VT Sourcebook 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1,011 Candidates and Elected Officials from All 50 States Have Signed the Pledge to Achieve America's Goals. Sign the Pledg
9/14/2020 Pledge — Future Now Start a Giving Circle Policy Work Donate About 1,011 candidates and elected officials from all 50 states have signed the Pledge to Achieve America’s Goals. Sign the pledge ↓ Rep. Kim Abbott MT House Elizabeth Alcorn VA House Rep. Jeramey Anderson MS District 83 District 58 House District 110 Rep. Chris Abernathy ID House Rep. Kelly Alexander NC House Rep. Marti Anderson IA House District 29A District 107 District 36 Rep. Gale Adcock NC House Rep. Terry Alexander SC House Rep. Richard Andrade AZ District 41 District 59 House District 29 Rep. John Ager* NC House Jenn Alford-Teaster NH Senate Anton Andrew PA House District 115 District 8 District 160 Sen. Irene Aguilar* CO Senate Sen. Denise Harper Angel KY Christian Andrews IA House District 32 Senate District 35 District 95 Del. Lashrecse Aird* VA House Rep. Richard Ames* NH House Joey Andrews MI House District District 63 Cheshire 9 79 Sen. Raumesh Akbari TN Rep. Carol Ammons IL House Naomi Andrews NH House Senate District 29 District 103 Rockingham 5 Rep. James Albis* CT House Rep. Mike Amyx KS House Senah Andrews NC House District 99 District 45 District 83 https://givingcircles.futurenow.org/pledge 1/18 9/14/2020 Pledge — Future Now Barb Anness MI House District Rep. Christy Bartlett NH House Rep. Barbara Bessette MT Start 4a5 Giving Circle Policy Work Merrimack 19 House District 24 Donate About Rep. Sarah Anthony MI House Rep. Sydney Batch NC House Sen. Alessandra Biaggi NY District 68 District 37 Senate District 34 Rep. -

Transmittal Email to House and Senate Members
Sent: Monday, March 5, 2018 1:47 PM To: David Ainsworth; Robert Bancroft; John Bartholomew; Fred Baser; Lynn Batchelor; Scott Beck; Paul Belaski; Steve Beyor; Clem Bissonnette; Thomas Bock; Bill Botzow; Patrick Brennan; Tim Briglin; Cynthia Browning; Jessica Brumsted; Susan Buckholz; Tom Burditt; Mollie Burke; William Canfield; Stephen Carr; Robin Chesnut-Tangerman; Annmarie Christensen; Kevin Christie; Brian Cina; Selene Colburn; Jim Condon; Peter Conlon; Daniel Connor; Chip Conquest; Sarah CopelandHanzas; Timothy Corcoran; Larry Cupoli; Maureen Dakin; David Deen; Dennis Devereux; Eileen Dickinson; Anne Donahue; Johannah Donovan; Betsy Dunn; Alyson Eastman; Alice Emmons; Peter Fagan; Rachael Fields; Robert Forguites; Robert Frenier; Douglas Gage; Marianna Gamache; John Gannon; Marcia Gardner; Dylan Giambatista; Diana Gonzalez; Maxine Grad; Rodney Graham; Adam Greshin; Sandy Haas; James Harrison; Mike Hebert; Robert Helm; Mark Higley; Matthew Hill; Mary Hooper; Jay Hooper; Lori Houghton; Mary Howard; Ronald Hubert; Kimberly Jessup; Ben Jickling; Mitzi Johnson; Ben Joseph; Bernie Juskiewicz; Brian Keefe; Kathleen Keenan; Charlie Kimbell; Warren Kitzmiller; Jill Krowinski; Rob LaClair; Martin LaLonde; Diane Lanpher; Richard Lawrence; Paul Lefebvre; Patti Lewis; William Lippert; Emily Long; Gabrielle Lucke; Terence Macaig; Michael Marcotte; Marcia Martel; Jim Masland; Christopher Mattos; Curt McCormack; Patricia McCoy; Francis McFaun; Alice Miller; Kiah Morris; Mary Morrissey; Mike Mrowicki; Barbara Murphy; Linda Myers; Gary Nolan; Terry -

