January 19, 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Legislative Schedule
21st Calendar Day EIGHTY-FIRST OREGON LEGISLATIVE ASSEMBLY 2021 Regular Session JOINT Legislative Schedule MONDAY, FEBRUARY 8, 2021 SENATE OFFICERS PETER COURTNEY, President LORI L. BROCKER, Secretary of the Senate JAMES MANNING, JR, President Pro Tempore CYNDY JOHNSTON, Sergeant at Arms HOUSE OFFICERS TINA KOTEK, Speaker TIMOTHY G. SEKERAK, Chief Clerk PAUL HOLVEY, Speaker Pro Tempore BRIAN MCKINLEY, Sergeant at Arms SENATE CAUCUS LEADERS ROB WAGNER, Majority Leader FRED GIROD, Republican Leader ELIZABETH STEINER HAYWARD, Deputy Majority Leader CHUCK THOMSEN, Deputy Republican Leader LEW FREDERICK, Majority Whip LYNN FINDLEY, Assistant Republican Leader SARA GELSER, Majority Whip DENNIS LINTHICUM, Republican Whip MICHAEL DEMBROW, Assistant Majority Leader KATE LIEBER, Assistant Majority Leader HOUSE CAUCUS LEADERS BARBARA SMITH WARNER, Majority Leader CHRISTINE DRAZAN, Republican Leader ANDREA SALINAS, Majority Whip DANIEL BONHAM, Deputy Republican Leader JULIE FAHEY, Deputy Majority Whip DUANE STARK, Republican Whip PAM MARSH, Assistant Majority Leader KIM WALLAN, Assistant Republican Whip RACHEL PRUSAK, Assistant Majority Leader BILL POST, Assistant Deputy Republican Leader JANEEN SOLLMAN, Assistant Majority Leader SHELLY BOSHART DAVIS, Assistant Republican Leader CEDRIC HAYDEN, Assistant Republican Leader RICK LEWIS, Assistant Republican Leader NO FLOOR SESSIONS SCHEDULED TODAY SENATE CONVENES AT 11:00 AM ON THURSDAY, FEBRUARY 11, 2021 HOUSE CONVENES AT 11:00 AM ON TUESDAY, FEBRUARY 9, 2021 LEGISLATIVE ACCESS NUMBERS: LEGISLATIVE INTERNET -

House Speaker Tina Kotek Announces Committees Urgent Issues Will Get Dedicated Attention in New Committees
OFFICE OF THE HOUSE SPEAKER 900 Court St., N.E., Room H-269 Salem OR 97301 http://www.oregonlegislature.gov/kotek NEWS RELEASE December 31, 2020 Danny Moran, 503-986-1204 [email protected] House Speaker Tina Kotek Announces Committees Urgent issues will get dedicated attention in new committees SALEM – Oregon House Speaker Tina Kotek on Thursday announced House committees for the 2021 Legislative Session. In addition to the standard policy and budget committees, the Oregon House of Representatives will have new committees in the upcoming session to address timely issues, including wildfire recovery, redistricting, institutional reform of the Legislature, as well as subcommittees focusing on COVID-19 response, equitable policing and the return of a policy committee dedicated to early childhood issues. “Oregonians are facing crises that demand urgent action. The House is ready to lead on the issues that matter most in people’s lives right now. We also need to create the space to have a focused conversation about long-term, transformational changes to modernize the people’s legislature,” Speaker Kotek said. “I’m grateful for the diverse perspectives that my colleagues will bring as we all work together to help Oregonians navigate the big challenges that lie ahead.” Speaker Kotek communicated directly with every returning and new member of the Oregon House of Representatives before deciding on committee assignments, taking the time to weigh and discuss their priorities, interests and notable experience. She also consulted with both caucus leaders before finalizing the assignments. The House will convene on Monday, January 11 to swear in members. -

