Can Residents Perform Transrectal Ultrasound-Guided Prostate Biopsy with Patient Comfort Comparable to Biopsy Performed by Attending Staff Urologists?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Is There Anything New in Prostate Cancer Screening?
IS THERE ANYTHING NEW IN PROSTATE CANCER SCREENING? ANDREW M.D. WOLF, MD, FACP ASSOCIATE PROFESSOR OF MEDICINE UNIVERSITY OF VIRGINIA SCHOOL OF MEDICINE No financial disclosures Case Presentation 62 yo white man without significant past medical history presents for annual preventive visit. He has no family history of prostate cancer. He has mild urinary hesitancy and his prostate is mildly enlarged without induration or nodules. His PSA has been gradually rising: - 2011: 2.35 - 2013: 2.17 - 2017: 3.75 - 2019: 4.51 Where do we go from here? What’s New in Prostate Cancer Screening? Key Questions • Do we have any new evidence for or against screening? • Do we have anything better than the PSA? • What about the good old digital rectal exam? • Are we doing any better identifying who needs to be treated? • What do the experts recommend? Prostate Cancer Incidence & Mortality Over the Decades Source: Seer 9 areas & US Mortality Files (National Center for Health Statistics, CDC, Feb 2018 CA Cancer J Clin 2019;69:7-34. Do we have any new evidence for or against prostate cancer screening? Is Prostate Screening Still Controversial? ERSPC Results • Prostate cancer death rate 27% lower in screened group (p = 0.0001) at 13 yrs • Number needed to screen to save 1 life: 781 • NNS to prevent 1 case of metastatic cancer: ~350 • Number needed to diagnose to save 1 life: 27 • Major issue of over-diagnosis & over-treatment Schroder FH, et al. Lancet 2014;384: 2027–2035 • Controlled for differences in study design • Adjusted for lead-time • Both studies led to a ~ 25-32% reduction in prostate cancer mortality with screening compared with no screening Ann Intern Med 2017;167:449-455 • 415,000 British men 50-69 randomized to a single offer to screen vs usual care (info sheet on request) • One-time screen & then followed for 10 yrs • Men dx’d with prostate cancer randomized to treatment vs active surveillance JAMA 2018;319(9):883-895. -

Profiling Prostate Cancer Therapeutic Resistance
International Journal of Molecular Sciences Review Profiling Prostate Cancer Therapeutic Resistance Cameron A. Wade 1 and Natasha Kyprianou 1,2,3,* 1 Departments of Urology, University of Kentucky College of Medicine, Lexington, Kentucky, KY 40536, USA; [email protected] 2 Department of Molecular and Cellular Biochemistry, University of Kentucky College of Medicine, Lexington, Kentucky, KY 40536, USA 3 Department of Toxicology & Cancer Biology, University of Kentucky College of Medicine, Lexington, Kentucky, KY 40536, USA * Correspondence: [email protected]; Tel.: +1-859-323-9812; Fax: +1-859-323-1944 Received: 1 March 2018; Accepted: 16 March 2018; Published: 19 March 2018 Abstract: The major challenge in the treatment of patients with advanced lethal prostate cancer is therapeutic resistance to androgen-deprivation therapy (ADT) and chemotherapy. Overriding this resistance requires understanding of the driving mechanisms of the tumor microenvironment, not just the androgen receptor (AR)-signaling cascade, that facilitate therapeutic resistance in order to identify new drug targets. The tumor microenvironment enables key signaling pathways promoting cancer cell survival and invasion via resistance to anoikis. In particular, the process of epithelial-mesenchymal-transition (EMT), directed by transforming growth factor-β (TGF-β), confers stem cell properties and acquisition of a migratory and invasive phenotype via resistance to anoikis. Our lead agent DZ-50 may have a potentially high efficacy in advanced metastatic castration resistant prostate cancer (mCRPC) by eliciting an anoikis-driven therapeutic response. The plasticity of differentiated prostate tumor gland epithelium allows cells to de-differentiate into mesenchymal cells via EMT and re-differentiate via reversal to mesenchymal epithelial transition (MET) during tumor progression. -

