BIONET Textbook 2 ______
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A DNA Database in the NHS: Your Freedom up for Sale?
A DNA database in the NHS: Your freedom up for sale? May 2013 In April 2013, the Caldicott Committee, including Government Chief Scientist Sir Mark Walport, proposed new rules for data-sharing which would allow the Government to build a DNA database of the whole population of England in the NHS by stealth.1 The plan is to make NHS medical records and people’s genetic information available to commercial companies and to use public-private partnerships to build a system where all private information about every citizen is also accessible to the police, social workers, security services and Government. The Wellcome Trust, which was involved in the Human Genome Project and was led by Walport for ten years, has produced a plan which involves including a variant file, containing the whole genome of every person minus the reference genome, as an attachment to every medical record in the NHS in England.2 This data would be made available to ‘researchers’ (including commercial companies) for data-mining in the cloud and personalised risk assessments would be returned to individuals. The aim is to transform the NHS in line with proposals developed more than a decade ago by former GlaxoSmithKline Chairman Sir Richard Sykes. This is expected to massively expand the market for medicines, medical tests and other products, such as supplements and cholesterol-lowering margarines, by allowing products to be marketed to individuals based on personal risk assessments, created using statistical analysis of genetic data, medical records and other health information. The proposal to build a DNA database in the NHS was endorsed by the Human Genomics Strategy Group in 20123,4 and the Government (led by Prime Minister David Cameron) has quietly adopted this recommendation without telling members of the public. -
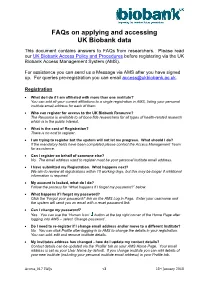
Faqs on Applying and Accessing UK Biobank Data
FAQs on applying and accessing UK Biobank data This document contains answers to FAQs from researchers. Please read our UK Biobank Access Policy and Procedures before registering via the UK Biobank Access Management System (AMS). For assistance you can send us a Message via AMS after you have signed up. For queries pre-registration you can email [email protected]. Registration What do I do if I am affiliated with more than one institute? You can add all your current affiliations to a single registration in AMS, listing your personal institute email address for each of them. Who can register for access to the UK Biobank Resource? The Resource is available to all bona fide researchers for all types of health-related research which is in the public interest. What is the cost of Registration? There is no cost to register. I am trying to register but the system will not let me progress. What should I do? If the mandatory fields have been completed please contact the Access Management Team for assistance. Can I register on behalf of someone else? No. The email address used to register must be your personal institute email address. I have submitted my Registration. What happens next? We aim to review all registrations within 10 working days, but this may be longer if additional information is required. My account is locked, what do I do? Follow the process for “What happens if I forget my password?” below. What happens if I forget my password? Click the ‘Forgot your password?’ link on the AMS Log in Page. -

Stem Cells: Biology and Clinical Potential
African Journal of Biotechnology Vol. 10(86), pp. 19929-19940, 30 December, 2011 Available online at http://www.academicjournals.org/AJB DOI: 10.5897/AJBX11.046 ISSN 1684–5315 © 2011 Academic Journals Review Stem cells: Biology and clinical potential Faris Q. B. Alenzi1* and Ali H. Bahkali 2 1College of Applied Medical Sciences, Prince Salman University, Al-Kharj, Saudi Arabia. 2College of Science, KSU, Riyadh, Saudi Arabia. Accepted 28 December, 2011 Stem cell technology has developed rapidly in recent years to the point that we can now envisage its future use in a variety of therapeutic areas. This review seeks to summarize the types and sources of stem cells that may be utilized in this way, their pattern of development, their plasticity in terms of differentiation and transdifferentiation, their ability to self-renew, the privileged microenvironment in which they are housed, their cell surface markers used to track them, issues relating to their transfection, and their fate. Particular reference is made, as prime examples, to how both the function of mesenchymal and neural stem cells are being studied experimentally, and currently used clinically in certain circumstances, towards the ultimate aim of their mainstream therapeutic use. Key words: Stem cells, apoptosis, differentiation, mesenchymal and neural stem cells, therapy. INTRODUCTION Stem cells are characterized by their ability to undergo cells (MSCs) can proliferate extensively in vitro , and symmetric cell division resulting in one undifferentiated differentiate under appropriate conditions into bone, daughter cell and one committed daughter cell. The cartilage and other mesenchymal tissues (Brazelton et undifferentiated daughter cell can maintain a population al., 2000). -