2018 New Member Orientation November 26 – 27, 2018
2018 New Member Orientation November 26 – 27, 2018 Monday, November 26, 2018 *All events are in the State House unless noted* Throughout the day Slide Show: The Legislature Cafeteria Lounge 7:15 a.m. – 9:00 a.m. Registration, Payroll, Expenses, Benefits, Photographs, and Room: 10/Room: 11 iPad Distribution and Training 7:30 a.m. – 10:00 a.m. Breakfast [PLEASE register first] Cafeteria - sidebar Open Cafeteria Account (if desired) 9:15 a.m. – 9:25 a.m. Welcome and Introduction Room 11 Mark Snelling, President, Snelling Center for Government 9:25 a.m. – 10:10 a.m. The Legislative Process Senate Chamber, or New House and Senate Members go to their respective chambers House Chamber to discuss parliamentary procedures, reporting and debate of bills, the amendment process, recording and notice of proceedings in Calendars and Journals, and legislative decorum John Bloomer, Secretary of the Senate William MaGill, Clerk of the House 10:10 a.m. – 10:20 a.m. Transition to Room 11 on 1st Floor 10:20 a.m. – 10:50 a.m. Overview of the Office of Legislative Council Room 11 Luke Martland, Director and Chief Legislative Counsel 10:50 a.m. – 12:20 p.m. Drafting Bills, Committee Hearings, and the Role of Location to be determined Legislative Council Discussion of the drafting process, bill introduction, the legislative committee process, and the role of the Office VT LEG #319211 v.1A 2018 New Member Orientation Page 2 of 6 Monday, November 26, 2018 continued 12:20 p.m. – 12:30 p.m. Transition to State House Cafeteria on 2nd floor 12:30 p.m. -

Forum: a Child of an Era of Fear
Sent: Tuesday, March 20, 2018 11:20 AM To: Maxine Grad Subject: Bob Williamson shares Hailey Napier's powerful letter from the VALLEY NEWS Dear Chair Maxine Grad, Below is Hailey Napier’s letter from the VALLEY NEWS. Hailey eloquently expresses how today’s youngsters feel when mass shootings occur and lawmakers do little to address the lethal problem. Best, Bob Williamson…And here’s the letter: http://www.vnews.com/ Forum: A Child of an Era of Fear When I was 12 years old, I began scanning for exits at every movie theater I went to and carefully thought through escape scenarios as the previews played. I assessed the space between the seats and the floor. Would I be able to crawl between the armrest and the wall unseen? That was the year of the Aurora shooting. If you don’t remember the details, 12 people were murdered in a Century 16 theater in Aurora, Colo.. They were watching The Dark Knight Rises. I had begged to see the movie myself, and as I read the headlines online, I realized that innocent people had died, and that I could easily have been one of them. I am a child of an era of fear. Born almost exactly a year after Columbine, I grew up with the pitch black, unspoken terror of lockdown drills. Hiding in corners and closets and behind desks, as if turning the lights off will convince a killer that school’s been canceled on a Tuesday in May; as if a bookshelf will protect me from the rain of bullets driven by some arbitrary vendetta against society. -

