ABS Booklet of Information
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
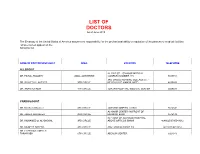
LIST of DOCTORS As of June 2018
LIST OF DOCTORS As of June 2018 The Embassy of the United States of America assumes no responsibility for the professional ability or reputation of the persons or medical facilities whose names appear on the following list. NAME OF DOCTOR/SPECIALIST AREA LOCATION TELEPHONE ALLERGIST AL-RAZI ST. - SAMOOR MEDICAL DR. FAISAL TBAILEH JABAL ALHUSSEIN COMPLEX NUMBER 145 5695151 3RD CIRCLE NURSING COLLAGE ST. - DR. SAYYED AL-NATHER 3RD CIRCLE NEAR HAYAT AMMAN HOTEL 4655893 DR. ANAN ALFAQIH 4TH CIRCLE JORDAN HOSPITAL/ MEDICAL CENTER 5609031 CARDIOLOGIST DR. Munther AlSaafeen 4TH CIRCLE JORDAN HOSPITAL CLINIC 5624840 AL-KHAIR CENTER- IN FRONT OF DR. ZAHER ALKASEEH 3RD CIRCLE HOUSING BANK 4645138 IN FRONT OF ALKHALDI HOSPITAL, DR. MOHAMED O. AL-BAGGAL 3RD CIRCLE ABOVE OPTICOS SHAMI 4646625/0795543012 DR. MUNEER AREEDA 4TH CIRCLE ABU HASSAN COMPLEX 4613613/4613614 DR. HATEM SALAMEH AL- TARAWNEH 5TH CIRCLE ABDOUN CENTER 5924343 DR. AHMAD MOHANNA AL ABDOUN CENTER, INFRONT OF ARABIC HARASEES 5TH CIRCLE CENTER 5924343 DR. IMAD HADAD 4TH CIRCLE JORDAN HOSPITAL CLINIC 5626197/0795303502 DR. NAZIH NAJEH AL-QADIRI 4TH CIRCLE JORDAN HOSPITAL CLINIC 5680060/0796999695 JABER IBN HAYYAN ST./ IBN HAYYAN DR. SUHEIL HAMMOUDEH SHMEISANI MEDICAL COMPLEX 5687484/0795534966 DR. YOUSEF QOUSOUS JABAL AMMAN AL-KHALIDI ST./ AL- BAYROUNI COMP. 4650888/0795599388 CARDIOVASCULAR SURGEON JABAL AMMAN NEAR ALKHALDI DR. SUHEIL SALEH 3RD CIRCLE HOSPITAL 4655772 / 079-5533855 COLORECTAL & GENERAL SURGERY DR. WAIL FATAYER KHALIDI HOSPITAL RAJA CENTER 5TH FLOOR 4633398 / 079-5525090 AL- RYAD COMP.BLDG NO. 41/ FLOOR DR. MARWAN S. RUSAN KHALIDI HOSPITAL ST. GROUND 4655772 / 0795530049 DR. JAMAL ARDAH TLA' AL- ALI IBN AL-HAYTHAM HOSPITAL 5602780 / 5811911 DENTISTS DENTAL CONSULTATION CENTER MAKA ST. -

Surgery Guidelines Infection Prevention
SURGERY GUIDELINES SURGICAL SITE INFECTION: REDUCING YOUR RISK A surgical site infection is a Stanford Hospital & Clinics is committed to implementing strategies to improve risk with any type of surgery. surgical care and to reduce the risk of You can take steps to reduce surgical site infections. your risk of surgical site We want your surgical experience at Stanford Hospital & Clinics to be positive. infection and complications. That experience includes educational • Talk with your healthcare provider materials that describe the process of your about your risk of infection and review surgery and the measures we take to ensure your safety. It is especially important to steps you can take to reduce your reduce the risk of infection. risk prior to the procedure. These are general guidelines. You will • Know the signs and symptoms be provided with more specific instructions of surgical site infection. related to your surgery before your discharge from the hospital. • Know how to reduce your risk while you are in the hospital. INFECTION PREVENTION stanfordhospital.org stanfordhospital.org PRIOR TO DAY OF AFTER SURGERY SURGERY SURGERY KEY POINTS HEALTHCARE TEAMS’ ROLE IN PREVENTION After your surgery and hospital stay, it is Tell your healthcare provider about other • Your surgeon may use electric clippers to important to watch for any changes in your medical problems you may have. Factors remove some of your hair before surgery. symptoms. Call your physician immediately or such as diabetes, obesity, smoking and some • Your surgical team will apply a skin antiseptic go to the nearest emergency room if you are medications could affect your surgery and immediately before the surgery experiencing any of the following symptoms: your treatment. -
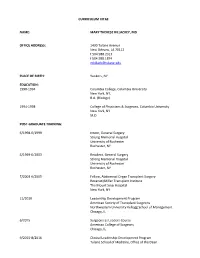
CV-Summer 2017.Pdf
