An Alternative Non-Invasive Therapy for Refractory Angina
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

National Cardiogenic Shock Initiative
EXCLUSION CRITERIA NATIONAL CARDIOGENIC SHOCK INITIATIVE Evidence of Anoxic Brain Injury Unwitnessed out of hospital cardiac arrest or any cardiac arrest in which ROSC is not ALGORITHM achieved in 30 minutes IABP placed prior to Impella Septic, anaphylactic, hemorrhagic, and neurologic causes of shock Non-ischemic causes of shock/hypotension (Pulmonary Embolism, Pneumothorax, INCLUSION CRITERIA Myocarditis, Tamponade, etc.) Active Bleeding Acute Myocardial Infarction: STEMI or NSTEMI Recent major surgery Ischemic Symptoms Mechanical Complications of AMI EKG and/or biomarker evidence of AMI (STEMI or NSTEMI) Cardiogenic Shock Known left ventricular thrombus Hypotension (<90/60) or the need for vasopressors or inotropes to maintain systolic Patient who did not receive revascularization blood pressure >90 Contraindication to intravenous systemic anticoagulation Evidence of end organ hypoperfusion (cool extremities, oliguria, lactic acidosis) Mechanical aortic valve ACCESS & HEMODYNAMIC SUPPORT Obtain femoral arterial access (via direct visualization with use of ultrasound and fluoro) Obtain venous access (Femoral or Internal Jugular) ACTIVATE CATH LAB Obtain either Fick calculated cardiac index or LVEDP IF LVEDP >15 or Cardiac Index < 2.2 AND anatomy suitable, place IMPELLA Coronary Angiography & PCI Attempt to provide TIMI III flow in all major epicardial vessels other than CTO If unable to obtain TIMI III flow, consider administration of intra-coronary ** QUALITY MEASURES ** vasodilators Impella Pre-PCI Door to Support Time Perform Post-PCI Hemodynamic Calculations < 90 minutes 1. Cardiac Power Output (CPO): MAP x CO Establish TIMI III Flow 451 Right Heart Cath 2. Pulmonary Artery Pulsatility Index (PAPI): sPAP – dPAP Wean off Vasopressors & RA Inotropes Maintain CPO >0.6 Watts Wean OFF Vasopressors and Inotropes Improve survival to If CPO is >0.6 and PAPI >0.9, operators should wean vasopressors and inotropes and determine if Impella can be weaned and removed in the Cath Lab or left in place with transfer to ICU. -

What Is Sepsis?
What is sepsis? Sepsis is a serious medical condition resulting from an infection. As part of the body’s inflammatory response to fight infection, chemicals are released into the bloodstream. These chemicals can cause blood vessels to leak and clot, meaning organs like the kidneys, lung, and heart will not get enough oxygen. The blood clots can also decrease blood flow to the legs and arms leading to gangrene. There are three stages of sepsis: sepsis, severe sepsis, and ultimately septic shock. In the United States, there are more than one million cases with more than 258,000 deaths per year. More people die from sepsis each year than the combined deaths from prostate cancer, breast cancer, and HIV. More than 50 percent of people who develop the most severe form—septic shock—die. Septic shock is a life-threatening condition that happens when your blood pressure drops to a dangerously low level after an infection. Who is at risk? Anyone can get sepsis, but the elderly, infants, and people with weakened immune systems or chronic illnesses are most at risk. People in healthcare settings after surgery or with invasive central intravenous lines and urinary catheters