What Does It Mean to Take an Ethics+ Approach to Global Biobank Governance?
Edinburgh Research Explorer What does it mean to take an ethics+ approach to global biobank governance? Citation for published version: Laurie, G 2017, 'What does it mean to take an ethics+ approach to global biobank governance?', Asian Bioethics Review, vol. 9, no. 4, pp. 285-300. https://doi.org/10.1007/s41649-017-0030-z Digital Object Identifier (DOI): 10.1007/s41649-017-0030-z Link: Link to publication record in Edinburgh Research Explorer Document Version: Peer reviewed version Published In: Asian Bioethics Review Publisher Rights Statement: This is a post-peer-review, pre-copyedit version of an article published in Asian Bioethics Review. The final authenticated version is available online at: https://link.springer.com/article/10.1007/s41649-017-0030-z General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 01. Oct. 2021 What Does It Mean to Take an Ethics+ Approach to Global Biobank Governance? Graeme Laurie School of Law, University of Edinburgh Abstract: This article re-examines and fundamentally re-assesses the symbiotic relationship between law and ethics in the governance and regulation of biobanks as a global phenomenon. -
Property Redux. Ownership of Human Tissue and the Governance of Post-Genomic Research Biobanks
PhD degree in “Foundations and Ethics of the Life Sciences” European School of Molecular Medicine (SEMM) and University of Milan Faculty of Medicine Settore disciplinare: M-FIL/02 PROPERTY REDUX. OWNERSHIP OF HUMAN TISSUE AND THE GOVERNANCE OF POST-GENOMIC RESEARCH BIOBANKS Bettina Schmietow IFOM-IEO Campus, Milan Matricola n. R08920 Supervisor: Dr. Matteo Mameli IFOM-IEO Campus, Milan Anno accademico 2012-2013 Abstract Biobank-based genomic research is considered instrumental to realize Personalised Medicine and considerable benefits for diagnosis and therapy of many common complex diseases. It raises manifold ethical and regulatory challenges which are discussed extensively, the main focus being on adaptations of Informed Consent to the emerging research context. This study highlights challenges to the strongly individualistic focus of classical research ethics in confrontation with biobank development. The debate on adequate protections for individual donor-participants tends towards deflationary accounts of participant rights, in which in particular the dimension of potential property in human tissue and genomic information is undervalued. Criticizing the common bioethical and legal stance that there can and should be no property in the human body and its parts, the close conceptual connections between privacy, property and consent underlying the protection of a more substantive version of participant integrity are emphasized. While ultimately the framework of traditional, in particular individual property rights is ill-suited to safeguard participant and public interests in research, property discourse is fundamental to advance discussion on the direction biobank ethics and governance should take by 1) taking serious the reordering of individual, group and societal interests in biobank research, 2) clarifying strength and limits of claims to “autonomy” and 3) refocusing to public or common goods biobank research should provide. -

Human Stem Cells: Ethical and Policy Issues
HUMAN STEM CELLS AN ETHICAL OVERVIEW CONTENTS PART I: WHAT ARE STEM CELLS AND WHAT DO THEY DO? What are stem cells? Page 4 Different types of stem cells Page 5 Different sources of stem cells Page 7 Preliminary findings and research possibilities Page 10 Focusing on human embryonic stem (ES) cells Page 11 PART II: ETHICAL ISSUES IN HUMAN EMBRYONIC STEM (ES) CELL RESEARCH The status of the human embryo Page 14 Donating embryos Page 18 Federal funding for human embryonic stem (ES) cell research Page 20 Opinions Page 23 Other ethical issues Page 25 PART III: SUGGESTED MATERIALS Websites Page 28 Books Page 28 Articles Page 29 PART IV: GLOSSARY AND REFERENCES Glossary Page 36 References Page 38 2 PART I WHAT ARE STEM CELLS AND WHAT DO THEY DO? 3 What are stem cells? Stem cells are “blank” cells found in human beings that are capable of developing into the many different kinds of cells you find in the human body. The human body contains stem cells because all human beings start out as only one cell, a zygote, which is a fertilized egg. The zygote grows into a human embryo by dividing first from one cell into two, then from two cells into four, and so on. In the first few divisions in the human embryo each cell contains the ability to make all the cells in the human body. As the cells of the human embryo continue to divide, the cells begin to specialize. The new cells are no longer completely “blank” because they begin to take on the functioning of a particular tissue or organ, such as the lungs or the nervous tissue. -