CURRICULUM VITAE NAME: MARY THERESE KILLACKEY, MD OFFICE ADDRESS: 1430 Tulane Avenue New Orleans, LA 70112 t 504.988.2317 f 504.988.1874 [email protected] PLACE OF BIRTH: Yonkers, NY EDUCATION: 1990-1994 Columbia College, Columbia University New York, NY, B.A. (Biology) 1994-1998 College of Physicians & Surgeons, Columbia University New York, NY M.D. POST-GRADUATE TRAINING: 6/1998-6/1999 Intern, General Surgery Strong Memorial Hospital University of Rochester Rochester, NY 6/1999-6/2003 Resident, General Surgery Strong Memorial Hospital University of Rochester Rochester, NY 7/2003-6/2005 Fellow, Abdominal Organ Transplant Surgery Recanati/Miller Transplant Institute The Mount Sinai Hospital New York, NY 11/2010 Leadership Development Program American Society of Transplant Surgeons Northwestern University Kellogg School of Management Chicago, IL 6/2015 Surgeons as Leaders Course American College of Surgeons Chicago, IL 9/2015-8/2016 Clinical Leadership Development Program Tulane School of Medicine, Office of the Dean New Orleans, LA 12/2015 Mid-Career Women Faculty Professional Development Seminar Association of American Medical Colleges Austin, TX 6/2016 Being a Resilient Leader Association of American Medical Colleges Washington, DC 6/2017 - 4/2018 Fellow, Executive Leadership in Academic Medicine Drexel University College of Medicine Philadelphia, PA ACADEMIC APPOINTMENTS: 7/2003-6/2005 Instructor in Surgery Mount Sinai School of Medicine New York, NY 10/2006-present Assistant Professor of Surgery and Pediatrics Tulane University -
Partnering with Your Transplant Team the Patient’S Guide to Transplantation
Partnering With Your Transplant Team The Patient’s Guide to Transplantation U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Health Resources and Services Administration This booklet was prepared for the Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation by the United Network for Organ Sharing (UNOS). PARTNERING WITH YOUR TRANSPLANT TEAM THE PATIENT’S GUIDE TO TRANSPLANTATION U.S. Department of Health and Human Services Health Resources and Services Administration Public Domain Notice All material appearing in this document, with the exception of AHA’s The Patient Care Partnership: Understanding Expectations, Rights and Responsibilities, is in the public domain and may be reproduced without permission from HRSA. Citation of the source is appreciated. Recommended Citation U.S. Department of Health and Human Services (2008). Partnering With Your Transplant Team: The Patient’s Guide to Transplantation. Rockville, MD: Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation. DEDICATION This book is dedicated to organ donors and their families. Their decision to donate has given hundreds of thousands of patients a second chance at life. CONTENTS Page INTRODUCTION.........................................................................................................................1 THE TRANSPLANT EXPERIENCE .........................................................................................3 The Transplant Team .......................................................................................................................4 -

Medications to Avoid Before Surgery
ENTRUST MEDICAL GROUP Pre‐operative Information Medications to Avoid Before Surgery It is important to avoid certain medications prior to surgery. The following medications can have effects on bleeding, swelling, increase the risk of blood clots, and cause other problems if taken around the time of surgery. Please notify your surgeon’s office if you are taking any vitamins, herbal medications/supplements as these can also cause problems during your surgery and should not be taken for the two week period before surgery and one week after surgery. It is extremely important that if you come down with a cold, fever, rash, or “any new” medical problem close to your surgery date, you should notify your surgeon’s office immediately. Section One: The following drugs contain aspirin and/or aspirin like effects that may affect your surgery (abnormal bleeding