your cancer journey. lgfb.ca 1-800-914-5665 Bonnyville 780-826-3311 ext 3162 Patient and Family Resource Centre Gift Shop Mon–Fri Main floor 780-432-8456 9:00 am–4:00 pm Monday–Friday 780-826-3311 9:00am-12:00 noon Main floor ext 3253 The centre provides information, referral and 1:00pm-4:00pm library services. You may borrow books or The Gift Shop is open to patients, families and DVD’s and CD’s, chat with a knowledgeable staff. There are many items available to buy, such volunteer or view web-based videos. If you are as gifts, clothes and books. new to the CCI, call or stop by to arrange a personalized patient orientation. The orientation is customized to your needs and Bonnyville Patient and Family Resource Centre takes 20-50 minutes based on areas covered. A variety of patient education resources are Mon-Fri, 9:30 am–2:30 pm available. Wig Services Bonnyville Community Volunteers The Cross Cancer Institute also has wig Cancer Centre The Bonnyville Health Centre Auxiliary services and provide wig fittings, head shaves Bonnyville Healthcare Centre volunteers provide warm blankets, beverages, and head washes at no cost. -

Newborn Blood Spot Screening Collection Location Codes North Zone Last Updated: April 2020
Newborn Blood Spot Screening Collection Location Codes North Zone Last Updated: April 2020 Alternate Facility Collection Main Phone AHS Facility Name Services Offered Zone Zone # Address City/Town Province Postal Code Name Location Code Number Athabasca Athabasca Community Health Community Health Public Health ACHSPH North 5 780-675-2231 3401 48th Ave Athabasca AB T9S 1M7 Services Services & Mental Health Athabasca Healthcare Centre Lab-Inpatient ATHCLI North 5 780-675-6000 3100 48 Avenue Athabasca AB T9S 1M9 Athabasca Healthcare Centre Lab-Outpatient ATHCLO North 5 780-675-6000 3100 48 Avenue Athabasca AB T9S 1M9 Birth Facility (Post- Athabasca Healthcare Centre ATHCPP North 5 780-675-6000 3100 48 Avenue Athabasca AB T9S 1M8 Partum Unit) Barrhead Community Health Services Public Health BHCSPH North 5 780-674-3408 6203 49 Street Barrhead AB T7N 1A1 Barrhead Healthcare Centre, Barrhead Healthcare Centre Mental Health & Lab-Inpatient BHHCLI North 5 780-674-2221 4815 51 Avenue Barrhead AB T7N 1M1 Community Cancer Centre Barrhead Healthcare Centre, Barrhead Healthcare Centre Mental Health & Lab-Outpatient BHHCLO North 5 780-674-2221 4815 51 Avenue Barrhead AB T7N 1M1 Community Cancer Centre Barrhead Healthcare Centre, Birth Facility (Post- Barrhead Healthcare Centre Mental Health & BHHCPP North 5 780-674-2221 4815 51 Avenue Barrhead AB T7N 1M1 Partum Unit) Community Cancer Centre Beaver First Nation FN Community BEAVFN North 5 780-927-3544 Bag 2700, High Level AB T0H 1Z0 Beaverlodge Public Beaverlodge Community Health Health Centre & Public