are also at risk. Any type of infection can lead to sepsis, but sepsis is most often associated with pneumonia, abdominal infections, or kidney infections. What are signs and symptoms of sepsis? The initial symptoms of the first stage of sepsis are: A temperature greater than 101°F or less than 96.8°F A rapid heart rate faster than 90 beats per minute A rapid respiratory rate faster than 20 breaths per minute A change in mental status Additional symptoms may include: • Shivering, paleness, or shortness of breath • Confusion or difficulty waking up • Extreme pain (described as “worst pain ever”) Two or more of the symptoms suggest that someone is becoming septic and needs immediate medical attention. -

Update on Volume Resuscitation Hypovolemia and Hemorrhage Distribution of Body Fluids Hemorrhage and Hypovolemia
11/7/2015 HYPOVOLEMIA AND HEMORRHAGE • HUMAN CIRCULATORY SYSTEM OPERATES UPDATE ON VOLUME WITH A SMALL VOLUME AND A VERY EFFICIENT VOLUME RESPONSIVE PUMP. RESUSCITATION • HOWEVER THIS PUMP FAILS QUICKLY WITH VOLUME LOSS AND IT CAN BE FATAL WITH JUST 35 TO 40% LOSS OF BLOOD VOLUME. HEMORRHAGE AND DISTRIBUTION OF BODY FLUIDS HYPOVOLEMIA • TOTAL BODY FLUID ACCOUNTS FOR 60% OF LEAN BODY WT IN MALES AND 50% IN FEMALES. • BLOOD REPRESENTS ONLY 11-12 % OF TOTAL BODY FLUID. CLINICAL MANIFESTATIONS OF HYPOVOLEMIA • SUPINE TACHYCARDIA PR >100 BPM • SUPINE HYPOTENSION <95 MMHG • POSTURAL PULSE INCREMENT: INCREASE IN PR >30 BPM • POSTURAL HYPOTENSION: DECREASE IN SBP >20 MMHG • POSTURAL CHANGES ARE UNCOMMON WHEN BLOOD LOSS IS <630 ML. 1 11/7/2015 INFLUENCE OF ACUTE HEMORRHAGE AND FLUID RESUSCITATION ON BLOOD VOLUME AND HCT • COMPARED TO OTHERS, POSTURAL PULSE INCREMENT IS A SENSITIVE AND SPECIFIC MARKER OF ACUTE BLOOD LOSS. • CHANGES IN HEMATOCRIT SHOWS POOR CORRELATION WITH BLOOD VOL DEFICITS AS WITH ACUTE BLOOD LOSS THERE IS A PROPORTIONAL LOSS OF PLASMA AND ERYTHROCYTES. MARKERS FOR VOLUME CHEMICAL MARKERS OF RESUSCITATION HYPOVOLEMIA • CVP AND PCWP USED BUT EXPERIMENTAL STUDIES HAVE SHOWN A POOR CORRELATION BETWEEN CARDIAC FILLING PRESSURES AND VENTRICULAR EDV OR CIRCULATING BLOOD VOLUME. Classification System for Acute Blood Loss • MORTALITY RATE IN CRITICALLY ILL PATIENTS Class I: Loss of <15% Blood volume IS NOT ONLY RELATED TO THE INITIAL Compensated by transcapillary refill volume LACTATE LEVEL BUT ALSO THE RATE OF Resuscitation not necessary DECLINE IN LACTATE LEVELS AFTER THE TREATMENT IS INITIATED ( LACTATE CLEARANCE ). Class II: Loss of 15-30% blood volume Compensated by systemic vasoconstriction 2 11/7/2015 Classification System for Acute Blood FLUID CHALLENGES Loss Cont. -
Recognizing and Treating Shock in the Prehospital Setting
9/3/2020 Recognizing and Treating Shock in the Prehospital Setting 1 9/3/2020 Special Thanks to Our Sponsor 2 9/3/2020 Your Presenters Dr. Raymond L. Fowler, Dr. Melanie J. Lippmann, MD, FACEP, FAEMS MD FACEP James M. Atkins MD Distinguished Professor Associate Professor of Emergency Medicine of Emergency Medical Services, Brown University Chief of the Division of EMS Alpert Medical School Department of Emergency Medicine Attending Physician University of Texas Rhode Island Hospital and The Miriam Hospital Southwestern Medical Center Providence, RI Dallas, TX 3 9/3/2020 Scenario SHOCK INDEX?? Pulse ÷ Systolic 4 9/3/2020 What is Shock? Shock is a progressive state of cellular hypoperfusion in which insufficient oxygen is available to meet tissue demands It is key to understand that when shock occurs, the body is in distress. The shock response is mounted by the body to attempt to maintain systolic blood pressure and brain perfusion during times of physiologic distress. This shock response can accompany a broad spectrum of clinical conditions that stress the body, ranging from heart attacks, to major infections, to allergic reactions. 