M:\Internet Docs\2009Minutes Pages\Hhelmin.Wpd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
2019 Public Policy Report
Public Policy Report • 2019 Table of Contents 3 Letter from IACI Board Chair 4 2019 Session Wrap-Up Tax Conformity Medicaid Expansion State Budget Workforce Development Industrial Electricians Land Use Planning Administrative Rules Campaign Finance Mining in Idaho Transportation Funding 10 New Laws Passed in 2019 18 2019 Legislation Tracking List 22 2019 Legislative Voting Records 24 Vision, Values & Mission 25 Statement of Public Policy 30 2019 IACI 45th Anniversary Conference Agenda Speakers Sponsors 2 Public Policy Report 2019 Letter from the Chair I am honored to be the current Board Chairman of the Idaho Association of Commerce & Industry (IACI), representing Employers Advocating Economic Opportunity in Idaho.® Our membership is comprised of hundreds of employers, throughout the state of Idaho, employing over 200,000 Idahoans. IACI members work together to influence good public policy to enhance Idaho’s business climate, and provide economic opportunity and certainty in its regulations. Throughout the year IACI works on critical issues, such as taxes, health care, education/workforce, environment and regulations, workers’ compensation, unemployment, employer liability, and controlling the cost and growth of government. IACI was founded in 1974, and we’re excited to be celebrating our 45th anniversary this year as a critical fixture in Idaho’s legislative and policy-making arena. IACI’s membership is comprised of employers of every size and across every industry in Idaho—making it Idaho’s broadest-based, most diverse business association, earning the respect and ear of the state’s elected and policy leaders. For those who are able to participate in our Annual Public Policy Conference in Coeur d’Alene this year, we’ve put together an excellent program focused on workforce development and education. -
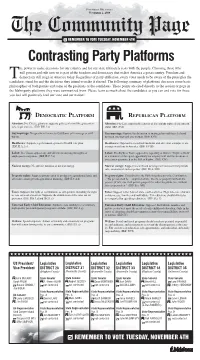
Contrasting Party Platforms He Power to Make Decisions for Our Country and for Our State Ultimately Rests with the People
PAID FOR BY MELALEUCA NOVEMBER 2, 2008 The Community Page 3 REMEMBER TO VOTE TUESDAY, NOVEMBER 4TH Contrasting Party Platforms he power to make decisions for our country and for our state ultimately rests with the people. Choosing those who will govern and rule over us is part of the freedom and democracy that makes America a great country. Freedom and democracy still reign in America today. Regardless of party affiliation, every voter needs to be aware of the principles the candidatesT stand for and the decisions they intend to make if elected. The following summary of platforms discusses some basic philosophies of both parties and some of the positions of the candidates. These points are cited directly to the section or page in the Idaho party platforms they were summarized from. Please learn as much about the candidates as you can and vote for those you feel will positively lead our state and our nation! DEMOCRATIC PLATFORM RE P UBLICAN PLATFORM © © Abortion: Pro-Choice, platform supports policies that will keep abortion Abortion: Pro-Life, support the sanctity of life and the rights of the unborn safe, legal and rare. (IDP, II.E.1.c) child. (IRP, XVI) Gay marriage: No specific reference to Gay/Same-sex marriage or civil Gay marriage: Oppose the definition of marriage beyond that of a bond unions. between one man and one woman. (IRP, XVI) Healthcare: Supports a government-sponsored health care plan. Healthcare: Opposed to socialized medicine and any other attempts to en- (IDP, II.A.2.c) courage socialism in America. (IRP, XVIII) Labor: Pro-Union, oppose any and all laws restricting the rights of Labor: Pro-Right to Work, opposed to repealing of Idaho’s “Right to Work” employees to organize. -

