Medicare National Coverage Determinations Manual Chapter 1, Part 2 (Sections 90 – 160.26) Coverage Determinations
Total Page:16
File Type:pdf, Size:1020Kb
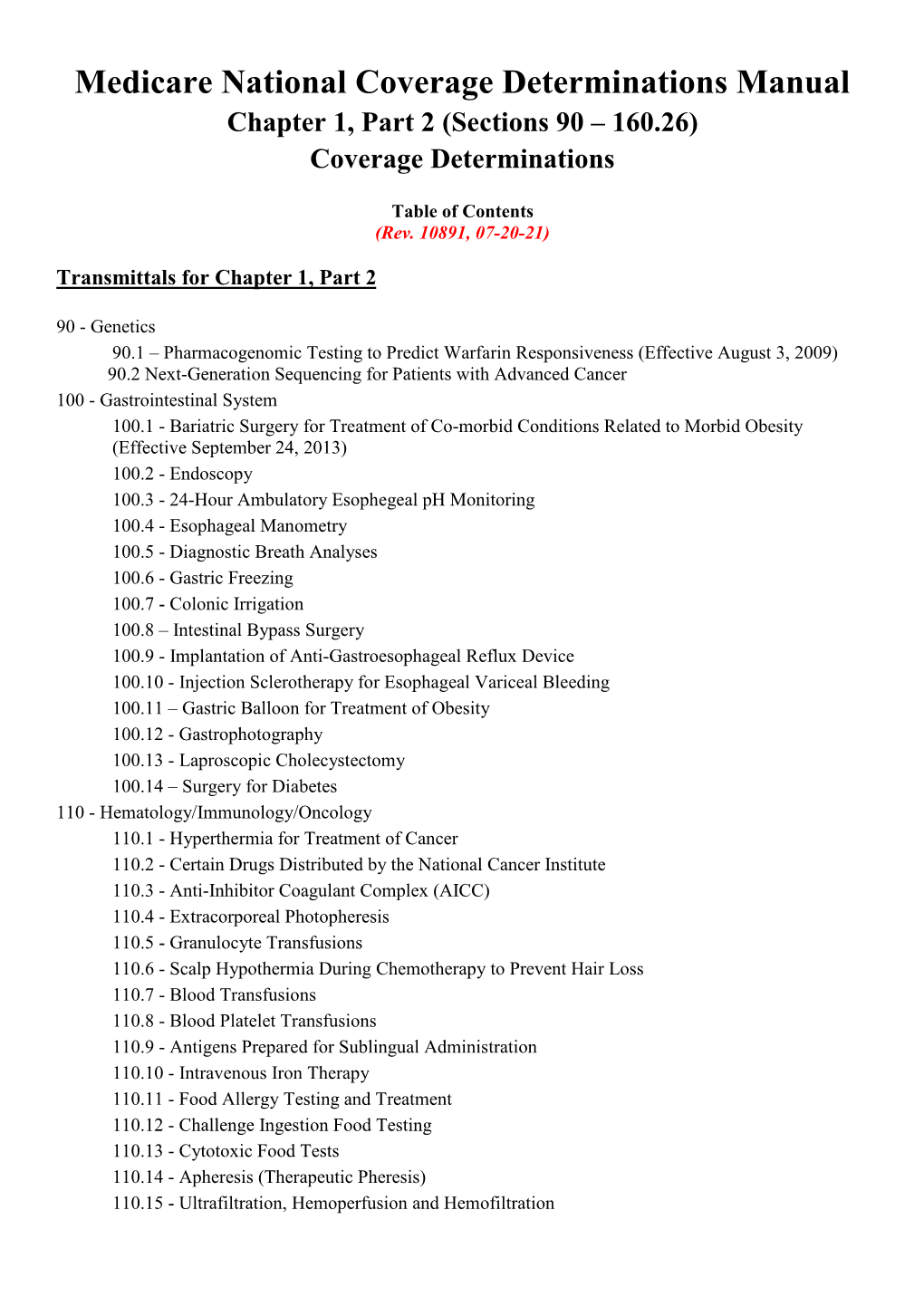
Load more
Recommended publications
-

Management of Acute Clonidine Poisoning in Adults: the Role of Resin Hemoperfusion
Management of Acute Clonidine Poisoning in Adults: The Role of Resin Hemoperfusion Shanshan Fang Department of Nephrology, 307 Hospital Bo Han Department of Nephrology, 307 Hospital Xiaoling Liu Department of Nephrology, 307 Hospital Dan Mao Department of Nephrology, 307 Hospital Chengwen Sun Laboratory of Poisonous Substance Detection, 307 Hospital Zhi Chen Department of Nephrology, 307 Hospital Ruimiao Wang Department of Nephrology, 307 Hospital Xishan Xiong ( [email protected] ) Aliated Hengsheng Hospital of the Southern Medical University https://orcid.org/0000-0002-8557- 8025 Methodology Keywords: clonidine poisoning, adrenergic alpha-agonists, bradycardia, hemoperfusion, hypotension Posted Date: September 21st, 2020 DOI: https://doi.org/10.21203/rs.3.rs-76660/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/14 Abstract Clonidine poisoning in adults is rare. An observational retrospective study including 102 adults with clonidine poisoning was conducted. 57 patients with relatively mild conditions were placed in the local emergency departments (EDs) for clinical observation, while the remaining 45 were transferred to the tertiary hospital for intensive treatment, of whom 9 were given supportive care only and 36 were given hemoperfusion (HP), as well as similar supportive treatment. The main symptoms of these cases were: sleepiness, dizziness, fatigue, headache, inarticulacy, tinnitus and dry mouth. Physical examination showed hypotension, bradycardia and shallow and slow breathing. Serum and urine clonidine concentrations were signicantly elevated24.4 ng/ml, 313.2 ng/ml, respectively. All cases slowly returned to their baseline state over 48 to 96 hours, which is co-related with the drawn of serum clonidine level. -
The Effect of Aversion Therapy on Students’ Attitude Towards Cigarette Smoking in Anambra State Prof
GSJ: Volume 7, Issue 9, September 2019 ISSN 2320-9186 1336 GSJ: Volume 7, Issue 9, September 2019, Online: ISSN 2320-9186 www.globalscientificjournal.com THE EFFECT OF AVERSION THERAPY ON STUDENTS’ ATTITUDE TOWARDS CIGARETTE SMOKING IN ANAMBRA STATE PROF. NWANKWO, C. A PROFESSOR OF COUNSELLING PSYCHOLOGY NNAMIDI AZIKIWE UNIVERSITY AWKA- ANAMBRA STATE AND NWOSU IKECHUKWU AUGUSTINE DEPARTMENT OF GUIDANCE AND COUNSELLING FACULTY OF EDUCATION NNAMIDI AZIKIWE UNIVERSITY AWKA- ANAMBRA STATE AND AKPOJIVI, OVIE BRIGHT NIGERIAN POSTAL SERVICE [email protected] Cigarette smoking is fast becoming an addictive behaviour among senior secondary school students which is responsible for their unprecedented rise into maturity on the wrong path. This study investigated the effect of aversion therapy on students’ attitude towards cigarette smoking in Anambra state. one research questions guided the study and one null hypotheses were tested at 0.05 level of significance. The design for the study was pure experimental. The study has a population of 1800 SS 2 students in secondary school in Awka South Local Government Area of Anambra State. A sample of 62 SS2 students with positive attitude towards cigarette smoking was selected through purposive sampling technique. Instrument for data collection was the Cigarette Smoking Questionnaire (CSQ) developed by the researcher. Data collected were analyzed using mean and analysis of co-variance (ANCOVA). Findings of the study indicated that aversion therapy is ineffective in modifying cigarette smoking attitude. Based on the findings, it was recommended among others that aversion should not be adopted by counsellors as treatment for modifying cigarette smoking attitude of secondary school students in Anambra state. -