and bruising). These drugs should be avoided for at least two weeks prior to surgery. A.P.C. Doloprin Nuprin A.S.A. Easprin Orudis A.S.A. Enseals Ecotrin Pabalate‐SF Advil Emprin with Codeine Pamelor Aleve Endep Parnate Alka‐Seltzer Plus Equagesic Tablets Percodan Alka‐Seltzer Etrafon Pepto‐Bismol (all types) Anacin Excedrin Persantine Anaprox Feldene Phenteramine Ansaid Fiorinal Phenylbutzone Argesic Flagly Ponstel Arthritis pain formula Four Way Cold Tablets Propoxyphene Compound Arthritis strength Bufferin Gemnisyn Robaxisal Arthropan Liquid Gleprin Rufen AS.A. Goody’s S‐A‐C Ascriptin Ibuprofen (all types) Saleto Asperbuf Indocin Salocol Aspergum Indomethacin Sine‐Aid/Sine‐Off/Sinutab Aspirin (all brands) Lanorinal SK‐65 Compound Atromid Lioresal St. Joseph’s Cold Tab B.C. -

Organ Transplant Discrimination Against People with Disabilities Part of the Bioethics and Disability Series
Organ Transplant Discrimination Against People with Disabilities Part of the Bioethics and Disability Series National Council on Disability September 25, 2019 National Council on Disability (NCD) 1331 F Street NW, Suite 850 Washington, DC 20004 Organ Transplant Discrimination Against People with Disabilities: Part of the Bioethics and Disability Series National Council on Disability, September 25, 2019 This report is also available in alternative formats. Please visit the National Council on Disability (NCD) website (www.ncd.gov) or contact NCD to request an alternative format using the following information: [email protected] Email 202-272-2004 Voice 202-272-2022 Fax The views contained in this report do not necessarily represent those of the Administration, as this and all NCD documents are not subject to the A-19 Executive Branch review process. National Council on Disability An independent federal agency making recommendations to the President and Congress to enhance the quality of life for all Americans with disabilities and their families. Letter of Transmittal September 25, 2019 The President The White House Washington, DC 20500 Dear Mr. President, On behalf of the National Council on Disability (NCD), I am pleased to submit Organ Transplants and Discrimination Against People with Disabilities, part of a five-report series on the intersection of disability and bioethics. This report, and the others in the series, focuses on how the historical and continued devaluation of the lives of people with disabilities by the medical community, legislators, researchers, and even health economists, perpetuates unequal access to medical care, including life- saving care. Organ transplants save lives. But for far too long, people with disabilities have been denied organ transplants as a result of unfounded assumptions about their quality of life and misconceptions about their ability to comply with post-operative care. -

General Surgery
- 1 - KALEIDA HEALTH Name: ___________________________________ Date: ____________________________ DELINEATION OF PRIVILEGES - GENERAL SURGERY PLEASE NOTE: Please check the box for each privilege requested. Do not use an arrow or line to make selections. We will return applications that ignore this directive. GENERAL STATEMENTS - Privileges in Adult Surgery are separated into the following divisions: General Surgery and Plastic Surgery. Applicants desiring procedure privileges in more than one division must complete separate forms for each. Procedures designated with an asterisk (*) indicate that Moderate or Deep Sedation may be required. If you do not have Moderate or Deep Sedation privileges, you must invite a Kaleida Health anesthesiologist to participate in the procedure. Procedures are also separated into levels of complexity (Level I-A, Level I-B, Level I, Level II, and Level III), which require increasing levels of education and experience. In general, procedures learned during residency are grouped in Level I-A or Level I and are granted upon evidence of successful completion of residency training. Level II procedures may or may not require evidence of additional training beyond residency. Documentation of additional training and/or experience is required for all Level III procedures. LEVEL I-A PRIVILEGES Procedures which involve primarily wound care, can be done under local anesthetic and occasionally involve application of temporary skin coverage or application of agents to expedite wound healing. Can be performed by any competent -