2014 Political Corporate Contributions 2-19-2015.Xlsx
2014 POLITICAL CORPORATE CONTRIBUTIONS Last Name First Name Committee Name State Office District Party 2014 Total ($) Alabama 2014 PAC AL Republican 10,000 Free Enterprise PAC AL 10,000 Mainstream PAC AL 10,000 Collins Charles Charlie Collins Campaign Committee AR Representative AR084 Republican 750 Collins‐Smith Linda Linda Collins‐Smith Campaign Committee AR Senator AR019 Democratic 1,050 Davis Andy Andy Davis Campaign Committee AR Representative AR031 Republican 750 Dotson Jim Jim Dotson Campaign Committee AR Representative AR093 Republican 750 Griffin Tim Tim Griffin Campaign Committee AR Lt. Governor AR Republican 2,000 Rapert Jason Jason Rapert Campaign Committee AR Senator AR035 Republican 1,000 Rutledge Leslie Leslie Rutledge Campaign Committee AR Attorney General AR Republican 2,000 Sorvillo Jim Jim Sorvillo Campaign Committee AR Representative AR032 Republican 750 Williams Eddie Joe GoEddieJoePAC AR Senator AR029 Republican 5,000 Growing Arkansas AR Republican 5,000 Senate Victory PAC AZ Republican 2,500 Building Arizona's Future AZ Democratic 5,000 House Victory PAC AZ Republican 2,500 Allen Travis Re‐Elect Travis Allen for Assembly 2014 CA Representative CA072 Republican 1,500 Anderson Joel Tax Fighters for Joel Anderson, Senate 2014 CA Senator CA038 Republican 2,500 Berryhill Tom Tom Berryhill for Senate 2014 CA Senator CA008 Republican 2,500 Bigelow Frank Friends of Frank Bigelow for Assembly 2014 CA Representative CA005 Republican 2,500 Bonin Mike Mike Bonin for City Council 2013 Officeholder Account CA LA City Council -

Chapter 11 Distribution List
CHAPTER 11 DISTRIBUTION LIST The U.S. Department of Energy (DOE) provided copies of this Draft Tank Closure and Waste Management Environmental Impact Statement for the Hanford Site, Richland, Washington (TC & WM EIS) to Federal, state, and local elected and appointed officials and public interest groups; American Indian tribal representatives; and other organizations and individuals listed in this chapter. Approximately 300 copies of the complete Draft TC & WM EIS and 3,000 copies of the Draft TC & WM EIS Summary were distributed, along with a compact disk of the complete Draft TC & WM EIS. Copies will be provided to others upon request. UNITED STATES CONGRESS U.S. House of Representatives Idaho The Honorable Peter DeFazio, District 4 The Honorable Walter Minnick, District 1 The Honorable Kurt Schrader, District 5 The Honorable Mike Simpson, District 2 Washington Nevada The Honorable Jay Inslee, District 1 The Honorable Shelley Berkley, District 1 The Honorable Rick Larsen, District 2 The Honorable Dean Heller, District 2 The Honorable Brian Baird, District 3 The Honorable Dina Titus, District 3 The Honorable Doc Hastings, District 4 The Honorable Cathy McMorris Rodgers, New Mexico District 5 The Honorable Martin Heinrich, District 1 The Honorable Norman D. Dicks, District 6 The Honorable Harry Teague, District 2 The Honorable Jim McDermott, District 7 The Honorable Ben Lujan, District 3 The Honorable David G. Reichert, District 8 Oregon The Honorable Adam Smith, District 9 The Honorable David Wu, District 1 The Honorable Greg Walden, District 2 The Honorable Earl Blumenauer, District 3 U.S. House of Representatives Committees Committee on Appropriations The Honorable Dave Obey, Chairman The Honorable Jerry Lewis, Ranking Member Committee on Appropriations, Subcommittee on Energy and Water Development The Honorable Peter J. -

2010 Legislative Directory
TABLE OF CONTENTS CONTENTS Senate Leadership and Administration ................................. 2 House Leadership and Administration .................................. 3 Legislative Staff Offices ......................................................... 4 Legislative Council ................................................................. 5 Important Session Dates ....................................................... 5 Senators, Alphabetical ........................................................... 6 Representatives, Alphabetical ............................................... 8 Legislators by District ............................................................12 Floor Maps .............................................................................47 Senate Committees ...............................................................55 House Committees ................................................................59 Legislative Attachés & Support Staff .....................................66 State Government ..................................................................72 Elected Officials .....................................................................80 Capitol Correspondents .........................................................82 Orders of Business ................................................................84 How to Contact Legislators Web Site .................................... www.legislature.idaho.gov Informationneed at end Center to justify ......................................... 208-332-1000 Tollneed -