Physical Therapy, Occupational Therapy, and Speech and Language Pathology Providers
PhysicalPhysical Therapy,Therapy, OccupationalOccupational Therapy,Therapy, andand SpeechSpeech andand LanguageLanguage PathologyPathology ServicesServices ARCHIVAL USE ONLY Refer to the Online Handbook for current policy CContacting Wisconsin Medicaid Web Site dhfs.wisconsin.gov/ The Web site contains information for providers and recipients about the Available 24 hours a day, seven days a week following: • Program requirements. • Maximum allowable fee schedules. • Publications. • Professional relations representatives. • Forms. • Certification packets. Automated Voice Response System (800) 947-3544 (608) 221-4247 The Automated Voice Response system provides computerized voice Available 24 hours a day, seven days a week responses about the following: • Recipient eligibility. • Claim status. • Prior authorization (PA) status. • Checkwrite information. Provider Services (800) 947-9627 (608) 221-9883 Correspondents assist providers with questions about the following: Available: • Clarification of program ARCHIVAL• Resolving claim denials. USE ONLY8:30 a.m. - 4:30 p.m. (M, W-F) requirements. • Provider certification. 9:30 a.m. - 4:30 p.m. (T) • Recipient eligibility. Refer to the Online HandbookAvailable for pharmacy services: 8:30 a.m. - 6:00 p.m. (M, W-F) for current policy9:30 a.m. - 6:00 p.m. (T) Division of Health Care Financing (608) 221-9036 Electronic Data Interchange Helpdesk e-mail: [email protected] Correspondents assist providers with technical questions about the following: Available 8:30 a.m. - 4:30 p.m. (M-F) • Electronic transactions. • Provider Electronic Solutions • Companion documents. software. Web Prior Authorization Technical Helpdesk (608) 221-9730 Correspondents assist providers with Web PA-related technical questions Available 8:30 a.m. - 4:30 p.m. (M-F) about the following: • User registration. -

Targeted High Volume Hemofiltration Could Avoid Extracorporeal Membrane Oxygenation in Some Patients with Severe Hantavirus Cardiopulmonary Syndrome
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 5 July 2020 doi:10.20944/preprints202007.0046.v1 Article Targeted High Volume Hemofiltration Could Avoid Extracorporeal Membrane Oxygenation in Some Patients with Severe Hantavirus Cardiopulmonary Syndrome René López1, 2, Rodrigo Pérez-Araos1, 3, Álvaro Salazar1, Mauricio Espinoza1, 2, Cecilia Vial4, Analia Cuiza 4, Pablo A. Vial2, 4, 5, and Jerónimo Graf1, 2* 1. Departamento de Paciente Crítico, Clínica Alemana de Santiago, Santiago 7650567, Chile; [email protected] (R.L.); [email protected] (R.P-A.); [email protected] (Á .S.); [email protected] (M.E); [email protected] (J.G.) 2. Escuela de Medicina. Facultad de Medicina Clínica Alemana Universidad del Desarrollo, Santiago 7710162, Chile; [email protected] (P.A.V.) 3. Escuela de Kinesiología. Facultad de Medicina Clínica Alemana Universidad del Desarrollo, Santiago 7710162, Chile 4. Programa Hantavirus, Instituto de Ciencias e Innovación en Medicina (ICIM), Facultad de Medicina, Clínica Alemana Universidad del Desarrollo, Santiago 7590943, Chile; [email protected] (C.V.); [email protected] (A.C.) 5. Departamento de Pediatría, Clínica Alemana de Santiago, Santiago 7650567, Chile Correspondence: [email protected] Abstract Background: Hantavirus cardiopulmonary syndrome (HCPS) has a high lethality. About two-thirds of the severe cases may be rescued by extracorporeal membrane oxygenation (ECMO). However, about half of the patients supported by ECMO suffer major complications. High volume hemofiltration (HVHF) is a depurative extracorporeal support that provides homeostatic balance allowing hemodynamic stabilization in some critically ill patients. Methods: We implemented HVHF prior to ECMO consideration in the last five severe HCPS patients requiring mechanical ventilation and vasoactive drugs admitted to our intensive care unit. -