Legislative Update
LEGISLATIVE UPDATE Prepared for OAFP April 4, 2021 HB 2510 – Safe Gun Storage The House Health Committee passed this bill on party lines. It would require gun owners to lock their firearms, and make them liable for injuries caused by a firearm stored unsecurely. Rep. Cedric Hayden (R-Roseburg) told a story about his rural constituents responsibly using firearms in their own defense, saying, “I’m very concerned about my rural constituents’ ability to protect their own.” Rep. Christine Drazan (R-Canby) said she was against the bill and had concerns about working this type of legislation remotely. She said her office received over 7000 emails on gun legislation before the Legislature, including this bill, largely opposing it. Committee Chair Rachel Prusak (D-Tualatin) responded that her office also received lots of public input on this bill, largely in favor. The bill now goes to the House floor. SB 772 – Naturopath Pay Parity The Senate Health Committee held a public hearing on this bill, which would require individual and group insurance policies to pay naturopaths the same as other providers, using the same methodology. Dr. Jeff Clark, Oregon Association of Naturopathic Physicians, told the Committee that health insurers refuse to negotiate with naturopathic doctors on rates. He said Healthnet “shamelessly” pays naturopaths 20%, Moda 40%, and BlueCross BlueShield 60% of what they pay other providers. Dr. Clark clarified that SB 722 does not lock in a fee-for-service model, and an amendment is being drafted to remove the emergency clause in order to give insurers more time to implement the new pay structure if passed. -
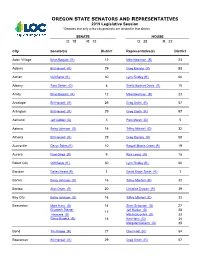
OREGON STATE SENATORS and REPRESENTATIVES 2019 Legislative Session * Denotes That Only a Few City Precincts Are Located in That District
OREGON STATE SENATORS AND REPRESENTATIVES 2019 Legislative Session * Denotes that only a few city precincts are located in that district SENATE HOUSE D: 18 R: 12 D: 38 R: 22 City Senator(s) District Representative(s) District Adair Village Brian Boquist (R) 12 Mike Nearman (R) 23 Adams Bill Hansell (R) 29 Greg Barreto (R) 58 Adrian Cliff Bentz (R ) 30 Lynn Findley (R) 60 Albany Sara Gelser (D) 8 Shelly Boshart Davis (R) 15 Amity Brian Boquist (R) 12 Mike Nearman (R) 23 Antelope Bill Hansell (R) 29 Greg Smith (R) 57 Arlington Bill Hansell (R) 29 Greg Smith (R) 57 Ashland Jeff Golden (D) 3 Pam Marsh (D) 5 Astoria Betsy Johnson (D) 16 Tiffiny Mitchell (D) 32 Athena Bill Hansell (R) 29 Greg Barreto (R) 58 Aumsville Denyc Boles (R) 10 Raquel Moore-Green (R) 19 Aurora Fred Girod (R) 9 Rick Lewis (R) 18 Baker City Cliff Bentz (R ) 30 Lynn Findley (R) 60 Bandon Dallas Heard (R) 1 David Brock Smith (R) 1 Banks Betsy Johnson (D) 16 Tiffiny Mitchell (D) 32 Barlow Alan Olsen (R) 20 Christine Drazan (R) 39 Bay City Betsy Johnson (D) 16 Tiffiny Mitchell (D) 32 Beaverton Mark Hass (D) 14 Sheri Schouten (D) 27 Elizabeth Steiner Jeff Barker (D) 28 17 Hayward (D) Mitch Greenlick (D) 33 Ginny Burdick (D) 18 Ken Helm (D) 34 Margaret Doherty (D) 35 Bend Tim Knopp (R) 27 Cheri Helt (R) 54 Boardman Bill Hansell (R) 29 Greg Smith (R) 57 City Senator(s) District Representative(s) District Bonanza Dennis Linthicum (R) 28 Werner Reschke (R) 56 Brookings Dallas Heard (R) 1 David Brock Smith (R) 1 Brownsville Lee Beyer (D) 6 Marty Wilde (D) 11 Burns Cliff Bentz (R ) 30 Lynn Findley (R) 60 Butte Falls Dennis Linthicum (R) 28 55 Vacant Seat Canby Alan Olsen (R) 20 Christine Drazan (R) 39 Cannon Beach Betsy Johnson (D) 16 Tiffiny Mitchell (D) 32 Canyon City Cliff Bentz (R ) 30 Lynn Findley (R) 60 Canyonville Dallas Heard (R) 1 Gary Leif (R) 2 Carlton Brian Boquist (R) 12 Ron Noble (R) 24 Cascade Locks Chuck Thomsen (R) 26 Anna Williams (D) 52 Cave Junction Herman Baertschiger Jr. -