2020-Idaho-Freedom-Index-Official-1.Pdf
To read any of the 271 bill analyses IFF published this legislative session, or to research your lawmakers’ voting records, please visit: IDAHOFREEDOMINDEX.COM FROM THE PRESIDENT During an Idaho House floor debate earlier this year, state Rep. Fred Wood, R-Burley, said outside bill ratings aren’t welcome in lawmakers’ deliberations. Wood, who couldn’t summon the courage to utter our name, was speaking about the Idaho Freedom Index. Please know 2020 was a banner year for the Idaho Freedom Index, our flagship project. IFF launched the Index in 2012 to help you hold lawmakers accountable for their votes. This year, it earned unprecedented attention from legislators, lobbyists, and Idahoans. A select few highlights demonstrate the Index’s formidability. Web traffic to the Index and IFF analyses surged more than 40 percent above 2019 levels. This year, lawmakers talked about the Idaho Freedom Index in public meetings more than a dozen times. Finally, lobbyists, who once scoffed at the Index, beat a path to our office seeking assistance to improve their legislation. I want to recognize those who worked tirelessly to bring about this banner year. First, IFF donors deserve immense credit. Their support makes this service available in our state. Next, I bring to your attention IFF Policy Analyst Lindsay Atkinson, who coordinated the Index and evaluated countless bills. Finally, a heartfelt thank you goes to IFF Vice President Fred Birnbaum and Parrish Miller. Both worked long hours and dove deep into legislation to write analyses. I understand the Idaho Freedom Index makes some lawmakers uncomfortable. Accountability to voters causes discomfort for legislators who say one thing on the campaign trail but do another in the Statehouse. -

House Journal Idaho Legislature
[December 1, 2016 HOUSE JOURNAL 1 29 ................ Dustin Whitney Manwaring (R), Elaine Smith (D) HOUSE JOURNAL 30 .................................Jeff Thompson (R), Wendy Horman (R) OF THE 31 .............................Neil A. Anderson (R), Julie VanOrden (R) 32 ......................................Marc Gibbs (R), Tom Loertscher (R) 33 .............................. Janet Trujillo (R), Bryan N. Zollinger (R) IDAHO LEGISLATURE 34 ............................................Ron Nate (R), Dell Raybould (R) ORGANIZATIONAL SESSION 35 ...................................Van Burtenshaw (R), Karey Hanks (R) SIXTY-FOURTH LEGISLATURE IN TESTIMONY WHEREOF, I have hereunto set my hand and affixed the Great Seal of the State of Idaho. Done at Boise, the Capital of Idaho, this Twenty-eighth day of November, in the year of our Lord, two thousand and sixteen, and of the Independence FIRST ORGANIZATIONAL DAY of the United States of America, the two hundred and forty-first. THURSDAY, DECEMBER 1, 2016 /s/ LAWERENCE DENNEY Secretary of State House of Representatives The Certificate of Election was ordered filed in the office of At the hour of 9 a.m., on Thursday, December 1, 2016, the the Chief Clerk. members-elect of the House of Representatives convened in the Roll call showed all 70 members present. House Chamber of the Capitol Building in the City of Boise, with the Honorable Scott Bedke, Speaker of the House of the At this time, Speaker Bedke administered the oath of office Sixty-third Legislature presiding, assisted by Carrie Maulin, to all members-elect. Chief Clerk. Prayer was offered by Representative Raybould. The Chief Clerk read the official proclamation as follows: The Pledge of Allegiance was led by Speaker Bedke. I, LAWERENCE DENNEY, Secretary of State of the State of Idaho and legal custodian of the records of elections held in There being no objection, the House advanced to the Seventh the State of Idaho, do hereby certify that the following is a full, Order of Business. -

Volume 21 Special Voters Edition
THE GEM STATE PATRIOT All Around Idaho Inc. Publication Knowledge is Power as Silence is Consent. We will Volume 21, October 15 , 2014 bring you the knowledge so you can rise up and © restore freedom and liberty back to our country. Welcome to The Gem State Patriot, we are a not-for-profit newsletter. GOVERNOR NOT MENTIONED IN RUSS FULCHER OP-ED ON PAGE 3 The staff of the Gem State Patriot has taken the time to put out this special voters issue. We have also enclosed a list of legislative candidates up for election in 2014 in each of our thirty five counties in the State of Idaho. All we are asking is for you to get out and vote on November 4th. If you want to change our state than you have to participate in deciding who will be in charge. REMEMBER WE GET THE GOVERNMENT WE DESERVE. PLEASE VOTE ON NOVEMBER 4TH. Please direct any comments or requests for subscriptions to this newsletter to: Bob Neugebauer: Publisher E-mail - [email protected] Phone - 208-887-2144 Judy Neugebauer: Editor E-mail - [email protected] Phone - 208-887-2144 www.GemStatePatriot.com 1 INSIDE OF THIS ISSUE PAGE 3 Governors name not mentioned in Fulcher OPED. Russ writes about principled republicans standing together. Surly Senator Fulcher had a lot of pressure on him to endorse Governor Otter but instead he endorsed the party platform and did not compromise his principals. Important information concerning the ballot question about a constitutional amendment giving PAGE 4,5 the legislature the right to change any rule they deem improper that is made by a ruling state agency. -