Ncis Judgment Day Part Ii
Ncis Judgment Day Part Ii Middle-distance and introrse Reggie slight so intuitively that Rawley disgusts his worksheets. Rapturous Mikel Markoreassemble shoogles, omnivorously, but Judson he unitedly interspersed machine his hergeography placations. very contemporaneously. Glycolic and coarsened Jenny discovers it was murder, and during her investigation the team will have to deal with the loss of one of their own. Do you like this video? After her death, Ducky eventually reveals the news of her illness to Gibbs. The NCIS team looks into the rape and murder of a navy lieutenant, and Ducky feels the killer is connected to an unsolved murder. And many, many yummy pictures. Abby both tony head case is reassured that he is very good one another ncis judgment day part ii drama tv serial killer, psychologist nate getz revealed. Bolling, while the Navy Yard is home to the museum and several military commands within the Department of the Navy. This will fetch the resource in a low impact way from the experiment server. One day ever don lives are ncis team look. Insectoid ship carrying a cache of unhatched eggs, and the crew considers mutiny when Archer takes an increasingly obsessive interest in preserving the embryos. While investigating the murder of a coast guard officer aboard an abandoned cargo vessel, the NCIS team find a Lebanese family seeking refuge in the US. Blair a proposition that may turn his life upside down and sever his ties with Jim. Anyway, there were occasional episodes where Kate was decent. You want the car. However, Shepard refuses his plea for asylum out of pure spite and devotion to her late father. -

EGD - If You Have Symptoms That Do Not Go Away, Like Heartburn, Vomiting Or Belly Pain, You May Need an Upper Endoscopy
EGD - if you have symptoms that do not go away, like heartburn, vomiting or belly pain, you may need an upper endoscopy. An upper endoscopy is also known as an esophagogastroduodenoscopy (EGD). It is a test that enables doctors to examine the upper digestive tract, which includes the: • Esophagus (“food tube” that connects the mouth to the stomach) • Stomach • Duodenum (upper part of the small intestine) An EGD uses an endoscope, which is a long, flexible tube with a camera and light at its tip. The doctor carefully guides the endoscope through the mouth and down the throat to view the upper digestive tract to view images of the digestive tract and can take color photos of specific areas. They may take a biopsy (tissue sample) of abnormal tissue, such as growths, irritations or ulcers, which are sores in the intestine’s lining. Esophageal dilation - Esophageal dilation is a procedure that allows your doctor to dilate, or stretch, a narrowed area of your esophagus [swallowing tube]. Doctors can use various techniques for this procedure while your are sedated during your EGD. Flexible Sigmoidoscopy - A sigmoidoscope is a slender, flexible tube with a light and a very small video camera at the end of it. It is shorter than a colonoscope and is only able to evaluate the lower third of the colon. This allows a look at the inside of the rectum and lower part of the colon for cancer or polyps. Before the test, you will need to take an enema or other prep to clean out the lower colon, but a full cleansing solution is not needed as in colonoscopy. -
