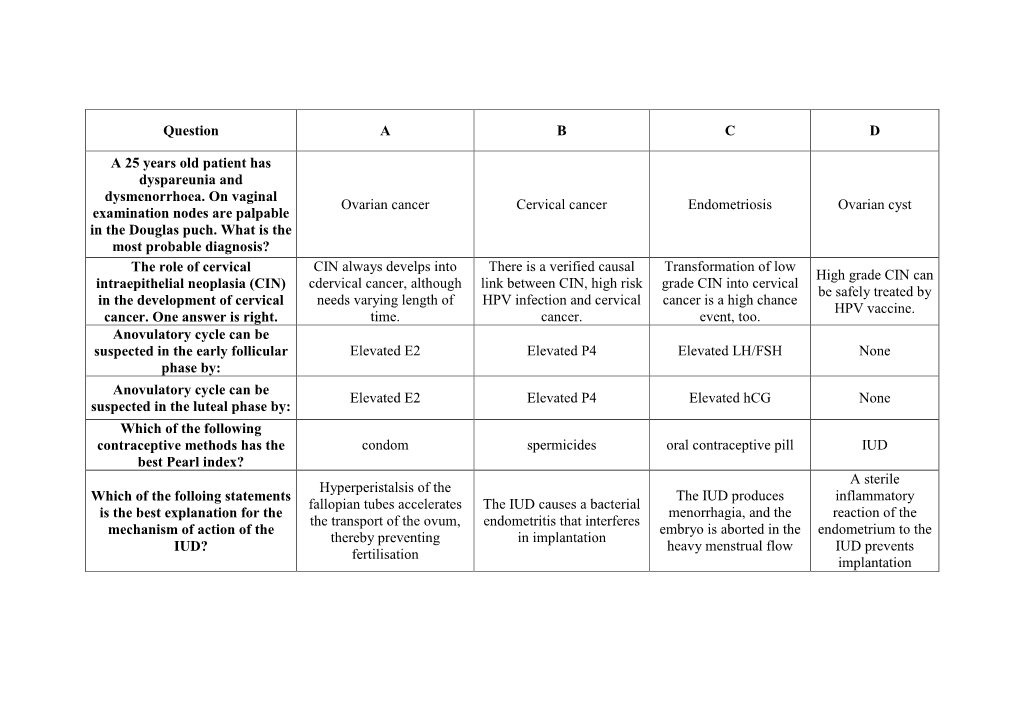
Question a B C D a 25 Years Old Patient Has Dyspareunia And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vaginitis and Abnormal Vaginal Bleeding
UCSF Family Medicine Board Review 2013 Vaginitis and Abnormal • There are no relevant financial relationships with any commercial Vaginal Bleeding interests to disclose Michael Policar, MD, MPH Professor of Ob, Gyn, and Repro Sciences UCSF School of Medicine [email protected] Vulvovaginal Symptoms: CDC 2010: Trichomoniasis Differential Diagnosis Screening and Testing Category Condition • Screening indications – Infections Vaginal trichomoniasis (VT) HIV positive women: annually – Bacterial vaginosis (BV) Consider if “at risk”: new/multiple sex partners, history of STI, inconsistent condom use, sex work, IDU Vulvovaginal candidiasis (VVC) • Newer assays Skin Conditions Fungal vulvitis (candida, tinea) – Rapid antigen test: sensitivity, specificity vs. wet mount Contact dermatitis (irritant, allergic) – Aptima TMA T. vaginalis Analyte Specific Reagent (ASR) Vulvar dermatoses (LS, LP, LSC) • Other testing situations – Vulvar intraepithelial neoplasia (VIN) Suspect trich but NaCl slide neg culture or newer assays – Psychogenic Physiologic, psychogenic Pap with trich confirm if low risk • Consider retesting 3 months after treatment Trichomoniasis: Laboratory Tests CDC 2010: Vaginal Trichomoniasis Treatment Test Sensitivity Specificity Cost Comment Aptima TMA +4 (98%) +3 (98%) $$$ NAAT (like GC/Ct) • Recommended regimen Culture +3 (83%) +4 (100%) $$$ Not in most labs – Metronidazole 2 grams PO single dose Point of care – Tinidazole 2 grams PO single dose •Affirm VP III +3 +4 $$$ DNA probe • Alternative regimen (preferred for HIV infected -