Neuroendocrine Differentiation of Prostatic Adenocarcinoma
J Lab Med 2019; 43(2): 123–126 Laboratory Case Report Cátia Iracema Morais*, João Lobo, João P. Barreto, Cláudia Lobo and Nuno D. Gonçalves Neuroendocrine differentiation of prostatic adenocarcinoma – an important cause for castration-resistant disease recurrence https://doi.org/10.1515/labmed-2018-0190 awareness of this entity is crucial due to its underdiagno- Received December 3, 2018; accepted December 12, 2018; previously sis and adverse prognosis. published online February 15, 2019 Keywords: carcinoma; castration-resistant (D064129); cell Abstract transformation; neoplastic (D002471); neuroendocrine (D018278); prostate (D011467); prostatic neoplasms. Background: Neuroendocrine differentiation of prostatic carcinoma is a rare entity associated with metastatic castration-resistant disease. Among useful biomarkers of neuroendocrine differentiation, chromogranin A, sero- Introduction tonin, synaptophysin and neuron-specific enolase stand out, while total prostate-specific antigen (PSA) levels are Neuroendocrine prostatic carcinoma is a rare and often low or undetectable. underdiagnosed histologic subtype. Despite the low Case presentation: We report a case of prostatic adenocar- incidence rate of primary neuroendocrine prostatic cinoma recurrence after a 6-year disease-free follow-up, in carcinoma (which represents under 1% of all prostate which increased serum chromogranin A levels and unde- cancers at diagnosis), 30–40% of patients who develop tectable total PSA provided a prompt indication of neu- metastasized castration-resistant -

Review Committee News—Urology
Review Committee News—Urology • Definitions of Board Pass Rates This is a reminder that programs will be cited for poor performance on the American Board of Urology examination if they average more than two standard deviations above the mean in failure rates over a five-year period. The RRC will only look at first-time test takers on Part One of the Board’s Qualifying Examination. The application of this standard began with programs reviewed after July 1, 2010. • Logging Ultrasound Procedures To define the current resident experience in performing urologic ultrasound procedures and to track this experience over time, the Urology Review Committee would like residents to log these cases starting July 1, 2012. Ultrasound cases include commonly performed procedures such as transrectal ultrasound (TRUS) with prostate biopsy, and non-TRUS biopsy procedures such as renal, pelvic, scrotal and penile ultrasound cases. The Review Committee is particularly interested in tracking resident involvement in non-TRUS biopsy ultrasound procedures. While TRUS-prostate biopsy will remain an index case with a minimum number required (25), there will be no minimum number of cases required for non- prostate ultrasound procedures. We ask that residents use one of the following CPT codes when logging these procedures: Category CPT code Scrotal 76870 Renal Retroperitoneal, limited (kidney only) 76775 Retroperitoneal, complete (both kidney and bladder) 76770 Transplant kidney ultrasound 76776 US guidance, intraoperative (e.g. during partial nephrectomy) 76998 US -

Clinical Summary: Screening for Prostate Cancer
Clinical Summary: Screening for Prostate Cancer Population Men aged 55 to 69 y Men 70 y and older The decision to be screened for prostate cancer should be Recommendation Do not screen for prostate cancer. an individual one. Grade: D Grade: C Before deciding whether to be screened, men aged 55 to 69 years should have an opportunity to discuss the potential benefits and harms of screening with their clinician and to incorporate their values and preferences in the decision. Screening offers a small potential benefit of reducing the chance of death from prostate cancer in some men. However, many men will experience potential harms of screening, including false-positive results that require additional testing and possible prostate biopsy; overdiagnosis and Informed Decision overtreatment; and treatment complications, such as incontinence and erectile dysfunction. Harms are greater for men 70 years Making and older. In determining whether this service is appropriate in individual cases, patients and clinicians should consider the balance of benefits and harms on the basis of family history, race/ethnicity, comorbid medical conditions, patient values about the benefits and harms of screening and treatment-specific outcomes, and other health needs. Clinicians should not screen men who do not express a preference for screening and should not routinely screen men 70 years and older. Risk Assessment Older age, African American race, and family history of prostate cancer are the most important risk factors for prostate cancer. Screening for prostate cancer begins with a test that measures the amount of prostate-specific antigen (PSA) protein in the blood. An elevated PSA level may be caused by prostate cancer but can also be caused by other conditions, including an enlarged Screening Tests prostate (benign prostatic hyperplasia) and inflammation of the prostate (prostatitis). -