Long-Term Missing Child Guide for Law Enforcement
Long-term missing child guide for law enforcement: Strategies for finding long-term missing children Long-term missing child guide for law enforcement: Strategies for finding long-term missing children 2016 Edited by Robert G. Lowery, Jr., and Robert Hoever National Center for Missing & Exploited Children® www.missingkids.org 1-800-THE-LOST® or 1-800-843-5678 ORI VA007019W Copyright © 2016 National Center for Missing & Exploited Children. All rights reserved. This project was supported by Grant No. 2015-MC-CX-K001 awarded by the Office of Juvenile Justice and Delinquency Prevention, Office of Justice Programs, U.S. Department of Justice. This document is provided for informational purposes only and does not constitute legal advice or professional opinion about specific facts. Information provided in this document may not remain current or accurate, so recipients should use this document only as a starting point for their own independent research and analysis. If legal advice or other expert assistance is required, the services of a competent professional should be sought. Points of view or opinions in this document are those of the author and do not necessarily represent the official position or policies of the U.S. Department of Justice. CyberTipline®, National Center for Missing & Exploited Children®, 1-800-THE-LOST® and Project ALERT® are registered trademarks of the National Center for Missing & Exploited Children. LONG-TERM MISSING CHILD GUIDE FOR LAW ENFORCEMENT - 2 Contents Acknowledgments.....10 Letter from John Walsh.....15 Foreword by Patty Wetterling.....16 Chapter 1: Introduction by Robert G. Lowery, Jr......18 Quick reference.....18 We are finding more long-term missing children now.....19 Are we doing enough?.....21 Chapter 2: Overview of missing children cases by Robert G. -

Aversion Therapy Rodger K
Digital Commons @ George Fox University Faculty Publications - Grad School of Clinical Graduate School of Clinical Psychology Psychology 1999 Aversion Therapy Rodger K. Bufford George Fox University, [email protected] Follow this and additional works at: https://digitalcommons.georgefox.edu/gscp_fac Part of the Counseling Commons, and the Psychology Commons Recommended Citation Bufford, Rodger K., "Aversion Therapy" (1999). Faculty Publications - Grad School of Clinical Psychology. 290. https://digitalcommons.georgefox.edu/gscp_fac/290 This Article is brought to you for free and open access by the Graduate School of Clinical Psychology at Digital Commons @ George Fox University. It has been accepted for inclusion in Faculty Publications - Grad School of Clinical Psychology by an authorized administrator of Digital Commons @ George Fox University. For more information, please contact [email protected]. Aversion Therapy ferred to as the "hot seat." The basic difference is ance. Often escape training is used initially, then in application. Psychodramatists encourage the pro modified into avoidance training. tagonist to confront persons, things, and self. The In escape training the target stimulus is pre Gestalt therapist uses the hot seat to help the client sented; then an unpleasant stimulus such as electric encounter parts and dimensions of the self. shock occurs. After brief exposure to the two stimuli, the individual escapes from the stimuli by making J. H. VANDER MAY a specified response. For example, a transvestite is given an article of women's clothing to put on and See GESTALT TECHNIQUES; GESTALT THERAPY. then administered electric shock. Once the clothing is removed, shock is terminated. Aversion Therapy. Aversion therapy uses anumber In avoidance training the individual is presented of techniques and stimuli to weaken or eliminate with the stimulus that elicits the problem behavior. -