General Surgery Career Resource
The American Journal of Surgery (2013) 206, 719-723 Association of Women Surgeons: Career Development Resources General surgery career resource Ana M. Parsee, M.D.a, Sharona B. Ross, M.D.b, Nancy L. Gantt, M.D.c, Kandace Kichler, M.D.d, Celeste Hollands, M.D.e,* aJohns Hopkins Hospital, Baltimore, MD, USA; bFlorida Hospital, Tampa, FL, USA; cNortheast Ohio Medical University, St. Elizabeth Health Center, Rootstown, OH, USA; dUniversity of Miami, Palm Beach Regional Campus, Palm Beach, FL, USA; eSt John’s Children’s Hospital, Springfield, IL, USA KEYWORDS: Abstract General surgery residency training can lead to a rewarding career in general surgery and General surgery; serve as the foundation for careers in several surgical subspecialties. It offers broad-based training with General surgery exposure to the cognitive and technical aspects of several surgical specialties and prepares graduating residency; residents for a wide range of career paths. This career development resource discusses the training as- Surgical fellowship; pects of general surgery. Surgical subspecialties; Ó 2013 Elsevier Inc. All rights reserved. Transition to practice; Surgery interest groups General surgery training provides the foundation for who enter medical school with an interest in surgery and many different surgical career paths. The training begins those who become interested early can become involved with a general surgery residency, which is usually followed in their schools’ surgery interest group (SIGs) as early as by either entry into practice or additional training. General the first day of medical school at most institutions. Each surgery residency programs provide broad-based training local SIG has different offerings to help students explore with exposure to the cognitive and technical aspects of and develop their interest in surgery as a career. -

Medical Terminology Abbreviations Medical Terminology Abbreviations
34 MEDICAL TERMINOLOGY ABBREVIATIONS MEDICAL TERMINOLOGY ABBREVIATIONS The following list contains some of the most common abbreviations found in medical records. Please note that in medical terminology, the capitalization of letters bears significance as to the meaning of certain terms, and is often used to distinguish terms with similar acronyms. @—at A & P—anatomy and physiology ab—abortion abd—abdominal ABG—arterial blood gas a.c.—before meals ac & cl—acetest and clinitest ACLS—advanced cardiac life support AD—right ear ADL—activities of daily living ad lib—as desired adm—admission afeb—afebrile, no fever AFB—acid-fast bacillus AKA—above the knee alb—albumin alt dieb—alternate days (every other day) am—morning AMA—against medical advice amal—amalgam amb—ambulate, walk AMI—acute myocardial infarction amt—amount ANS—automatic nervous system ant—anterior AOx3—alert and oriented to person, time, and place Ap—apical AP—apical pulse approx—approximately aq—aqueous ARDS—acute respiratory distress syndrome AS—left ear ASA—aspirin asap (ASAP)—as soon as possible as tol—as tolerated ATD—admission, transfer, discharge AU—both ears Ax—axillary BE—barium enema bid—twice a day bil, bilateral—both sides BK—below knee BKA—below the knee amputation bl—blood bl wk—blood work BLS—basic life support BM—bowel movement BOW—bag of waters B/P—blood pressure bpm—beats per minute BR—bed rest MEDICAL TERMINOLOGY ABBREVIATIONS 35 BRP—bathroom privileges BS—breath sounds BSI—body substance isolation BSO—bilateral salpingo-oophorectomy BUN—blood, urea, nitrogen -