5 9/3/2020 Causes of Shock Shock may be caused when oxygen intake, absorption, or delivery fails, or when the cells are unable to take up and use the delivered oxygen to generate sufficient energy to carry out cellular functions. 6 9/3/2020 Causes of Shock Hypovolemic Shock Distributive Shock Inadequate circulating fluid leads A precipitous increase in vascular to a diminished cardiac output, capacity as blood vessels dilate and which results in an inadequate the capillaries leak fluid, translates into delivery of oxygen to the too little peripheral vascular resistance tissues and cells and a decrease in preload, which in turn reduces cardiac output 7 9/3/2020 Causes of Shock Cardiogenic Shock Obstructive Shock The heart is unable to circulate Obstruction to the forward flow of sufficient blood to meet the blood exists in the great vessels metabolic needs of the body. -

Cardiac Shock-Wave Therapy in the Treatment of Coronary Artery Disease
Burneikaitė et al. Cardiovascular Ultrasound (2017) 15:11 DOI 10.1186/s12947-017-0102-y REVIEW Open Access Cardiac shock-wave therapy in the treatment of coronary artery disease: systematic review and meta-analysis Greta Burneikaitė1,2,7*, Evgeny Shkolnik3,4, Jelena Čelutkienė1,2*, Gitana Zuozienė1,2, Irena Butkuvienė1,2, Birutė Petrauskienė1,2, Pranas Šerpytis1,2, Aleksandras Laucevičius1,5 and Amir Lerman6 Abstract Aim: To systematically review currently available cardiac shock-wave therapy (CSWT) studies in humans and perform meta-analysis regarding anti-anginal efficacy of CSWT. Methods: The Cochrane Controlled Trials Register, Medline, Medscape, Research Gate, Science Direct, and Web of Science databases were explored. In total 39 studies evaluating the efficacy of CSWT in patients with stable angina were identified including single arm, non- and randomized trials. Information on study design, subject’s characteristics, clinical data and endpoints were obtained. Assessment of publication risk of bias was performed and heterogeneity across the studies was calculated by using random effects model. Results: Totally, 1189 patients were included in 39 reviewed studies, with 1006 patients treated with CSWT. The largest patient sample of single arm study consisted of 111 patients. All selected studies demonstrated significant improvement in subjective measures of angina symptoms and/or quality of life, in the majority of studies left ventricular function and myocardial perfusion improved. In 12 controlled studies with 483 patients included (183 controls) angina class, Seattle Angina Questionnaire (SAQ) score, nitrates consumption were significantly improved after the treatment. In 593 participants across 22 studies the exercise capacity was significantly improved after CSWT, as compared with the baseline values (in meta-analysis standardized mean difference SMD = −0.74; 95% CI, −0.97 to −0.5; p < 0.001). -
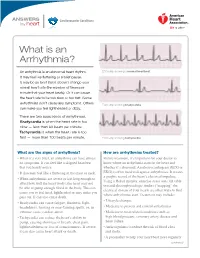
What Is an Arrhythmia?