Draft House Human Services Letter to Dept Of
115 STATE STREET REP. ANN PUGH, CHAIR MONTPELIER, VT 05633 REP. SANDY HAAS, VICE CHAIR TEL: (802) 828-2228 REP. FRANCIS MCFAUN, RANKING MEMBER FAX: (802) 828-2424 REP. THERESA WOOD, CLERK REP. JESSICA BRUMSTED REP. JAMES GREGOIRE REP. LOGAN NICOLL REP. DANIEL NOYES REP. KELLY PAJALA REP. MARYBETH REDMOND STATE OF VERMONT REP. CARL ROSENQUIST GENERAL ASSEMBLY HOUSE COMMITTEE ON HUMAN SERVICES April 20, 2020 Ken Schatz, Commissioner Department for Children and Families 280 State Drive, HC 1 North Waterbury, VT 05671-1080 Dear Commissioner Schatz, As you know, the House Committee on Human Services has spent considerable time in the last few weeks taking testimony and engaging in discussions regarding compliance with parent-child contact orders regarding children in need of care or supervision during the current declared state of emergency. The Committee understands the tremendous pressure you and your staff are under and the extraordinary steps you are taking to see that children who are in the custody of DCF are safe and well- cared for during the COVID-19 outbreak. While our committee believes that the safest approach for everyone during the state of emergency is to replace in-person contact with remote or virtual visits as recommended by Vermont Department of Health Commissioner Levine on March 25, 2020, we understand there may be some instances, taken on a case-by-case basis, where in-person contact may critical to staying on the path to family reunification and can be effectuated in a safe manner. To this end, we ask that DCF use the Vermont Department of Health’s most recent guidance regarding COVID-19 best practices to develop specific written guidance for DCF staff, foster parents, natural parents, and others who may participate in or facilitate in-person parent-child contact during the declared state of emergency. -
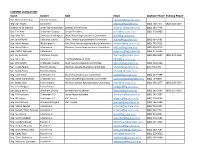
Refer to This List for Area Legislators and Candidates
CURRENT LEGISLATORS Name District Role Email Daytime Phone Evening Phone Sen. Richard Westman Lamoille County [email protected] Rep. Dan Noyes Lamoille-2 [email protected] (802) 730-7171 (802) 644-2297 Speaker Mitzi Johnson Grand Isle-Chittenden Speaker of the House [email protected] (802) 363-4448 Sen. Tim Ashe Chittenden County Senate President [email protected] (802) 318-0903 Rep. Kitty Toll Caledona-Washington Chair, House Appropriations Committee [email protected] Sen. Jane Kitchel Caledonia County Chair, Senate Appropriations Committee [email protected] (802) 684-3482 Rep. Mary Hooper Washington-4 Vice Chair, House Appropriations Committee [email protected] (802) 793-9512 Rep. Marty Feltus Caledonia-4 Member, House Appropriations Committee [email protected] (802) 626-9516 Rep. Patrick Seymour Caledonia-4 [email protected] (802) 274-5000 Sen. Joe Benning Caledonia County [email protected] (802) 626-3600 (802) 274-1346 Rep. Matt Hill Lamoille 2 *NOT RUNNING IN 2020 [email protected] Sen. Phil Baruth Chittenden County Chair, Senate Education Committee [email protected] (802) 503-5266 Sen. Corey Parent Franklin County Member, Senate Education Committee [email protected] 802-370-0494 Sen. Randy Brock Franklin County [email protected] Rep. Kate Webb Chittenden 5-1 Chair, House Education Committee [email protected] (802) 233-7798 Rep. Dylan Giambatista Chittenden 8-2 House Leadership/Education Committee [email protected] (802) 734-8841 Sen. Bobby Starr Essex-Orleans Member, Senate Appropriations Committee [email protected] (802) 988-2877 (802) 309-3354 Sen. -

APPENDIX a Members, Officers and Standing Committees of the House of Representatives 2017 Biennial Session Prepared by William M
APPENDIX A Members, Officers and Standing Committees of the House of Representatives 2017 Biennial Session Prepared by William M. MaGill, Clerk of the House _____________________ MEMBERS OF THE HOUSE Mitzi Johnson, Speaker South Hero, VT William M. MaGill, Clerk of the House Waitsfield, VT Representatives Town Committee Seat Ainsworth, David M. Royalton Natural Resources, Fish & Wildlife 78 Ancel, Janet Calais Ways and Means 135 Bancroft, Robert L. Westford Transportation 98 Bartholomew, John L. Hartland Agriculture & Forestry 86 Baser, Fred K. Bristol Ways and Means 11 Batchelor, Lynn D. Derby Corrections and Institutions 35 Beck, Scott L. St. Johnsbury Education 118 Belaski, Paul S. Windsor Corrections and Institutions 16 Beyor, Stephen C. Highgate Natural Resources, Fish & Wildlife 104 Bissonnette, Clement J. Winooski Transportation 39 Bock, Thomas A. Chester Agriculture & Forestry 42 Botzow II, William G. Pownal Commerce and Economic Development 147 Brennan, Patrick M. Colchester Transportation 76 Briglin, Timothy C. Thetford Health Care 93 Browning, Cynthia M. Arlington Ways and Means 67 Brumsted, Jessica C. Shelburne Government Operations 46 Buckholz, Susan M. Hartford Agriculture & Forestry 28 Burditt, Thomas B. West Rutland Judiciary 115 Burke, Mollie S. Brattleboro Transportation 24 Canfield, William P. Fair Haven Ways and Means 71 Carr, Stephen A. Brandon Energy and Technology 23 Chesnut-Tangerman, Middletown Springs Energy and Technology 52 Robin J. Christensen, Annmarie Weathersfield Health Care 49 Christie, Kevin B. Hartford General, Housing and Military Affairs 10 Cina, Brian J. Burlington Health Care 88 Colburn, Selene Burlington Judiciary 51 Condon, James O. Colchester Ways and Means 69 Conlon, Peter C. Cornwall Education 80 Connor, Daniel F. -