Successful Treatment of Genital Pruritus Using Topical Immunomodulators As a Single Therapy in Multi-Morbid Patients
Letters to the Editor 195 Successful Treatment of Genital Pruritus Using Topical Immunomodulators as a Single Therapy in Multi-morbid Patients Elke Weisshaar Clinical Social Medicine, Occupational and Environmental Dermatology, University Hospital Heidelberg, Thibautstrasse 3, DE-69115 Heidelberg, Germany. E-mail: [email protected] Accepted October 29, 2007. Sir, origin. He had been suffering from arterial hyperten- Anogenital pruritus is defined as pruritus affecting the skin sion, recurrent back pain and occasional heartburn. of the anus, perianal and genital area. In men it frequently Various topical treatments, including glucocortico- presents as scrotal pruritus and in females as vulval steroids and pimecrolimus 1% cream, did not relieve his pruritus. It may be caused by skin diseases (e.g. eczema, scrotal pruritus. Because of the history of encephalitis psoriasis, irritant or allergic contact dermatitis), infections he rejected any further diagnostic tests and systemic (e.g. candidiasis, parasitosis, lichen sclerosus, prema- treatments and requested symptomatic relief. The lignant or malignant conditions), as well as by systemic scrotum showed mild lichenifications. Topical tacro- diseases. Age, especially in female patients, determines limus 0.03% was started twice daily and the pruritus the initial most common differential diagnoses that need resolved completely within 2 weeks (VAS 0). After 6 to be considered (1). Acute genital pruritus is often caused weeks he continued to apply tacrolimus 0.03% twice a by infections, allergic or irritant contact dermatitis, leading week for a further period of 8 weeks. He has now been to prompt resolution after causal therapy. In a number of almost free of pruritus for one year and uses tacrolimus patients no underlying disease can be identified and the approximately 3 applications a week every 2 months condition is termed “pruritus of undetermined origin”. -

A Review on the Outcome of Patient Managed in One Stop Postmenopausal Bleeding Clinic in New Territories East Cluster, NTEC
A Review on the Outcome of Patient managed in One Stop Postmenopausal Bleeding Clinic in New Territories East Cluster, NTEC Principal Investigator: Dr. CHEUNG Chun Wai Co-investigators: Dr. FUNG Wen Ying, Linda Dr. CHAN Wai Yin, Winnie Prof. Lao Tzu Hsi, Terence Department of Obstetrics and Gynaecology, the Chinese University of Hong Kong, Shatin, New Territories, Hong Kong. Version: 1 Date: 24 Jul 2017 1 Introduction: Postmenopausal bleeding (PMB) is a common gynaecological complaint, accounting for up to 5 to 10 % of postmenopausal women being referred to gynaecological outpatient clinic (1, 2). It also comprised of up to 10% of our outpatient gynaecological referral. In general, 60 % of women with postmenopausal bleeding have no organic causes identified, whilst benign causes of PMB includes atrophic vaginitis, endometrial polyp, submucosal fibroid and functional endometrium. However, between 5.7 to 11.5% of women with postmenopausal bleeding have endometrial carcinoma (3, 4, 5), which is the fourth most common cancer among women (6), therefore, it is important to investigate carefully to exclude genital tract cancer. In the past, often women with PMB require multiple clinic visits in order to reach a final diagnosis. This not only increase the medical cost as a whole, but also imposes an enormous stress and burden on patients, concerning about delayed or overlooked diagnosis of genital tract cancer. A One-stop postmenopausal bleeding clinic has been established since February, 2002 by the Department of Obstetrics and Gynaecology, New Territories East cluster (NTEC) aiming at providing immediate assessment of women with postmenopausal bleeding in one single outpatient clinic assessment. -