Regular Document
Libertarian Party of Oregon 2020 Primary Election Voters’ Guide US Senator US Senator Gary Dye Jodie Ann Newell Libertarian Libertarian I am running for US Senate in hopes of Occupational Background: Small reforming the Libertarian Party's Business Banking and Commercial No photo submitted message so that the general public will No photo submitted Lending actually entrust us with transforming our society to one that is libertarian. Governmental Experience: Jantzen Because – let's face it – our current Beach Moorage Inc Homeowner’s message and political tactics have failed Association Board of Directors miserably at the polls, and after almost 50 years of effort, our nation is closer to We are living in an interesting time. becoming totalitarian than it is libertarian. Our party's status is even During the Coronavirus Pandemic, we experienced what some worse – Libertarians have so little faith in the efficacy of our own economists are referring to as The Great Suppression. Small message, tactics, and candidates, that many will choose to not vote businesses were hit the hardest by the economic shutdown. People are for Libertarians, let alone support them with their time and money not feeling safe. Proponents of gun control are now trying to buy guns such that we might actually have a chance at winning an election. — this can be attributed to a feeling of economic insecurity. As your Clearly, something has to change. Senator, I will work to eliminate federal regulations that harm small businesses and reward big corporations. States should not be forced to My campaign will not only address the goodness of Libertaria, but stay open, but they should be incentivized to do so. -

Today We Are Unified in Calling on Residents and Visitors to Our
Today we are unified in calling on residents and visitors to our respective communities to refrain from violence in the exercise of our First Amendment rights to free speech and to peaceably assemble. Black Lives Matter. Violence has no place in civic engagement and protest. Throughout 2020, and in too many years prior, we have born witness to instances of racial injustice, police brutality and the rise of white supremacist rhetoric throughout our country, and right here at home. Even now we are experiencing unhelpful and inflammatory comments and acts, from many quarters, including the highest office in the land. The overwhelming majority of our community who have risen to protest for social justice and against racial inequities have done so peacefully, in keeping with public health guidelines and within the bounds protected by our state and federal constitutions. Unfortunately, there are some individuals who have chosen violence over peaceful protest, violence towards other protestors, violence towards police officers and even an instance of deadly violence experienced recently in downtown Portland. While we recognize the outrage toward racial injustice is the foundation for the past 100+ days of protest, we call on everyone in our community seeking to confront racial injustice and to demand police accountability to forgo the path of violence. We invite every member of our respective communities to continue to engage with our governments, to hold us accountable and to contribute to and facilitate a transformation away from racist systems and towards a more equitable, just community. Similarly, we ask those who may want to demonstrate to do so peacefully and safely. -

1% 2% 4% 2% 29% 8% 5%
November 3, 2020 Election 8QR৽FLDO5HVXOWV Summary of City Measures Types of City Measures Results of City Measures 2% Bonds 2% 8% Annexation Other 4% 31% 29% Marijuana Charter Failed Amendments 71% Passed 29% Bonds 2% 5% Fees Gas Tax All Local Government Measures 1% Regional 14% RFPD/Fire 37% Districts Cities 14% Other Special Districts 16% School 18% Districts Counties All Measures by Local Governments Local Government Type Number of Measures Passed Failed Cities 38 71% 29% Counties 19 53% 47% School Districts/Community 17 82% 18% Colleges RFPD/Fire Districts 15 73% 27% Other Special Districts 14 71% 29% Regional 1 0% 100% Bond Measures by Local Governments Local Government Type Number of Bond Measures Passed Failed Cities 1 100% 0% Counties 1 100% 0% School Districts/Community 14 86% 14% Colleges RFPD/Fire Districts 1 100% 0% Other Special Districts 2 100% 0% Regional 0 N/A N/A Levy Measures by Local Governments Local Government Type Number of Levy Measures Passed Failed Cities 11 64% 36% Counties 2 0% 100% School Districts/Community 3 100% 0% Colleges RFPD/Fire Districts 8 75% 25% Other Special Districts 8 75% 25% Regional 0 N/A N/A Details of City Measures Banks Annexation Annexes 1.03 acres of continuous land to the City of Banks. Pass Yes No 585 67% 282 33% Bend Bond $190 Million; For traffic flow, East-West connections, neighborhood safety improvements. Pass Yes No 33,154 58% 23,847 42% Charter Charter Coquille Cove Amendment Amendment Amends charter to allow nomination of Adopts new charter for Cove city candidates by paying a fee as an government. -