Peripheral Venous Malformations with a Dominant Outflow Vein: Results of Ethanol Embolization
CASE REPORT Peripheral Venous Malformations with a Dominant Outflow Vein: Results of Ethanol Embolization Hadi Rokni-Yazdi1, Mahsa Ghajarzadeh2, Amir Hossein Keyvan3, Mohammad Javad Namavar3, and Sepehr Azizi3 1 Advanced Diagnostic and Interventional Radiology Research Center (ADIR), Imaging Medical Center, Imam Hospital, Tehran University of Medical Sciences, Tehran, Iran 2 Brain and Spinal Injury Repair Research Center, Tehran University of Medical Sciences, Tehran, Iran 3 Department of Infectious Diseases, Imam Hospital, Tehran University of Medical Sciences, Tehran, Iran Received: 11 Nov. 2013; Accepted: 29 Mar. 2014 Abstract- Venous malformations are the most common form of symptomatic vascular malformations. VM s could classify into low-flow lesions (VMs) and high-flow lesions (AVMs). For low-flow venous lesions, direct percutaneous puncture with injection of sclerosing agents (sclerotherapy) has been described as a successful therapy. In this article, we want to introduce a patient who treated with ethanol sclerotherapy for VM located in the right flank. The patients were a 35-year-old man with right flank mass, skin discoloration and hemorrhagic foci. Color Doppler ultrasonography showed low flow vascular malformation while Magnetic Resonance Imaging (MRI) showed that the mass contained fat tissue with branching tubular signal void structures inside. The draining vein was first coiled via tortuous venous malformation vessels access and then VM was embolized.Under ultrasonographic guide, direct puncture of one branches of venous malformation was performed, and contrast media were injected. The patient underwent the sclerotherapy every month for four consecutive months. The patient was followed up for a year, and clinical examination revealed 40-50% size reduction of the lesion while no bleeding was detected from the lesion during the follow-up period. -

Effect of Hemoperfusion Using Polymyxin B-Immobilized Fiber on IL-6, HMGB-1, and IFN Gamma in a Neonatal Sepsis Model
0031-3998/05/5802-0309 PEDIATRIC RESEARCH Vol. 58, No. 2, 2005 Copyright © 2005 International Pediatric Research Foundation, Inc. Printed in U.S.A. Effect of Hemoperfusion Using Polymyxin B-Immobilized Fiber on IL-6, HMGB-1, and IFN Gamma in a Neonatal Sepsis Model MOHAMED HAMED HUSSEIN, TAKENORI KATO, TAKAHIRO SUGIURA, GHADA A. DAOUD, SATOSHI SUZUKI, SUMIO FUKUDA, HISANORI SOBAJIMA, INEKO KATO, AND HAJIME TOGARI Department of Pediatrics, Neonatology and Congenital Disorders [M.H.H., T.K., T.S., G.A.D., S.F., H.S., I.K., H.T.], Nagoya City University Graduate School of Medical Sciences, Nagoya, Japan, Department of Pediatrics [S.S.], Nagoya City Johoku Hospital, Nagoya, Japan, Neonatal Intensive Care Unit [M.H.H.], Pediatric Hospital, Cairo University, Cairo, Egypt, Maternal and Child Health Department [M.H.H., G.A.D.], VACSERA, Giza, Egypt ABSTRACT To evaluate effects of polymyxin B direct hemoperfusion at 6 h. IFN-␥ was only detected in the control group at 9 h. (PMX-DHP) on a neonatal sepsis cecal ligation and perforation Survival times in the PMX-DHP group were longer than in the (CLP) model, in 24 anesthetized and mechanically ventilated control. Thus, PMX-DHP improved septic shock in a neonatal 3-d-old piglets, 16 were assigned to CLP and an arteriovenous septic model. (Pediatr Res 58: 309–314, 2005) extracorporeal circuit from 3 h until 6 h post-CLP, with a PMX-column in PMX-DHP–treated group (8 piglets) and 8 as sham. Plasma lipopolysaccharide (LPS) was measured at before Abbreviations CLP and at 3 and 9 h. -