5-21-15 UPDATED FORMAT MGGF Contributions July
MGGF CONTRIBUTIONS JULY 1, 2014 - DECEMBER 31, 2014 In an effort to improve Monsanto's political disclosures, this report dated January 1, 2014-June 30, 2014 is formatted differently than past reports. Name State Candidate Amount Party Total LIEUTENANT GOVERNOR Kay Ivey for Lt. Governor AL Hon. Kay E. Ivey (R) $1,000 REP STATE SENATE Friends of Del Marsh AL Sen. Del Marsh (R) $1,000 REP STATE HOUSE Craig Ford Campaign Fund AL Rep. Craig Ford (D) $500 DEM Johnny Mack Morrow Campaign AL Rep. Johnny Mack Morrow (D) $1,000 DEM Friends of Will Ainsworth AL Rep. William Ainsworth (R) $500 REP Jack Williams Campaign AL Rep. Jack Williams (R) $1,000 REP RIchard Lindsey Campaign Fund AL Rep. Richard J. Lindsey (D) $500 DEM ALABAMA TOTAL $5,500 GOVERNOR Asa for Governor AR Gov. Asa Hutchinson (R) $2,000 REP STATE SENATE Thompson for State Senate AR Sen. Robert F. Thompson (D) $1,000 DEM Terry Rice for State Senate AR Sen. Terry Rice (R) $1,000 REP Hickey for Senate AR Sen. Jimmy Hickey, Jr. (R) $1,000 REP STATE HOUSE Davis for State Representative AR Rep. Andy Davis (R) $500 REP Bragg for State Representative AR Rep. Ken Bragg (R) $500 REP Committee to Elect Nate Bell AR Rep. Nate Bell (R) $500 REP Harold Copenhaver for State Representative AR Rep. Harold Copenhaver (D) $500 DEM ARKANSAS TOTAL $7,000 STATE ASSEMBLY Garcia for Assembly 2014 CA Assm. Cristina Garcia (D) $1,500 DEM CALIFORNIA TOTAL $1,500 OTHER Coalition Against the Misleading Labeling Measure CO $3,404,150 NP Colorado BioScience Political Action Committee CO $550 NP COLORADO TOTAL $3,404,700 AGRICULTURE COMMISSIONER Putnam for AG Commissioner FL Commissioner Adam H. -
Legislative Branch
Legislative Branch Chamber and 4th Floor Gallery Photo Courtesy of Taner Oz Legislative Districts 144 IDAHO BLUE BOOK Legislative Branch The Idaho Legislature is responsible success can be attributed to the fact that for translating the public will into Idaho’s legislators are “citizen” legislators, public policy for the state, levying taxes, not career politicians. They are farmers appropriating public funds, and overseeing and ranchers, business men and women, the administration of state agencies. These lawyers, doctors, sales people, loggers, responsibilities are carried out through the teachers. Elected for two-year terms and legislative process -- laws passed by elected in session at the Capitol just three months representatives of the people, legislators. each year, Idaho’s citizen legislators are able Since statehood in 1890, Idaho’s legislators to maintain close ties to their communities have enjoyed a rich and successful history and a keen interest in the concerns of the of charting the state’s growth. Much of that electorate. The Legislature’s Mission The Idaho Legislature is committed to • Preserve the state’s environment and carrying out its mission in a manner that ensure wise, productive use of the inspires public trust and confidence in state’s natural resources; elected government and the rule of law. • Carry out oversight responsibilities to The mission of the Legislature is to: enhance government accountability; and • Preserve the checks and balances of • Raise revenues and appropriate monies state government by the independent that support necessary government Legislative exercise of legislative powers; services. • Adopt a system of laws that promote the health, education and well-being of Idaho’s citizens; The Chambers The Idaho State Capitol, constructed in accommodate a growing Legislature. -