ANSWERS Cardiovascular Conditions by heart What is an Arrhythmia? An arrhythmia is an abnormal heart rhythm. ECG strip showing a normal heartbeat It may feel like fluttering or a brief pause. It may be so brief that it doesn’t change your overall heart rate (the number of times per minute that your heart beats). Or it can cause the heart rate to be too slow or too fast. Some arrhythmias don’t cause any symptoms. Others ECG strip showing bradycardia can make you feel lightheaded or dizzy. There are two basic kinds of arrhythmias. Bradycardia is when the heart rate is too slow — less than 60 beats per minute. Tachycardia is when the heart rate is too fast — more than 100 beats per minute. ECG strip showing tachycardia What are the signs of arrhythmia? How are arrhythmias treated? • When it’s very brief, an arrhythmia can have almost Before treatment, it’s important for your doctor to no symptoms. It can feel like a skipped heartbeat know where an arrhythmia starts in the heart and that you barely notice. whether it’s abnormal. An electrocardiogram (ECG or • It also may feel like a fluttering in the chest or neck. EKG) is often used to diagnose arrhythmias. It creates a graphic record of the heart’s electrical impulses. • When arrhythmias are severe or last long enough to Using a Holter monitor, exercise stress tests, tilt table affect how well the heart works, the heart may not test and electrophysiologic studies (“mapping” the be able to pump enough blood to the body. -

Distributive Shock
ASK THE EXPERT h EMERGENCY MEDICINE/CRITICAL CARE h PEER REVIEWED Distributive Shock Garret E. Pachtinger, VMD, DACVECC VETgirl; Veterinary Specialty and Emergency Center Levittown, Pennsylvania Clinical Clues YOU HAVE ASKED ... Distributive shock is generally associ- What is distributive shock, and ated with altered vasomotor tone— notably inappropriate vasodilation (eg, how do I treat it? sepsis, systemic inflammatory response syndrome), excessive vasoconstriction THE EXPERT SAYS ... (eg, following trauma or anaphylaxis), or abnormalities in normal blood flow Shock (ie, inadequate cellular energy (eg, obstructive diseases such as gastric production or the body’s inability to dilatation-volvulus [GDV] or pericardial supply cells and tissues with oxygen and effusion)—resulting in maldistribution nutrients and remove waste products1-3) of blood flow. can cause quick clinical deterioration and requires rapid identification and Patients with septic distributive shock treatment. Distributive shock is a gen- often have hyperemic mucous mem- eral classification for syndromes that branes caused by uncontrolled vasodila- cause massive maldistribution of blood tion from inflammatory mediators and flow (seeReferences , page 96). Anaphy- cytokine release (see References, page lactic, obstructive, and septic shock are 96). Patients with anaphylactic or GDV = gastric dilatation- common forms of distributive shock. obstructive distributive shock show volvulus October 2016 cliniciansbrief.com 93 ASK THE EXPERT h EMERGENCY MEDICINE/CRITICAL CARE h PEER -

Septic Shock: Recognition and Initial Management
DATE: January 2017 TEXAS CHILDREN’S HOSPITAL EVIDENCE-BASED OUTCOMES CENTER RECOGNITION AND INITIAL MANAGEMENT OF SEPTIC SHOCK Evidence-Based Guideline (7,8) Definition: Shock is a complex clinical syndrome caused by Table 2. PALS Adjusted Vital Signs for Septic Shock an acute failure of circulatory function, with inadequate tissue Age Heart Rate Resp Rate Systolic BP Temp (°C) and organ perfusion, where delivery of oxygen and substrates 0d - 1m > 205 > 60 < 60 <36 or >38 to body tissues, as well as removal of metabolic waste > 1m - 3m > 205 > 60 < 70 <36 or >38 products are insufficient. (1) Sepsis is defined as abnormal temperature or leukocyte count, in addition to other abnormal > 3m - 1y > 190 > 60 < 70 <36 or >38.5 vital signs, in the presence of proven or known invasive > 1y - 2y > 190 > 40 < 70 + (age