Prostate Biopsy in the Staging of Prostate Cancer
Prostate Cancer and Prostatic Diseases (1997) 1, 54±58 ß 1997 Stockton Press All rights reserved 1365±7852/97 $12.00 Review Prostate Biopsy in the staging of prostate cancer L Salomon, M Colombel, J-J Patard, D Gasman, D Chopin & C-C Abbou Service d'Urologie, CHU, Henri Mondor, CreÂteil, France The use of prostate biopsies was developed in parallel with progress in our knowledge of prostate cancer and the use of prostate-speci®c antigen (PSA). Prostate biopsies were initially indicated for the diagnosis of cancer, by the perineal approach under general anesthesia. Nowadays prostate biopsies are not only for diagnostic purposes but also to determine the prognosis, particularly before radical prostatectomy. They are performed in patients with elevated PSA levels, by the endorectal approach, sometimes under local anesthesia.(1±3) The gold standard is the sextant biopsy technique described by Hodge4,5, which is best to diagnose prostate cancer, particularly in case of T1c disease (patients with serum PSA elevation).6±13 Patients with a strong suspicion of prostate cancer from a negative series of biopsies can undergo a second series14;15 with transition zone biopsy16,17 or lateral biopsy.18,19 Karakiewicz et al 20 and Uzzo et al 21 proposed that the number of prostate biopsies should depend on prostate volume to improve the positivity rate. After the diagnosis of prostate cancer, initial therapy will depend on several prognostic factors. In the case of radical prostatectomy, the results of sextant biopsy provide a wealth of information.22,23 The aim of this report is to present the information given by prostate biopsy in the staging of prostate cancer. -

ICD-9-CM C&M March 2011 Diagnosis Agenda
ICD-10 Coordination and Maintenance Committee Meeting March 19-20, 2014 Diagnosis Agenda Welcome and announcements Donna Pickett, MPH, RHIA Co-Chair, ICD-10 Coordination and Maintenance Committee Diagnosis Topics: Contents Opioid Induced Constipation ............................................................................................. 9 Severity of coronary calcification ................................................................................... 10 Sesamoid Fractures .......................................................................................................... 11 Familial Hypercholesterolemia ....................................................................................... 12 Bacteriuria ....................................................................................................................... 14 Mast Cell Activation Syndromes .................................................................................... 15 Necrotizing Enterocolitis ................................................................................................. 17 Hypertensive Crisis, Urgency and Emergency ................................................................ 18 Abnormal level of advanced glycation end products in tissues ...................................... 20 Cryopyrin-Associated Periodic Syndromes and Other Autoinflammatory Syndromes .. 22 Pulsatile Tinnitus ............................................................................................................. 26 In-Stent Restenosis of Coronary -

Prostate Cancer Screening NATIONAL GUIDELINE SUMMARY the Guideline Was Developed Using an Evidence-Based Methodology
Prostate Cancer Screening NATIONAL GUIDELINE SUMMARY The guideline was developed using an evidence-based methodology. This guideline summary is intended to guide health care professionals with prostate cancer screening in asymptomatic adult men. It does not apply to men who have signs or symptoms of prostate disease, or in whom a diagnosis has already been made. PROSTATE CANCER SCREENING AND Men with an elevated PSA have approximately a 70% chance of having a prostate biopsy that is negative for SHARED DECISION-MAKING cancer. • For average risk men, offer prostate cancer screening If a cancer is detected, it may or may not ever become with prostate-specifi c antigen (PSA) testing and digital clinically signifi cant3 in a man’s lifetime. rectal examination (DRE) in the context of a shared If diagnosed, the grade and stage of the cancer determines decision-making approach starting at age 50. the likely effectiveness of treatment. Potential benefi ts • For higher risk men (i.e., black/African-American of prostate cancer treatments may include increased life descent, family history of at least one fi rst degree span, and reduction in morbidity from locally advanced and relative with prostate cancer), offer prostate cancer metastatic disease. Prostate cancer treatments may also screening with PSA and DRE in the context of a shared have potential complications. Some men with prostate decision-making approach starting at age 40. cancer may elect not to be treated after discussion with their urologist. • Prostate cancer screening is not recommended for men age 75 or older. IF SCREENING IS REQUESTED • In the shared decision-making approach, include • For men who elect to participate in prostate cancer information regarding the potential benefi ts and risks screening: of undergoing screening for prostate cancer. -