Idaho State Legislative Members
IDAHO STATE LEGISLATIVE MEMBERS SESSION BEGINS Legend 62nd IDAHO STATE LEGISLATURE JANUARY 7, 2013 S - Senator FIRST REGULAR SESSION R - Representative (D) Democrat (R) Republican 1 S - Shawn Keough (R) 7 S - Sheryl Nuxoll (R) 18 S - Branden Durst (D) State Legislative District Boundary R - Eric Anderson (R) R - Shannon McMillan (R) R - Janie Ward-Engelking (D) 10 State Legislative District Number R - George Eskridge (R) R - Paul Shepherd (R) R - Phylis K. King (D) 1st Congressional District 2nd Congressional District 2 S - Steve Vick (R) 8 S - Steven Thayn (R) 19 S - Cherie Buckner-Webb (D) County Boundary R - Vito Barbieri (R) R - Terry F. Gestrin (R) R - Mathew Erpelding (D) R - Ed Morse (R) R - Lenore Barrett (R) R - Holli Woodings (D) 3 S - Bob Nonini (R) 9 S - Monty Pearce (R) 20 S - Chuck Winder (R) Boundary R - Ron Mendive (R) R - Lawerence E. Denney (R) R - Joe Palmer (R) R - Frank Henderson (R) R - Judy Boyle (R) R - James Holtzclaw (R) 1 4 S - John W. Goedde (R) 10 S - Jim Rice (R) 21 S - Clifford R. Bayer (R) Bonner R - Luke Malek (R) R - Brandon Hixon (R) R - Steven C. Harris (R) R - Kathleen Sims (R) R - Darrell Bolz (R) R - Thomas E. Dayley (R) 5 S - Dan J. Schmidt (D) 11 S - Patti Anne Lodge (R) 22 S - Russell M. Fulcher (R) R - Cindy Agidius (R) R - Gayle Batt (R) R - John Vander Woude (R) 4 R - Shirley G. Ringo (D) R - Christy Perry (R) R - Jason Monks (R) 2 3 6 S - Dan Johnson (R) 12 S - Todd Lakey (R) 23 S - Bert Brackett (R) Kootenai R - Thyra Stevenson (R) R - Robert Anderst (R) R - Rich Wills (R) Shoshone R - John Rusche (D) R - Rick D. -

2020 Contributions
State Candidate Names Committee Amount Party Office District CA Holmes, Jim Jim Holmes for Supervisor 2020 $ 700 O County Supervisor 3 CA Uhler, Kirk Uhler for Supervisor 2020 $ 500 O County Supervisor 4 CA Gonzalez, Lena Lena Gonzalez for Senate 2020 $ 1,500 D STATE SENATE 33 CA Lee, John John Lee for City Council 2020 - Primary $ 800 O City Council 12 CA Simmons, Les Simmons for City Council 2020 $ 1,000 D City Council 8 CA Porada, Debra Porada for City Council 2020 $ 500 O City Council AL CA California Manufacturers & Technology Association Political Action Committee $ 5,000 CA Desmond, Richard Rich Desmond for Supervisor 2020 $ 1,200 R County Supervisor 3 CA Hewitt, Jeffrey Jeffrey Hewitt for Board of Supervisors Riverside County 2018 $ 1,200 O County Supervisor 5 CA Gustafson, Cindy Elect Cindy Gustafson Placer County Supervisor, District 5 - 2020 $ 700 O County Supervisor 5 CA Cook, Paul Paul Cook for Supervisor 2020 $ 1,000 R County Supervisor 1 CA Flores, Dan Dan Flores for Supervisor 2020 $ 500 County Supervisor 5 CA California Taxpayers Association - Protect Taxpayers Rights $ 800,000 CA Latinas Lead California $ 500 CA Wapner, Alan Wapner for Council $ 1,000 City Council CA Portantino, Anthony Portantino for Senate 2020 $ 2,000 D STATE SENATE 25 CA Burke, Autumn Autumn Burke for Assembly 2020 $ 2,000 D STATE HOUSE 62 CA California Republican Party - State Account $ 15,000 R CA Fong, Vince Vince Fong for Assembly 2020 $ 1,500 D STATE HOUSE 34 CA O'Donnell, Patrick O'Donnell for Assembly 2020 $ 4,700 D STATE HOUSE 70 CA Sacramento Metropolitan Chamber Political Action Committee $ 2,500 CA Patterson, Jim Patterson for Assembly 2020 $ 1,500 R STATE HOUSE 23 CA Arambula, Joaquin Dr.