INVESTIGATION and TREATMENT of VAGINAL DISCHARGE and PRURITUS VULVAE L Chan
INVITED ARTICLE I INVESTIGATION AND TREATMENT OF VAGINAL DISCHARGE AND PRURITUS VULVAE L Chan ABSTRACT The causes of vaginal discharge for pruritus vulvae in a patient are considered in three categories: common causes like vaginal candidosis, Trichomonal vaginitis, Gardnerella vaginitis; less common causes like gonococ- cal infection, Chlamydia infection and T-mycoplasma infection; and uncommon causes which include allergy to nylon underwear, human papilloma infection and eczema. The clinical features of each and a suggested treatment regime are given. Keywords: Vaginal discharge, Pruritus vulvae. SING MED J. 1989; NO 30: 471 - 472 INTRODUCTION atedly. Vaginal examination usually reveals white curdy discharge. Microscopy will show fungal spores or Vaginal discharge and pruritus vulvae are common hyphae. Treatment of the infection is with a course of symptoms that patients present with when they visit a antifungal vaginal tablets, e.g. Tioconazole (Gyno- gynaecologist. These symptoms suggest vaginal infec- Trosyd) 100 mgm o.n. for 3 nights. Anti -fungal cream tion, but as with all clinical problems, the diagnosis be given if there is pruritus vulvae. Oral Ketoconazole rests on a careful history, a thorough clinical examina- (Nizoral) one b.d. can be given for 5 days if there is tion and appropriate investigations. recurrent vaginal candidosis. Persistent chronic candi - The patient can complain of vaginal discharge, dosis. ìs due to lowered resistance to fungal infection. pruritus vulvae or both of these symptoms. Firstly, one Occasionally, the husband harbours a candida infection must determine whether the complaint is made so that between the prepuce and the glans penis and this the patient can legitimise seeing the doctor for the real infection needs -to be eradicated. -

Uterine Anomalies in Infertility - an Evaluation by Diagnostic Hysterolaparoscopy
Jebmh.com Original Research Article Uterine Anomalies in Infertility - An Evaluation by Diagnostic Hysterolaparoscopy Benudhar Pande1, Soumyashree Padhan2, Pranati Pradhan3 1, 2, 3 Department of Obstetrics and Gynaecology, Veer Surendra Sai Institute of Medical Science and Research, Burla, Odisha, India. ABSTRACT BACKGROUND About 10 - 15 % of reproductive age couples are affected by infertility.1 According Corresponding Author: Dr. Pranati Pradhan, to WHO 60 - 80 million couples currently suffer from infertility.2 Prevalence of Assistant Professor, infertility is rapidly increasing globally.3 Uterine factors of infertility include uterine Department of O & G, anomalies, fibroid uterus, synechiae, Asherman’s syndrome, and failure of VIMSAR, Burla – 768017, implantation without any known primary causes. Congenital uterine malformations Odisha, India. are seen in 10 % cases of infertile women. We wanted to evaluate the anomalies E-mail: [email protected] of uterus in case of primary and secondary infertility by DHL (diagnostic hysterolaperoscopy). DOI: 10.18410/jebmh/2020/580 METHODS How to Cite This Article: Pande B, Padhan S, Pradhan P. Uterine This is a hospital-based, observational study, conducted in the Department of anomalies in infertility-an evaluation by Obstetrics and Gynaecology, VIMSAR, Burla, from November 2017 to October diagnostic hysterolaparoscopy. J Evid 2019. Diagnostic hysterolaparoscopy was done in 100 infertility cases. Based Med Healthc 2020; 7(48), 2831- 2835. DOI: 10.18410/jebmh/2020/580 RESULTS In our study, uterine anomaly i.e. septate uterus was the most common Submission 03-09-2020, hysteroscopic abnormaly found in 23 cases followed by submucous fibroid, polyp, Peer Review 10-09-2020, Acceptance 17-10-2020, synechiae and bicornuate uterus. -