Select Bibliography
Select Bibliography (A more detailed Bibliography is available on the The Federation Press website) Aatre, Rajani, and Sharlene Day, ‘Psychological issues in genetic testing for inherited cardiovascular diseases’ (2011) 4 Circulation: Cardiovascular Genetics 87 Abadie, Alberto, and Sebastien Gay, ‘The Impact of Presumed Consent Legislation on Cadaveric Organ Donation: A Cross-Country Study’ (2006) 25(4) Journal of Health Economics 599 Abbing, HDC Roscam, Jan KM Gevers, Ewoud H Hondius and JH Hubben (eds), Health Law, Human Rights and the Bioethics Convention: Essays in Honour of Henriette Abbing (Martinus Nijhoff, Amsterdam, 2005) Abbott, FM, ‘The enduring enigma of TRIPS: A challenge for the world economic system’ (1998) 1 Journal of International Economic Law 497 Abbott, Katherine, et al, ‘Families Looking Back: One Year After Discussion of Withdrawal or Withholding of Life-Sustaining Support (2001) 29(1) Critical Care Medicine 197 Abegunde, Dele O, et al, ‘The Burden and Costs of Chronic Diseases in Low-Income and Middle-Income Countries’ (2007) 370 The Lancet 1929 Abel, Richard, Politics by Other Means: Law in the Struggle Against Apartheid 1980 – 1994 (Routledge, New York and London, 1st ed, 1995) Abrams, Paula, ‘The Bad Mother: Stigma, Abortion and Surrogacy’ (2015) 43 Journal of Law, Medicine and Ethics 179 ACCC, ‘ACCC tackles Homeopathy Plus! Whooping Cough claims’, <http://www.accc.gov.au/content/ index.phtml/itemId/1049609/fromItemId/142> ACMG Board of Directors, ‘ACMG Policy Statement: Updated Recommendations Regarding Analysis -

New Genetics, New Social Formations
New Genetics, New Social Formations The genomic era requires more than just a technical understanding of gene structure and function. New technological options cannot survive without being entrenched in networks of producers, users and various services. New genetic technologies cut across a range of public domains and private lifeworlds, often appearing to gen- erate an institutional void in response to the complex challenges they pose. Chap- ters in this volume discuss a variety of these novel manifestations across both health and agriculture, including: gene banks intellectual property rights committees of inquiry non-governmental organisations (NGOs) national research laboratories These are explored in such diverse locations as Amazonia, China, Finland, Israel, the UK and the USA. This volume reflects the rapidly changing scientific, clinical and social environment within which new social formations are being constructed and reconstructed. It brings together a range of empirical and theoretical insights that serve to help better understand complex, and often contentious, innovative processes in the new genetic technologies. Peter Glasner is Professorial Fellow in the Economic and Social Research Council’s Centre for Economic and Social Aspects of Genomics at Cardiff University. He is Co-editor of the journals New Genetics and Society and 21st Century Society.He has a longstanding research interest in genetics, innovation and science policy. He is an Academician of the Academy of Learned Societies in the Social Sciences. Paul Atkinson is Distinguished Research Professor in Sociology at Cardiff University, where he is Associate Director of the ESRC Centre for Economic and Social Aspects of Genomics. He has published extensively on the sociology of medical knowledge and qualitative research methods. -

Bridging the Cultural Divide in California's
“SO FAR LEFT, WE’RE RIGHT”: BRIDGING THE CULTURAL DIVIDE IN CALIFORNIA’S STEM CELL CONTROVERSY by Joan Kathleen Higgs BA, Simon Fraser University, 2005 THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF ARTS in the Department of Sociology and Anthropology Faculty of Arts and Social Sciences © Joan Kathleen Higgs 2010 SIMON FRASER UNIVERSITY Spring 2010 All rights reserved. However, in accordance with the Copyright Act of Canada, this work may be reproduced, without authorization, under the conditions for Fair Dealing. Therefore, limited reproduction of this work for the purposes of private study, research, criticism, review and news reporting is likely to be in accordance with the law, particularly if cited appropriately. Approval Name: Joan Kathleen Higgs Degree: Master of Arts Title of Thesis: “So Far Left, We’re Right”: Bridging the Cultural Divide in California’s Stem Cell Controversy Examining Committee: Dr. Ann Travers Chair Assistant Professor of Sociology Simon Fraser University Dr. Dara Culhane Senior Supervisor Associate Professor of Anthropology Simon Fraser University Dr. Michael Kenny Supervisor Professor of Anthropology Simon Fraser University Dr. Marina Morrow Internal Examiner Assistant Professor, Faculty of health Sciences Simon Fraser University Date Defended/Approved: April 13, 2010 ii Declaration of Partial Copyright Licence The author, whose copyright is declared on the title page of this work, has granted to Simon Fraser University the right to lend this thesis, project or extended essay to users of the Simon Fraser University Library, and to make partial or single copies only for such users or in response to a request from the library of any other university, or other educational institution, on its own behalf or for one of its users. -