in yr x 2) <36 or >38.5 infection. Severe sepsis is defined as sepsis in combination > 2y - 4y > 140 > 40 < 70 + (age in yr x 2) <36 or >38.5 with either cardiovascular organ dysfunction or acute > 4y - 6y > 140 > 34 < 70 + (age in yr x 2) <36 or >38.5 respiratory distress. This condition may also exist when sepsis > 6y - 10y > 140 > 30 < 70 + (age in yr x 2) <36 or >38.5 is combined with two or more other organ dysfunctions, including neurologic, renal, hepatic or hematologic systems. In > 10y - 13y > 100 > 30 < 90 <36 or >38.5 children, septic shock is defined as proven or suspected > 13y > 100 > 16 < 90 <36 or >38.5 infection with the presence of tachycardia and poor perfusion with or without hypotension. -

Sepsis ACP 2019
Sepsis ACP 2019 • Are sepsis bundles good for patient care? • Politics • CMS requirements • New York’s Rory Staunton Law • Industry involvement Controversial • Is the science sound? • Emergency room physician petition to retire guidelines • More than 5800 ER physicians signed petition Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016 Critical Care Medicine 2017. 45(3):486 • Initial Resuscitation. • At least 30 mL/Kg of IV crystalloid fluid within first 3 hours • After initial resuscitation, additional fluids guided by frequent reassessment • MAP >65 mm Hg • Guiding resuscitation to normalize lactate in patients with elevated lactate levels as a marker of tissue hypoperfusion. • Appropriate routine microbiologic cultures before starting antimicrobial therapy and within one hour. • Empiric coverage for all likely pathogens • Combination therapy for initial management of septic shock • Procalcitonin levels to support shortening duration of therapy. Sepsis Guidelines Continued: • Source control intervention be implemented as soon as medically and logistically practical. • Fluid therapy. • Fluid challenge technique with continued fluid administration as long as hemodynamics factors continue to improve. • Vasopressors. • Norepinephrine as the first-choose vasopressor • Adding vasopressin 0.03 U/min or epinephrine. • Recommend against IV hydrocortisone if adequate fluid resuscitation and vasopressor are able to restore hemodynamics stability. Sepsis Guidelines Continued • Transfusion only when -

Pediatric Hypovolemic Shock Michael J
Send Orders of Reprints at [email protected] 10 The Open Pediatric Medicine Journal, 2013, 7, (Suppl 1: M3) 10-15 Open Access Pediatric Hypovolemic Shock Michael J. Hobson1,2 and Ranjit S. Chima*,1,2 1Division of Critical Care Medicine, Cincinnati Children's Hospital Medical Center, Cincinnati, Ohio, USA 2Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati Children's Hospital Medical Center, Cincinnati, Ohio, USA Abstract: Hypovolemic shock is a common yet underappreciated insult which often accompanies illnesses afflicting children. Indeed, it is by far the most common type of shock in the pediatric age group worldwide. Early recognition and treatment of hypovolemic shock is paramount to reversing cellular hypoxia and ischemia before irreparable end-organ damage ensues. Keywords: Hypovolemic shock, dehydration, hemorrhage. INTRODUCTION for the administration of diluted juices or formula which may put the patient at risk for hyponatremia. Hypernatremia Hypovolemic shock is a common yet underappreciated results from an excessive loss of free water relative to insult which often accompanies illnesses afflicting children. sodium; the reverse is true in the case of hyponatremic Early recognition and treatment of shock is paramount to dehydration. The causes of dehydration and hypovolemic reversing cellular hypoxia and ischemia before irreparable shock in children are numerous (Table 2), but can be broadly end-organ damage ensues. Described over 150 years ago, defined by either decreased intake of fluid, excessive hypovolemic shock remains the most common etiology of gastrointestinal losses, excessive urinary losses, or shock affecting children today. Diarrheal illnesses resulting translocation of body fluid from the intravascular in dehydration account alone for approximately 30% of compartment. -