Regulation 4 —Pharmacy
Agency # 070.00 REGULATION 4 —PHARMACY 04-00: GENERAL REGULATIONS REGARDING PHARMACIES 04-00-0001—EQUIPMENT SPECIFICATIONS Prescription equipment appropriate for the pharmacy’s specific scope of practice shall be maintained by the pharmacy and may include but is not limited to: (a) Graduates capable of measuring from 0.1ml to at least 120ml (b) Mortars and pestles--at least one (porcelain or glass) (c) Hot and cold running water in the prescription department (d) Spatulas (e) Ointment slab or ointment papers (f) Exempt narcotic record book (g) Class III balance and weights or comparable electronic scale (h) Equipment for labeling (i) Refrigeration for the proper storage of biologicals and other medications. Medications shall be stored in a separate compartment or area from food. Each pharmacy shall maintain a pharmacy library: (1) available for use by the pharmacist and the patient, including either current drug information manuals, or computers capable of printing current drug information for the pharmacist and patient drug information and monographs for patients. (2) other pharmacy reference books and periodicals necessary for effective pharmacy practice. EXCEPTIONS: Pharmacies meeting the requirements of regulation 04-02-0100 or regulation 07-02-0001 shall be exempt from requirements of this regulation when not applicable. (10/09/80, Revised 6/25/83, 4/07/89, 6/07/90, 8/20/97, 11/1/2007 and 11/6/2008) 04-00-0002—TIME REQUIRMENTS FOR PHARMACIES AND FOR THE PHARMACIST IN CHARGE (a) Unless expressly provided otherwise in Board regulations, all pharmacies in Arkansas shall be open a minimum of forty (40) hours per week and have on duty an Arkansas licensed pharmacist in charge. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Posterior Cervical Discectomy: an Optimally Invasive Approach to Laterally Prolapsed Cervical Disc
Original Research Article DOI: 10.18231/2455-8451.2016.0005 Posterior cervical discectomy: An optimally invasive approach to laterally prolapsed cervical disc Shashank Sah1,*, Suresh Kumar Kaushik2, Neeraj Prajapati3 1Associate Professor, Dept. of General Surgery, 2Associate Professor, Dept. of Orthopaedics, 3Associate Professor, Dept. of Radiology, SRMSIMS, Bareilly, Uttar Pradesh *Corresponding Author: Email: [email protected] Abstract Aim: Posterior cervical discectomy is one of the surgical techniques for management of laterally prolapsed cervical disc causing cervical radiculopathy. This method has remained under-utilized in comparison to the classic technique of Anterior Cervical Discectomy and Fusion (ACDF). The study was conducted to evaluate it’s feasibility in terms of ease, challenges and short term outcome. Material and Methods: This is a prospective study conducted over a period of 65 months. Patients visiting to neurosurgery/ orthopedics OPD’s with cervical disc diseases and requiring surgery, were further evaluated on the basis of selection criteria for the feasibility of posterior cervical discectomy. Patients meeting the selection criteria were then operated upon by this approach and the outcome was evaluated. Results: Posterior cervical discectomy is essentially a disc conserving, optimally invasive microscopic technique - best suited for selected subset of patients with laterally prolapsed disc causing radiculopathy. 21 out of 23 patients appreciated the surgical benefit by as early as 48 hours of operation. There were no complications. Conclusion: Posterior cervical discectomy is an excellent direct approach to the diseased segment provided case selection criteria are properly followed. Keywords: Cervical disc, Posterior cervical discectomy, Lamino-foraminotomy, Motion preserving cervical disc surgery Introduction approach has largely remained underutilized and Cervical disc disease is a prevalent and disabling therefore in the present study we evaluated this disorder.