How to Evaluate Vaginal Bleeding and Discharge
How to Evaluate Vaginal Bleeding and Discharge Is the bleeding normal or abnormal? When does vaginal discharge reflect something as innocuous as irritation caused by a new soap? And when does it signal something more serious? The authors’ discussion of eight actual patient presentations will help you through the next differential diagnosis for a woman with vulvovaginal complaints. By Vincent Ball, MD, MAJ, USA, Diane Devita, MD, FACEP, LTC, USA, and Warren Johnson, MD, CPT, USA bnormal vaginal bleeding or discharge is typically due to either inadequate levels of estrogen one of the most common reasons women or a persistent corpus luteum. Structural causes of come to the emergency department.1,2 bleeding include leiomyomas, endometrial polyps, or Because the possible underlying causes malignancy. Infectious etiologies include pelvic in- Aare diverse, the patient’s age, key historical factors, flammatory disease (PID). Additionally, a variety of and a directed physical examination are instrumental bleeding dyscrasias involving platelet or clotting fac- in deciding on diagnosis and treatment. This article tors can complicate the normal menstrual period. Iat- will review some common case presentations of rogenic causes of vaginal bleeding include hormone nonpregnant female patients with abnormal vaginal replacement therapy, steroid hormone contraception, bleeding, inflammation, or discharge. and contraceptive intrauterine devices.3-5 Anovulatory bleeding is common in perimenar- ABNORMAL VAGINAL BLEEDING chal girls as a result of an immature hypothalamic- To ensure appropriate patient management, “Is she pituitary axis and in perimenopausal women due to pregnant?” should be the first question addressed, declining levels of estrogen. During reproductive since some vulvovaginal signs and symptoms will years, dysfunctional uterine differ in significance and urgency depending on the bleeding (DUB) is the most >>FAST TRACK<< answer. -

OBGYN-Study-Guide-1.Pdf
OBSTETRICS PREGNANCY Physiology of Pregnancy: • CO input increases 30-50% (max 20-24 weeks) (mostly due to increase in stroke volume) • SVR anD arterial bp Decreases (likely due to increase in progesterone) o decrease in systolic blood pressure of 5 to 10 mm Hg and in diastolic blood pressure of 10 to 15 mm Hg that nadirs at week 24. • Increase tiDal volume 30-40% and total lung capacity decrease by 5% due to diaphragm • IncreaseD reD blooD cell mass • GI: nausea – due to elevations in estrogen, progesterone, hCG (resolve by 14-16 weeks) • Stomach – prolonged gastric emptying times and decreased GE sphincter tone à reflux • Kidneys increase in size anD ureters dilate during pregnancy à increaseD pyelonephritis • GFR increases by 50% in early pregnancy anD is maintaineD, RAAS increases = increase alDosterone, but no increaseD soDium bc GFR is also increaseD • RBC volume increases by 20-30%, plasma volume increases by 50% à decreased crit (dilutional anemia) • Labor can cause WBC to rise over 20 million • Pregnancy = hypercoagulable state (increase in fibrinogen anD factors VII-X); clotting and bleeding times do not change • Pregnancy = hyperestrogenic state • hCG double 48 hours during early pregnancy and reach peak at 10-12 weeks, decline to reach stead stage after week 15 • placenta produces hCG which maintains corpus luteum in early pregnancy • corpus luteum produces progesterone which maintains enDometrium • increaseD prolactin during pregnancy • elevation in T3 and T4, slight Decrease in TSH early on, but overall euthyroiD state • linea nigra, perineum, anD face skin (melasma) changes • increase carpal tunnel (median nerve compression) • increased caloric need 300cal/day during pregnancy and 500 during breastfeeding • shoulD gain 20-30 lb • increaseD caloric requirements: protein, iron, folate, calcium, other vitamins anD minerals Testing: In a patient with irregular menstrual cycles or unknown date of last menstruation, the last Date of intercourse shoulD be useD as the marker for repeating a urine pregnancy test. -