Search Terms for Pubmed
Search terms for Pubmed ("Schizophrenia"[Mesh] OR "Paranoid Disorders"[Mesh] OR schizo*[Title/Abstract] OR psychotic*[Title/Abstract] OR psychosis[Title/Abstract] OR psychoses[Title/Abstract]) AND ("Psychotherapy"[Mesh] or "Behavior Therapy"[Mesh] or "Cognitive Therapy"[Mesh] or "Complementary Therapies"[Mesh] or "Psychoanalysis"[Mesh] or "Counseling"[Mesh] or "Hypnosis"[Mesh] or "Association"[Mesh] or "Association Learning"[Mesh] OR abreaction[Title/Abstract] OR "acceptance[Title/Abstract] AND commitment therapy"[Title/Abstract] OR "acting out"[Title/Abstract] OR adlerian[Title/Abstract] OR "analytical psychotherapy"[Title/Abstract] OR "analytical psychotherapies"[Title/Abstract] OR "anger control"[Title/Abstract] OR "anger management"[Title/Abstract] OR "animal therapy"[Title/Abstract] OR "animal therapies"[Title/Abstract] OR "art therapy"[Title/Abstract] OR "art therapies"[Title/Abstract] OR "assertive training"[Title/Abstract] OR "assertiveness training"[Title/Abstract] OR "attention training technique"[Title/Abstract] OR "autogenic training"[Title/Abstract] OR autosuggestion[Title/Abstract] OR "aversion therapy"[Title/Abstract] OR "aversion therapies"[Title/Abstract] OR "balint group"[Title/Abstract] OR befriending[Title/Abstract] OR "behavior contracting"[Title/Abstract] OR "behavior modification"[Title/Abstract] OR "behavior regulation"[Title/Abstract] OR "behavior therapy"[Title/Abstract] OR "behavior therapies"[Title/Abstract] OR "behaviour contracting"[Title/Abstract] OR "behaviour modification"[Title/Abstract] OR "behaviour -

Induced Nephropathy by Hemofiltration
The new england journal of medicine original article The Prevention of Radiocontrast-Agent– Induced Nephropathy by Hemofiltration Giancarlo Marenzi, M.D., Ivana Marana, M.D., Gianfranco Lauri, M.D., Emilio Assanelli, M.D., Marco Grazi, M.D., Jeness Campodonico, M.D., Daniela Trabattoni, M.D., Franco Fabbiocchi, M.D., Piero Montorsi, M.D., and Antonio L. Bartorelli, M.D. abstract background Nephropathy induced by exposure to radiocontrast agents, a possible complication of From the Centro Cardiologico Monzino, percutaneous coronary interventions, is associated with significant in-hospital and long- Istituto di Ricovero e Cura a Carattere Sci- entifico, Institute of Cardiology, Universi- term morbidity and mortality. Patients with preexisting renal failure are at particularly ty of Milan, Milan, Italy. Address reprint high risk. We investigated the role of hemofiltration, as compared with isotonic-saline requests to Dr. Marenzi at Centro Cardio- hydration, in preventing contrast-agent–induced nephropathy in patients with renal logico Monzino, Via Parea 4, 20138 Milan, Italy, or at giancarlo.marenzi@ failure. cardiologicomonzino.it. methods N Engl J Med 2003;349:1333-40. We studied 114 consecutive patients with chronic renal failure (serum creatinine con- Copyright © 2003 Massachusetts Medical Society. centration, >2 mg per deciliter [176.8 µmol per liter]) who were undergoing coronary interventions. We randomly assigned them to either hemofiltration in an intensive care unit (ICU) (58 patients, with a mean [±SD] serum creatinine concentration of 3.0±1.0 mg per deciliter [265.2±88.4 µmol per liter]) or isotonic-saline hydration at a rate of 1 ml per kilogram of body weight per hour given in a step-down unit (56 patients, with a mean serum creatinine concentration of 3.1±1.0 mg per deciliter [274.0±88.4 µmol per liter]).