Surviving Sepsis Campaign Hour 1 Bundle
Hour-1 Bundle Initial Resuscitation for Sepsis and Septic Shock 3 5 ! Administer broad- Apply vasopressors if MEDICAL spectrum antibiotics. hypotensive during or EMERGENCY after fluid resuscitation to maintain a mean arterial Initiate bundle upon 4 pressure ≥ 65 mm Hg. recognition of sepsis/septic shock. Begin rapid May not complete all bundle elements administration of within one hour of recognition. 30 mL/kg crystalloid for hypotension or lactate ≥ 4 mmol/L. 1 68 Measure lactate level. 100/50 96 Remeasure lactate 14 if initial lactate elevated (> 2 mmol/L). 2 Obtain blood cultures before administering antibiotics. Bundle: SurvivingSepsis.org/Bundle Complete Guidelines: SurvivingSepsis.org/Guidelines © 2019 the Society of Critical Care Medicine and the European Society of Intensive Care Medicine. All Rights Reserved. BUNDLE HOUR-1 BUNDLE: INITIAL RESUSCITATION FOR SEPSIS AND SEPTIC SHOCK: 1) Measure lactate level.* 2) Obtain blood cultures before administering antibiotics. 3) Administer broad-spectrum antibiotics. 4) Begin rapid administration of 30mL/kg crystalloid for hypotension or lactate ≥4 mmol/L. 5) Apply vasopressors if hypotensive during or after fluid resuscitation to maintain a mean arterial pressure ≥ 65 mm Hg. *Remeasure lactate if initial lactate elevated (> 2 mmol/L). © 2019 the Society of Critical Care Medicine and the European survivingsepsis.org Society of Intensive Care Medicine. All Rights Reserved. 1. *Act quickly upon sepsis & septic shock recognition 2. Minimize time to treatment - sepsis & septic shock are medical emergencies 3. Monitor closely for response to interventions 4. Communicate sepsis status in hand-offs *All elements of the Hour-1 bundle may or may not be completed in the first hour after sepsis recognition survivingsepsis.org BUNDLE HOUR-1 BUNDLE: INITIAL RESUSCITATION FOR SEPSIS AND SEPTIC SHOCK: 1) Measure lactate level.* 2) Obtain blood cultures before administering antibiotics. -

Lynn Fitzgerald Macksey
SHOCK STATES Lynn Fitzgerald Macksey RN, MSN, CRNA Define SHOCK : a state where tissue perfusion to vital organs is inadequate. Shock state In all shock states, the ultimate result is inadequate tissue perfusion, leading to a decreased delivery of oxygen and nutrients to cells…. and, therefore, cell energy. Clinical recognition of shock Symptoms dizziness, nausea, visual changes, thirst, dyspnea Signs cold clammy skin, pallor, confusion, agitation, diaphoresis, weak thready pulse, obvious injury Compensatory stages of shock Sympathetic nervous system Renin-angiotensin system Pituitary-antidiuretic hormone release Shunting from less critical areas to brain and heart Progressive decompensation Failure of compensatory mechanisms in Bowel CNS & autonomic Heart Kidneys Lungs Liver What will we see? Shock diagnosis Clinical examination Diagnostics: CXR CBC blood chemistry EKG ABG vital signs Monitoring organ perfusion in shock states Base deficit Blood lactate levels Normalization of these markers are the end point goals of resuscitation! Base Deficit Reflects severity of shock, the oxygen debt, changes in oxygen delivery, and the adequacy of fluid resuscitation. 2-5 mmol/L suggests mild shock 6-14 mmol/L indicates moderate shock > 14 mmol/L is a sign of severe shock Base Deficit The base deficit reflects the likelihood of multiple organ failure and survival. An admission base deficit in excess of 5-8 mmol/L correlates with increased mortality. Lactate Levels Blood lactate levels correlate with other signs of hypoperfusion. Normal lactate levels are 0.5-1.5 mmol/L >5 mmol/L indicate significant lactic acidosis. Lactate Levels Failure to clear lactate within 24 hours after circulatory shock is a predictor of increased mortality.