Coexistence of Adenomyosis, Adenocarcinoma, Endometrial and Myometrial Lesions in Resected Uterine Specimens
MOLECULAR AND CLINICAL ONCOLOGY 9: 231-237, 2018 Coexistence of adenomyosis, adenocarcinoma, endometrial and myometrial lesions in resected uterine specimens SEZA TETİKKURT1, ELİF ÇELİK1, HAZAL TAŞ1, TUĞÇE CAY1, SELMAN IŞIK2 and ABDULLAH TANER USTA3 Departments of 1Pathology, and 2Obstetrics and Gynecology, Bağcılar Training and Research Hospital, University of Health Sciences, Istanbul 34200; 3Department of Obstetrics and Gynecology, Acıbadem University, Istanbul 34718, Turkey Received April 5, 2018; Accepted June 12, 2018 DOI: 10.3892/mco.2018.1660 Abstract. The present study was conducted to identify adenomyosis may be an important factor for the determination endometrial and myometrial lesions coexisting with adenomy- of prognosis. osis, and to evaluate the clinicopathological characteristics of endometrial adenocarcinomas associated with adenomyosis. Introduction A retrospective analysis of the resected uterine specimens of 319 patients with adenomyosis admitted between January 1, Adenomyosis is defined as the benign infiltration of the endo- 2014 and August 1, 2017 was performed. The endometrial and metrium into the myometrium, leading to a diffusely enlarged myometrial lesions coexisting with adenomyosis were evalu- uterus that microscopically exhibits ectopic, non-neoplastic ated. The clinicopathological prognostic factors, including endometrial glands and stroma, surrounded by hypertro- tumor grade, myometrial invasion, lymphovascular space phic and hyperplastic myometrium (1). During periods of involvement, lymph node invasion, pathological stage and regeneration, healing and re-epithelisation, the endometrium recurrence, were analysed. For data analysis, the Chi-squared may invade a predisposed myometrium or a traumatised test was used and a P-value of <0.05 was considered to indi- endometrial-myometrial interface. Hormonal, genetic and cate statistically significant differences. The mean age of the immunological factors may be implicated in this sequence of patients was 52.1 years. -

Pretest Obstetrics and Gynecology
Obstetrics and Gynecology PreTestTM Self-Assessment and Review Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the information contained herein with other sources. For example and in particular, readers are advised to check the prod- uct information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. Obstetrics and Gynecology PreTestTM Self-Assessment and Review Twelfth Edition Karen M. Schneider, MD Associate Professor Department of Obstetrics, Gynecology, and Reproductive Sciences University of Texas Houston Medical School Houston, Texas Stephen K. Patrick, MD Residency Program Director Obstetrics and Gynecology The Methodist Health System Dallas Dallas, Texas New York Chicago San Francisco Lisbon London Madrid Mexico City Milan New Delhi San Juan Seoul Singapore Sydney Toronto Copyright © 2009 by The McGraw-Hill Companies, Inc. -

An Endometrial Polyp on Ultrasound
EXPOSITION OF AN ENDOMETRIAL POLYP ON ULTRASOUND INTRODUCTION: CASE: An Endometrial Polyp (EP) is a mass situated within the endometrium, affecting A premenopausal woman, suffering from menorrhagia and pre-menopausal and post-menopausal women, specifically those treated with inter-menstrual bleeding (IMB) presented to her general tamoxifen1. It is estimated that 25% of women have an EP2, which are predomi- practitioner and was referred for a pelvic US in line with best nately benign overgrowths of endometrial cells, however a malignant risk exists practice5,7. The patient was in good health, with no further (1 - 3%)3,4. Malignancy risk, alongside symptoms such as menorrhagia and infer- complaints and a normal body mass index (BMI). No previous tility, categorises EP’s as a pathology that requires an early diagnosis to aid best cancer or EP history. No previous Tamoxifen use. Both trans- treatment. Ultrasound (US) is the first-choice modality for assessment of sus- abdominal (TAUS) and transvaginal (TVUS) scans were per- pected EP’s5, with large studies proving it highly sensitive6. formed, in keeping with NICE guidelines5. The GP had estab- lished normal Ca-125 levels. B-mode US revealed a 12 x 11mm EP within the distal seg- Transvaginal trans- ment of the endometrial cavity. This presented as a focal hy- verse view - polyp perechoic region within the endometrium, surrounded by with surrounding free fluid. Use of doppler US established internal vascularity trace of free fluid. via a feeder vessel. Normal appearances of the uterus, ova- ries and adnexa. SYMPTOMS: • Menorrhagia3 (see spotting) • Pain3 • IMB3 • Post-menopausal bleeding (PMB)3 • ‘Spotting’ - new research theorises spotting and bleeding originates from the rupturing of the fragile vascular network within the polyp9. -