Pattern of Prostate Cancer Presentation Among the Egyptian Population
351 Central European Journal of Urology O R I G I N A L P A P E R UROLOGICAL ONCOLOGY Pattern of prostate cancer presentation among the Egyptian population: A study in a single tertiary care center Ahmed Elabbady, Ahmed Eid, Ahmed Fahmy, Ahmed Fouad Kotb University of Alexandria, Faculty of Medicine, Department of Urology, Alexandria, Egypt Article history Introduction Prostate cancer is a common health problem that in the majority of cases starts to develop Submitted: April 22, 2014 at the age of 50 years, reaching its peak at 60–70 years of age. A variation in its incidence and prevalence Accepted: June 23, 2014 exists between western, Asian and Arabic populations. The aim of our work was to report the pattern of prostate cancer presentation in Alexandria University that as a tertiary referral center provides care for uro–oncology cases. Correspondence Ahmed Fouad Kotb Material and methods Data collection for all patients diagnosed with prostate cancer at Alexandria Uni- University of Alexandria versity in Egypt through the year 2012 was done. Faculty of Medicine Results The mean age of the patients was 67. Mean serum total PSA, prostate volume and PSAd were Department of Urology 149 ng/ml, 63 grams and 3.1 ng/ml/gm respectively. 25% of patients were asymptomatic diagnosed ac- El–Khartoum square, cidentally during screening for prostate cancer. The remaining group was presenting with LUTS, including Azarita Alexandria, Egypt 23 patients who presented initially with back pain. phone: +2 0120 302 1316 Conclusions Egyptian men with prostate cancer have a markedly high PSA density and Gleason grade [email protected] at diagnosis. -

Prostate Cancer Early Detection, Diagnosis, and Staging Finding Prostate Cancer Early
cancer.org | 1.800.227.2345 Prostate Cancer Early Detection, Diagnosis, and Staging Finding Prostate Cancer Early Catching cancer early often allows for more treatment options. Some early cancers may have signs and symptoms that can be noticed, but that is not always the case. ● Can Prostate Cancer Be Found Early? ● Screening Tests for Prostate Cancer ● American Cancer Society Recommendations for Prostate Cancer Early Detection ● Insurance Coverage for Prostate Cancer Screening Diagnosis and Planning Treatment After a cancer diagnosis, staging provides important information about the extent of cancer in the body and anticipated response to treatment. ● Signs and Symptoms of Prostate Cancer ● Tests to Diagnose and Stage Prostate Cancer ● Prostate Pathology ● Prostate Cancer Stages and Other Ways to Assess Risk ● Survival Rates for Prostate Cancer ● Questions To Ask About Prostate Cancer 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 Can Prostate Cancer Be Found Early? Screening is testing to find cancer in people before they have symptoms. For some types of cancer, screening can help find cancers at an early stage, when they are likely to be easier to treat. Prostate cancer can often be found early by testing for prostate-specific antigen (PSA) levels in a man’s blood. Another way to find prostate cancer is the digital rectal exam (DRE). For a DRE, the doctor puts a gloved, lubricated finger into the rectum to feel the prostate gland. These tests and the actual process of screening are described in more detail in Screening Tests for Prostate Cancer. If the results of either of these tests is abnormal, further testing (such as a prostate biopsy) is often done to see if a man has cancer. -