2016 POLITICAL DONATIONS Made by WEYERHAEUSER POLITICAL ACTION COMMITTEE (WPAC)
2016 POLITICAL DONATIONS made by WEYERHAEUSER POLITICAL ACTION COMMITTEE (WPAC) ALABAMA U.S. Senate Sen. Richard Shelby $2,500 U.S. House Rep. Robert Aderholt $5,000 Rep. Bradley Byrne $1,500 Rep. Elect Gary Palmer $1,000 Rep. Martha Roby $2,000 Rep. Terri Sewell $3,500 ARKANSAS U.S. Senate Sen. John Boozman $2,000 Sen. Tom Cotton $2,000 U.S. House Rep. Elect Bruce Westerman $4,500 FLORIDA U.S. House Rep. Vern Buchanan $2,500 Rep. Ted Yoho $1,000 GEORGIA U.S. Senate Sen. Johnny Isakson $3,000 U.S. House Rep. Rick Allen $1,500 Rep. Sanford Bishop $2,500 Rep. Elect Buddy Carter $2,500 Rep. Tom Graves $2,000 Rep. Tom Price $2,500 Rep. Austin Scott $1,500 IDAHO U.S. Senate Sen. Mike Crapo $2,500 LOUISIANA U.S. Senate Sen. Bill Cassidy $1,500 U.S. House Rep. Ralph Abraham $5,000 Rep. Charles Boustany $5,000 Rep. Garret Graves $1,000 Rep. John Kennedy $2,500 Rep. Stephen Scalise $3,000 MAINE U.S. Senate Sen. Susan Collins $1,500 Sen. Angus King $2,500 U.S. House Rep. Bruce Poliquin $2,500 MICHIGAN U.S. Senate Sen. Gary Peters $1,500 Sen. Debbie Stabenow $2,000 MINNESOTA U.S. Senate Sen. Amy Klobuchar $2,000 U.S. House Rep. Rick Nolan $1,000 Rep. Erik Paulsen $1,000 Rep. Collin Peterson $1,500 MISSISSIPPI U.S. Senate Sen. Roger Wicker $4,000 U.S. House Rep. Gregg Harper $4,000 Rep. Trent Kelly $3,000 Rep. -

Oregon State House of Representatives (Parts of Coos, Curry, (Parts of Lincoln, Polk, HD 1 Douglas, & Josephine Counties) HD 10 Tillamook, & Yamhill) Rep
Oregon State House of Representatives (parts of Coos, Curry, (parts of Lincoln, Polk, HD 1 Douglas, & Josephine Counties) HD 10 Tillamook, & Yamhill) Rep. David Brock Smith Max Sherman A tireless champion for rural Oregonians, A longtime Tillamook County Farm Bureau David is an outstanding advocate for families leader, Max has deep roots in agriculture and working in farming, ranching, and natural the north coast community. He has invested resources. time testifying in Salem and understands how public policy impacts farm and ranch families. (parts of Douglas, Jackson, & HD 2 Josephine) Rep. Gary Leif HD 11 (parts of Lane & Linn) A former Douglas County Commissioner, Gary Katie Boshart Glaser has been a steadfast voice for farmers and A dedicated Linn County Farm Bureau board ranchers since entering the Legislature. member and farmer, Katie understands the issues that impact farm and ranch families and will work toward common-sense HD 3 (part of Josephine) solutions as a legislator. Lily Morgan As a former sergeant with the Josephine HD 15 (parts of Benton & Linn) &RXQW\6KHULII¶V2I¿FHDQG-RVHSKLQH&RXQW\ Rep. Shelly Boshart Davis Commissioner, Lily will bring decades of public service, common sense, and experience with A longtime Farm Bureau leader, Shelly has rural Oregon to the Legislature. been an unwavering advocate and champion for agriculture in the Legislature. She recently received an OFB Top Hand Award for her HD 4 (parts of Jackson & Josephine) tireless work on behalf of Oregon’s farmers, Rep. Duane Stark ranchers, and small business owners. A dedicated advocate for his constituents, Duane is an effective representative for rural HD 17(parts of Linn & Marion) families at the state Capitol. -

House Republican Leader Announces Leadership Team
From the HOUSE REPUBLICAN OFFICE For Immediate Release Thursday, December 31 2020 Contact: Jihun Han, 503-501-1677 Email: [email protected] House Republican Leader Announces 2021 Caucus Leadership Team Salem, ORE. – Today, House Republican Leader Christine Drazan (R-Canby) announced the leadership team as the caucus heads into the 2021 Legislative Session: “I am pleased to announce the House Republican leadership team as we prepare for the 2021 Legislative Session,” said House Republican Leader Christine Drazan (R-Canby). “This leadership team represents rural, suburban and urban areas across the state, and the team’s diverse backgrounds and professional experiences will serve Oregon well. As we continue to face challenging issues amplified by the ongoing COVID-19 pandemic and wildfire recovery efforts, Oregonians expect strong and steady leaders who will fight for their future, and that’s what the House Republican Leadership team will do.” Oregon House Republican Leadership Team Representative Christine Drazan (R-Canby), House Republican Leader Representative Daniel Bonham (R-The Dalles), House Republican Deputy Leader Representative Duane Stark (R-Grants Pass), House Republican Whip Representative Kim Wallan (R-Medford), House Republican Assistant Whip Representative Bill Post (R-Keizer), House Republican Assistant Deputy Representative Shelly Boshart Davis (R-Albany), House Republican Assistant Leader Representative Cedric Hayden (R-Roseburg), House Republican Assistant Leader Representative Rick Lewis (R-Silverton), House Republican Assistant Leader Representative Greg Smith (R-Heppner), Vice-Chair of Ways and Means, ex-officio member ### . -