Vaginitis and Sexually Transmitted Diseases
VAGINITIS AND SEXUALLY TRANSMITTED DISEASES Joel T. Katz, MD* Sexually transmitted diseases (STDs) are among the most in which R0 is the average number of secondary cases gener- common causes of infectious illness in the world. The Unite d ated by each primary infection in a population (i.e., the States leads industrialized nations in the occurrence of STDs, reproductive number), b is the average probability of trans- and after a slight trend downward in the 1990s, there has mission with each sexual partnership, c is the average been an upswing in STDs in the past decade, especially number of sexual partnerships formed per unit of time, and among teenagers. Currently, the annual rate of AIDS diag- D is the mean duration of infection.8 For diseases in which noses reported among males aged 15 to 19 years has nearly each case generates an average of one additional case, R0 doubled in the past 10 years, and rates for gonorrhea and equals 1 and the prevalence remains stable; values less than syphilis have also risen in this population.1 In many deve l- 1 and greater than 1 are associated with a declining or rising oping nations, STDs (excluding HIV infection) are the prevalence, respectively. second greatest cause of disability-adjusted years of life Although each of the terms in this equation is complex, lost,2 and highly prevalent bacterial and viral STDs may the simplification that the equation offers can explain a great facilitate HIV transmission.3 deal about the distribution of different STDs in a population Of the more than 30 sexually transmitted pathogens and provides a framework for conceptualizing STD epide- that are currently recognized, eight have been identified miology. -

Laboratory Diagnosis of Sexually Transmitted Infections, Including Human Immunodeficiency Virus
Laboratory diagnosis of sexually transmitted infections, including human immunodeficiency virus human immunodeficiency including Laboratory transmitted infections, diagnosis of sexually Laboratory diagnosis of sexually transmitted infections, including human immunodeficiency virus Editor-in-Chief Magnus Unemo Editors Ronald Ballard, Catherine Ison, David Lewis, Francis Ndowa, Rosanna Peeling For more information, please contact: Department of Reproductive Health and Research World Health Organization Avenue Appia 20, CH-1211 Geneva 27, Switzerland ISBN 978 92 4 150584 0 Fax: +41 22 791 4171 E-mail: [email protected] www.who.int/reproductivehealth 7892419 505840 WHO_STI-HIV_lab_manual_cover_final_spread_revised.indd 1 02/07/2013 14:45 Laboratory diagnosis of sexually transmitted infections, including human immunodeficiency virus Editor-in-Chief Magnus Unemo Editors Ronald Ballard Catherine Ison David Lewis Francis Ndowa Rosanna Peeling WHO Library Cataloguing-in-Publication Data Laboratory diagnosis of sexually transmitted infections, including human immunodeficiency virus / edited by Magnus Unemo … [et al]. 1.Sexually transmitted diseases – diagnosis. 2.HIV infections – diagnosis. 3.Diagnostic techniques and procedures. 4.Laboratories. I.Unemo, Magnus. II.Ballard, Ronald. III.Ison, Catherine. IV.Lewis, David. V.Ndowa, Francis. VI.Peeling, Rosanna. VII.World Health Organization. ISBN 978 92 4 150584 0 (NLM classification: WC 503.1) © World Health Organization 2013 All rights reserved. Publications of the World Health Organization are available on the WHO web site (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for non-commercial distribution – should be addressed to WHO Press through the WHO web site (www.who.int/about/licensing/copyright_form/en/index.html).