Needle Biopsy and Radical Prostatectomy Specimens David J Grignon
Modern Pathology (2018) 31, S96–S109 S96 © 2018 USCAP, Inc All rights reserved 0893-3952/18 $32.00 Prostate cancer reporting and staging: needle biopsy and radical prostatectomy specimens David J Grignon Department of Pathology and Laboratory Medicine, Indiana University School of Medicine, IUH Pathology Laboratory, Indianapolis, IN, USA Prostatic adenocarcinoma remains the most common cancer affecting men. A substantial majority of patients have the diagnosis made on thin needle biopsies, most often in the absence of a palpable abnormality. Treatment choices ranging from surveillance to radical prostatectomy or radiation therapy are largely driven by the pathologic findings in the biopsy specimen. The first part of this review focuses on important morphologic parameters in needle biopsy specimens that are not covered in the accompanying articles. This includes tumor quantification as well as other parameters such a extraprostatic extension, seminal vesicle invasion, perineural invasion, and lymphovascular invasion. For those men who undergo radical prostatectomy, pathologic stage and other parameters are critical in prognostication and in determining the appropriateness of adjuvant therapy. Staging parameters, including extraprostatic extension, seminal vesicle invasion, and lymph node status are discussed here. Surgical margin status is also an important parameter and definitions and reporting of this feature are detailed. Throughout the article the current reporting guidelines published by the College of American Pathologists and the International Collaboration on Cancer Reporting are highlighted. Modern Pathology (2018) 31, S96–S109; doi:10.1038/modpathol.2017.167 The morphologic aspects of prostatic adenocarcinoma hormonal therapy.4,5 For needle biopsy specimens the have a critical role in the management and prognos- data described below are largely based on standard tication of patients with prostatic adenocarcinoma. -
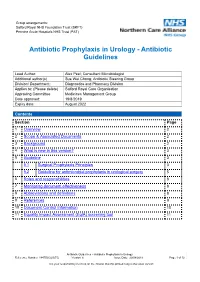
Antibiotic Prophylaxis in Urology - Antibiotic Guidelines
Group arrangements: Salford Royal NHS Foundation Trust (SRFT) Pennine Acute Hospitals NHS Trust (PAT) Antibiotic Prophylaxis in Urology - Antibiotic Guidelines Lead Author: Alex Peel; Consultant Microbiologist Additional author(s) Sue Wei Chong; Antibiotic Steering Group Division/ Department:: Diagnostics and Pharmacy Division Applies to: (Please delete) Salford Royal Care Organisation Approving Committee Medicines Management Group Date approved: 19/8/2019 Expiry date: August 2022 Contents Contents Section Page 1 Overview 2 2 Scope & Associated Documents 2 3 Background 2 4 What is new in this version? 3 5 Guideline 3 5.1 Surgical Prophylaxis Principles 3 5.2 Guideline for antimicrobial prophylaxis in urological surgery 5 6 Roles and responsibilities 8 7 Monitoring document effectiveness 8 8 Abbreviations and definitions 8 9 References 9 10 Document Control Information 10 11 Equality Impact Assessment (EqIA) screening tool 11 Antibiotic Guidelines – Antibiotic Prophylaxis in Urology Reference Number 144TD(C)25(F5) Version 6 Issue Date: 29/08/2019 Page 1 of 12 It is your responsibility to check on the intranet that this printed copy is the latest version Group arrangements: Salford Royal NHS Foundation Trust (SRFT) Pennine Acute Hospitals NHS Trust (PAT) 1. Overview This policy recommends surgical prophylaxis options for adult patients undergoing specified urological procedures. If you have any concerns about the content of this document please contact the author or advise the Document Control Administrator. 2. Scope This policy applies to all clinical staff involved the prescribing of antimicrobials, but particularly those involved in the perioperative care of patients undergoing urological surgery (namely urological surgeons and anaesthetists). Associated Documents 144TD(C)25(A5) - Issue No 3.1 - Antimicrobial Stewardship Policy http://intranet.srht.nhs.uk/policies-resources/trust-policy-documents/topics- prescriptions/antibiotic/antibiotic-prescribing-principles/144tdc25a5/ 163TD(C)(33) – Issue No.