House Committee on Education
HOUSE COMMITTEE ON EDUCATION March 11, 2019 Hearing Room D 03:00 PM MEMBERS PRESENT: Rep. Margaret Doherty, Chair Rep. Teresa Alonso Leon, Vice-Chair Rep. Cheri Helt, Vice-Chair Rep. Diego Hernandez Rep. Courtney Neron Rep. Jeff Reardon Rep. E. Werner Reschke Rep. Janeen Sollman Rep. Kim Wallan STAFF PRESENT: Alethia Miller, LPRO Analyst Desiree’ Leon-Chavez, Committee Assistant EXHIBITS: Exhibits from this meeting are available here MEASURES/ISSUES: HB 2023 – Public Hearing HB 2441 – Public Hearing HB 2940 – Public Hearing HB 2358 – Work Session HB 2964 – Work Session HB 2026 – Work Session HB 2224 – Public Hearing 00:00:05 Meeting Called to Order 00:00:06 Chair Doherty 00:00:30 HB 2023 - Public Hearing 00:00:31 Chair Doherty 00:00:37 Alethia Miller, LPRO Analyst 00:01:49 Rep. Diego Hernandez, House District 47 00:02:34 EXHIBIT 1: Jessica Ventura, Legislative Director, Oregon Department of Education 00:06:00 EXHIBITS 2-4: Joseph Gallegos, Pacific University; Oregon Commission on Hispanic Affairs 00:09:04 Vice-Chair Helt 00:11:55 Laura Curtis, Basic Rights Oregon 00:13:30 EXHIBIT 5: witness registration This recording log is in compliance with Senate and House Rules. For complete contents, refer to the digital audio recording. HED 03/11/2019 Page 2 of 7 00:13:32 The following is submitted for the record without public testimony: EXHIBIT 6: Caroline Bleckmann, Licensed Clinical Social Worker, Benson Wellness Clinic EXHIBIT 7: Jenny Lee, Advocacy Director, Coalition of Communities of Color EXHIBIT 8: Kelli Horvath, Public Affairs Consultant, -

Candidates and Measures on the Ballot
County: MULTNOMAH Date : 9/11/2020 3:41:23 PM Proof Ballot Content Report No. : E-019 Election : 11/03/2020 - November General Election 2020 Federal Offices Federal President and Vice President Vote for 1 4 Year Term Donald J Trump / Michael R Pence Republican Joseph R Biden / Kamala D Harris Democrat Jo Jorgensen / Jeremy (Spike) Cohen Libertarian Howie Hawkins / Angela Walker Pacific Green Dario Hunter / Dawn Neptune Adams Progressive Number Candidates Filed: 5 US Senator Vote for 1 6 Year Term Jo Rae Perkins Republican Jeff Merkley Democrat, Independent, Working Families Ibrahim A Taher Pacific Green, Progressive Gary Dye Libertarian Number Candidates Filed: 4 Contest Total: 2 US Representative, 1st District US Representative, 1st District Vote for 1 2 Year Term Suzanne Bonamici Democrat, Working Families Christopher C Christensen Republican Number Candidates Filed: 2 Contest Total: 1 US Representative, 3rd District US Representative, 3rd District Vote for 1 2 Year Term Earl Blumenauer Democrat, Working Families Joanna Harbour Republican Alex C DiBlasi Pacific Green Josh Solomon Libertarian Number Candidates Filed: 4 Contest Total: 1 US Representative, 5th District US Representative, 5th District Vote for 1 2 Year Term Matthew James Rix Libertarian Amy Ryan Courser Republican Kurt Schrader Democrat Number Candidates Filed: 3 Contest Total: 1 Oregon Centralized Voter Registration Page : 1 County: MULTNOMAH Date : 9/11/2020 3:41:23 PM Proof Ballot Content Report No. : E-019 Election : 11/03/2020 - November General Election 2020 Partisan