HOUSE COMMITTEES 2019 - 2020 Legislative Session
HOUSE COMMITTEES 2019 - 2020 Legislative Session Agriculture & Forestry Education Health Care Rep. Carolyn W. Partridge, Chair Rep. Kathryn Webb, Chair Rep. William J. Lippert Jr., Chair Rep. Rodney Graham, Vice Chair Rep. Lawrence Cupoli, Vice Chair Rep. Anne B. Donahue, Vice Chair Rep. John L. Bartholomew, Ranking Mbr Rep. Peter Conlon, Ranking Member Rep. Lori Houghton, Ranking Member Rep. Thomas Bock Rep. Sarita Austin Rep. Annmarie Christensen Rep. Charen Fegard Rep. Lynn Batchelor Rep. Brian Cina Rep. Terry Norris Rep. Caleb Elder Rep. Mari Cordes Rep. John O'Brien Rep. Dylan Giambatista Rep. David Durfee Rep. Vicki Strong Rep. Kathleen James Rep. Benjamin Jickling Rep. Philip Jay Hooper Rep. Woodman Page Appropriations Rep. Christopher Mattos Rep. Lucy Rogers Rep. Catherine Toll, Chair Rep. Casey Toof Rep. Brian Smith Rep. Mary S. Hooper, Vice Chair Rep. Peter J. Fagan, Ranking Member Energy & Technology Human Services Rep. Charles Conquest Rep. Timothy Briglin, Chair Rep. Ann Pugh, Chair Rep. Martha Feltus Rep. Laura Sibilia, Vice Chair Rep. Sandy Haas, Vice Chair Rep. Robert Helm Rep. Robin Chesnut-Tangerman, Rep. Francis McFaun, Ranking Member Rep. Diane Lanpher Ranking Member Rep. Jessica Brumsted Rep. Linda K. Myers Rep. R. Scott Campbell Rep. James Gregoire Rep. Maida Townsend Rep. Seth Chase Rep. Logan Nicoll Rep. Matthew Trieber Rep. Mark Higley Rep. Daniel Noyes Rep. David Yacovone Rep. Avram Patt Rep. Kelly Pajala Rep. Heidi E. Scheuermann Rep. Marybeth Redmond Commerce & Rep. Michael Yantachka Rep. Carl Rosenquist Rep. Theresa Wood Economic Development General, Housing, & Military Affairs Rep. Michael Marcotte, Chair Judiciary Rep. Thomas Stevens, Chair Rep. Jean O'Sullivan, Vice Chair Rep. -

Alexandria Ocasio-Cortez People Power Meme Co-Op 9/17/18, 7�19 AM
Alexandria Ocasio-Cortez People Power Meme Co-Op 9/17/18, 719 AM The names of all 626 Berniecrats who have won primaries so far in 2018! WARREN LYNCH · WEDNESDAY, JUNE 20, 2018 For all ye doubters (especially those working at NPR) who keep saying that the Berniecrats and progressives are “losing” the 2018 primaries! There are 626 names here, and 82 of them in FEDERAL races! The number of seated progressives is about to at least TRIPLE this November, so don’t believe the hype! (updated 9/16/18) The list is now annotated! People have been asking me for ages: “WHY do these people count as Berniecrats?” So now there’s a key, from most left-leaning to most moderate: (DSA) - endorsed by Democratic Socialists of America, the leftist group that Alexandria Ocasio-Cortez is a member of. (even to the left of Bernie!) (Bernie) - endorsed by Bernie personally (LB) - endorsed by Local Berniecrats, a grassroots group with no money that started on the Internet with the goal of making Bernie’s down-ballot dream come true (OR) - endorsed by Our Revolution, either national or a local branch. The organization started by Bernie Sanders. (W) - personally endorsed by me, Warren Lynch. This candidate is a person I know personally, and I vouch for them that they are a progressive. (JD) - endorsed by Justice Democrats, the group run by The Young Turks (PCCC) - endorsed by, or my friend from, Progressive Change Campaign Committee, the progressive group which sent me to DC to learn stuff. Some of their candidates are a bit moderate or not Berniecrats per se, but all are strong bold progressives. -