Proposal to Create a Graduate Minor in Bioethics
Center for Bioethics and Medical Humanities Proposal for a Graduate Minor in Bioethics June, 2015 [Revised September, 2015] [Revised October, 2015] Graduate Studies Committee Proposing the Graduate Program MA in Bioethics: Ryan Nash, MD, MA (Chair) Alan Litsky, MD, ScD Karla Zadnik, OD, PhD 1. Title of the proposed graduate minor: Graduate Minor in Bioethics 2. Rational for its development Currently, the University does not offer any programs on the graduate level in bioethics. In light of the established presence of bioethics as a multidisciplinary and interdisciplinary field, the Center for Bioethics was launched in 2013 with the task of addressing this need. An MA in Bioethics has been proposed, and a Graduate Minor in Bioethics is a natural programmatic extension of the proposed MA in Bioethics. In short, the primary rational for developing the Graduate Minor is to offer scholarship and training in ethics for graduate students in a field that warrants the University’s attention. As part of the planning process for the MA program, Ryan Nash (Director, Center for Bioethics) met with deans and directors from the OSU health campus colleges and schools—including College of Medicine, Biomedical Science, Health and Rehabilitation Sciences, College of Nursing, College of Optometry, College of Pharmacy, and College of Veterinary Medicine—to discuss the MA and Graduate Minor. The leaders from the health campus colleges and schools have all expressed agreement that a Graduate Minor in Bioethics would serve their graduate students well. Further conversations with leadership in the Colleges of Public Affairs, Law, Public Health, Social Work, the Department of Philosophy, and other “stakeholder” disciplines for bioethics have led to the same consensus that a Graduate Minor is a welcome addition for the University. -

David B. Fletcher CV Wheaton College (IL)
David B. Fletcher Associate Professor of Philosophy Wheaton College Wheaton, Illinois 60187 (630)752-5890, fax 752-5581 [email protected] EDUCATION Ph.D. Philosophy, University of Illinois at Urbana-Champaign, 1984 M.A. Philosophy, Loyola University of Chicago, 1980 B.A. Trinity College, Deerfield, Illinois, 1973 Wright College, City Colleges of Chicago, 1970-71 PROFESSIONAL/TEACHING EXPERIENCE Wheaton College, 1981-present Associate Professor (Assistant Professor, 1981-86; tenure awarded, 1988) Courses taught: Ethical Theory; Bioethics; Contemporary Moral Problems; Philosophy of Law; Introduction to Philosophy; Aesthetics; Asian Philosophy; Business Ethics; Social Philosophy; Social and Legal Philosophy; Global Justice; Ethics in Education, Marxism; Plato Seminar; Existentialism; Humanism; Internship; Independent Study Wheaton College, 1994-1997 Chair, Department of Philosophy Trinity Evangelical Divinity School, 1994- Visiting present Professor of Bioethics Graduate Courses taught: Bioethics Seminar, Advanced Institute in Bioethics, Introduction to Bioethics, Classic Cases in Bioethics, Ethical Theory Green College, University of Oxford, 1991 Visiting Scholar College of St. Francis, 1985-1995 Adjunct Professor, Health Arts Courses taught: Ethics and Morality, Philosophy and Modern Society, World Religions 2 University of Illinois, 1977-81 Graduate Teaching Assistant, Instructor Department of Philosophy Courses taught: Introduction to Philosophy, Introduction to Ethics, Logic Loyola University, 1975-76 Graduate Assistant Department of Philosophy Journal of the American Medical Association, 1974 Manuscript Editor THESES DIRECTED Co-directed a master’s thesis at the Command and General Staff College of the U. S. Army for Major Mitchell Payne, The Army Ethic, 2014. Co-directed a master’s thesis in bioethics at Trinity International University for Sarah Flashing, H. -

Sources of Human Embryonic Stem Cells and Ethics
Sources of human embryonic stem cells and ethics This text has been taken from the following article, Hug K. Sources of human embryos for stem cell research: ethical problems and their possible solutions. Medicina (Kaunas) 2005; 41 (12): 1002-10. The author has made some modifications in this web version of the text. This is an overview of ethical issues discussed specifically regarding human embryonic stem cell research before the derivation of human iPS cells. The use of human embryonic stem cells in research has raised a number of ethical controversies. The extent of these controversies is partly dependent on the source of embryonic stem cells (1). There are three main sources of human embryonic stem cells: 1. Already existing embryonic stem cell lines; 2. Embryos that are left unused after in vitro fertilization procedures (the so-called “spare” embryos); 3. Embryos created by means of somatic cell nuclear transfer technique (the same technique that was used when Dolly was created) for the purpose of conducting research. Deriving embryonic stem cells from already existing embryonic stem cell lines is a less controversial practice than deriving them from “spare” embryos left from in vitro fertilization procedures. Stem cells derived from embryos created for research by somatic cell nuclear transfer technique raise major ethical objections from certain parts of society, arguing from religious and other moral perspectives (1). However, many of those who oppose embryonic stem cell research generally agree that the first source of embryonic stem cells (already created embryonic stem cell lines) is an acceptable one. They base this opinion on the argument that stem cell lines have already been created and it is impossible to save the lives of former embryos from which they were created, even if harvesting of embryos itself may have been a morally wrong action.