Current House Journal
Journal of the House of the STATE OF VERMONT BIENNIAL SESSION, 2021 ________________ Wednesday, January 6, 2021 Pursuant to the provisions of the Constitution and Laws of the State of Vermont, the members-elect of the House of Representatives convened in the State House in Montpelier on the first Wednesday after the first Monday, being the sixth day of January, in the year of our Lord, two thousand and twenty-one. At ten o’clock in the forenoon, the Honorable James C. Condos, Secretary of State, called the House to order for the seventy-sixth biennial session. Devotional Exercises Devotional exercises were conducted by The Rt. Rev. Dr. Shannon McVean-Brown, Episcopal Bishop of Vermont, Burlington. Pledge of Allegiance Secretary of State James C. Condos, led the House in the Pledge of Allegiance. ROLL CALL Secretary of State, James C. Condos, called the roll for the seventy-sixth biennial session: Addison-1 Robin Scheu Addison-1 Amy D. Sheldon Addison-2 Peter Conlon Addison-3 Matthew Birong Addison-3 Diane M. Lanpher Addison-4 Mari Cordes Addison-4 Caleb Elder 1 JOURNAL OF THE HOUSE 2 Addison-5 Harvey T. Smith Addison-Rutland Terry E. Norris Bennington-1 Nelson Brownell Bennington-2-1 Timothy R. Corcoran II Bennington-2-1 Dane Whitman Bennington-2-2 Mary A. Morrissey Bennington-2-2 Michael Nigro Bennington-3 David K. Durfee Bennington-4 Seth Bongartz Bennington-4 Kathleen James Bennington-Rutland Linda Joy Sullivan Caledonia-1 Marcia Robinson Martel Caledonia-2 Joseph “Chip” J. Troiano Caledonia-3 Scott L. Beck Caledonia-3 R. -

Bi-State Primary Care Association, January 2020
Vermont 2020January 2020 Primary Care Sourcebook Bi-State Primary Care Association 61 Elm Street, Montpelier, Vermont 05602 (802) 229-0002 www.bistatepca.org TABLE OF CONTENTS Introduction to Bi-State Page 3 Overcoming Transpiration Barriers Page 18 Bi-State PCA Vermont Members Page 4 Helping Patients Experiencing Homelessness Page 19 Key Elements of Bi-State’s Work Page 5 Accessing Nutritious Food Page 19 FQHC’s, AHEC, PPNNE, and VCCU Page 7 Reducing Isolation for Farmworkers Page 20 Member Map Page 8 Other Elements of Comprehensive Care Page 21 Payer Mix Page 9 Vermont Rural Health Alliance (VRHA) Page 24 Bi-States 2019-2020 Vermont Public Policy 1 in 3 Vermonters in over 88 Sites Page 10 Page 27 Principles Investing in Primary Care Page 11 FQHC Funding Page 28 Workforce Development Supports Primary Care Page 13 FQHC and ACO Participation Page 28 Bi-State Workforce Recruitment Center Page 14 FQHC Federal Requirements Page 29 Workforce & Area Health Education Centers (AHEC) Page 15 Member Sites by Organization Page 30 Addressing All the Factors of Wellness Page 17 Member Sites by County Page 31 Legislative Representation List Biennium 2019 – Tracking Social Determinants of Health Page 18 Page 33 2020 2 What is a Primary Care Association? Each of the 50 states (or in Bi-State’s case, a pair of states) has one nonprofit Primary Care Association (PCA) to serve as the voice for Community Health Centers. These health centers were born out of the civil rights and social justice movements of the 1960’s with a clear mission that prevails today: to provide health care to communities with a scarcity of providers and services. -

Rep. Catherine Toll, Chair, House Committee on Appropriations
115 STATE STREET REP. CATHERINE TOLL, CHAIR MONTPELIER, VT 05633 REP. MARY S. HOOPER, VICE CHAIR TEL: (802) 828-2228 FAX: (802) 828-2424 REP. PETER J. FAGAN, RANKING MEMBER REP. CHARLES CONQUEST REP. MARTHA FELTUS REP. ROBERT HELM REP. KIMBERLY JESSUP REP. DIANE LANPHER REP. LINDA K. MYERS STATE OF VERMONT REP. MAIDA TOWNSEND REP. DAVID YACOVONE GENERAL ASSEMBLY House Committee on Appropriations DATE: May 27, 2020 FROM: Rep. Kitty Toll, Chair, House Committee on Appropriations TO: All House Committee Chairs RE: FY 2021 First Phase/Transition Budget Bill as Proposed by the Administration The Administration presented its proposed FY2021 budget for the first quarter, July 1, 2020 through September 30, 2020, to the House Appropriations Committee on Tuesday. This proposal provides the State with a budget to start the fiscal year. The budget for the remaining three- quarters of the fiscal year will be addressed during the months of August and September when we will have more information on State revenues, Federal funds, and the effect that the COVID- 19 epidemic has had on Vermont. The General Assembly has been provided with informal weekly updates on revenues from the Joint Fiscal Office, the latest being Tuesday, May 19. The Official Consensus Revenue Forecast will be presented to the Emergency Board in mid-August for adoption. Until that time, there is no official forecast upon which to base the budget, making the process of developing the FY 2021 budget challenging. The latest informal revenue update can be found in the following links. FY 2020/21/22 Revenues detail can be found at: Revenue Forecast May 19, 2020.