The Allopregnanolone to Progesterone Ratio Across the Menstrual Cycle and in Menopause
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Progestogen Only Pill
The Progestogen Only Pill Mini-pill or POP A service provided by page 2 of 8 How does the progestogen only pill (POP) work? The progestogen only pill mainly works by thickening the mucus you produce from your cervix. This makes it more difficult for sperm to get to the egg. It can also sometimes stop your ovaries from producing an egg (ovulation). How effective is the pill? The effectiveness of the pill depends on the woman taking it. At best it is over 98% effective (when no pills are missed). However failure rates can be much higher (9-15%) if women do not remember to take their pill properly. Missed pills can lead to pregnancy. Advantages of the POP • It doesn’t interfere with sex. • You can use it whilst you are breastfeeding. • It is useful if you cannot take oestrogen (the hormone contained in the combined oral contraceptive) • Can be used at any age even if you smoke and are over 35 years of age. • It may help with premenstrual symptoms and painful periods. page 3 of 8 Disadvantages of the POP • You have to remember to take your pill at the same time every day. • Your periods may become irregular or even stop altogether on the POP, this is not dangerous but if you miss a period you need to check that you are not pregnant by coming to clinic for a pregnancy test. • You may get some temporary side effects, such as spotty skin, breast tenderness and mood changes, though these should stop within a few months. -

Redalyc.Timing of Progesterone and Allopregnanolone Effects in a Serial
Salud Mental ISSN: 0185-3325 [email protected] Instituto Nacional de Psiquiatría Ramón de la Fuente Muñiz México Contreras, Carlos M.; Rodríguez-Landa, Juan Francisco; Bernal-Morales, Blandina; Gutiérrez-García, Ana G.; Saavedra, Margarita Timing of progesterone and allopregnanolone effects in a serial forced swim test Salud Mental, vol. 34, núm. 4, julio-agosto, 2011, pp. 309-314 Instituto Nacional de Psiquiatría Ramón de la Fuente Muñiz Distrito Federal, México Available in: http://www.redalyc.org/articulo.oa?id=58221317003 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Salud Mental 2011;34:309-314Timing of progesterone and allopregnanolone effects in a serial forced swim test Timing of progesterone and allopregnanolone effects in a serial forced swim test Carlos M. Contreras,1,2 Juan Francisco Rodríguez-Landa,1 Blandina Bernal-Morales,1 Ana G. Gutiérrez-García,1,3 Margarita Saavedra1,4 Artículo original SUMMARY Total time in immobility was the highest and remained at similar levels only in the control group throughout the seven sessions of the The forced swim test (FST) is commonly employed to test the potency serial-FST. In the allopregnanolone group a reduction in immobility of drugs to reduce immobility as an indicator of anti-despair. Certainly, was observed beginning 0.5 h after injection and lasted approximately antidepressant drugs reduce the total time of immobility and enlarge 1.5 h. Similarly, progesterone reduced immobility beginning 1.0 h the latency to the first immobility period. -

WHO Statement on Progestogen-Only Implants
WHO statement on Progestogen-only implants Key facts Progestogen-only implants consist of hormone-filled capsules or rods that are inserted under the skin in a woman’s upper arm The purpose of this Statement is to reiterate and Life-Saving Commodities for Women and Children clarify the existing (current) WHO position based on endorsed contraceptive implants as one of its 13 Life- published guidance that is still valid. WHO monitors Saving Commodities. the evidence in this field closely and will update Primary mechanisms of action of the implants include its guidance as and when new evidence becomes thickening cervical mucus (making it difficult for available. sperm to penetrate) and preventing ovulation in KEY FACTS ABOUT PROGESTOGEN-ONLY IMPLANTS about half of menstrual cycles. Long-acting reversible contraceptives, including USE OF PROGESTOGEN-ONLY IMPLANTS BY intrauterine devices and implants are the most WOMEN LIVING WITH HIV effective methods of reversible contraception. These There have been concerns from recent publications methods have multiple advantages over other regarding the effectiveness of progestogen-only reversible methods. Most importantly, once in place, implants among women living with HIV and on they do not require daily or monthly dosing and their some antiretroviral drugs.1 However, compared with duration of contraceptive action ranges from 3 to 5 other hormonal methods, no significant differences years. in pregnancy rates have been observed with Progestogen-only implants consist of hormone-filled progestogen-only implants.2 capsules or rods that are inserted under the skin of a woman’s upper arm. Current systems consist of one or two rods. -

Dose Response Effect of Cyclical Medroxyprogesterone on Blood Pressure in Postmenopausal Women
Journal of Human Hypertension (2001) 15, 313–321 2001 Nature Publishing Group All rights reserved 0950-9240/01 $15.00 www.nature.com/jhh ORIGINAL ARTICLE Dose response effect of cyclical medroxyprogesterone on blood pressure in postmenopausal women PJ Harvey1, D Molloy2, J Upton2 and LM Wing1 Departments of 1Clinical Pharmacology and 2Medicine, Flinders University of South Australia, Bedford Park, Adelaide, South Australia, Australia 5042 Objective: This study was designed to compare with mean values of weeks 3 and 4 of each phase used for placebo the dose-response effect of cyclical doses of analysis. Ambulatory BP was performed in the final the C21 progestogen, medroxyprogesterone acetate week of each phase. (MPA) on blood pressure (BP) when administered to Results: Compared with the placebo phase, end of normotensive postmenopausal women receiving a fixed phase clinic BP was unchanged by any of the proges- mid-range daily dose of conjugated equine oestrogen togen treatments. There was a dose-dependent (CEE). decrease in ambulatory daytime diastolic and mean Materials and methods: Twenty normotensive post- arterial BP with the progestogen treatments compared menopausal women (median age 53 years) participated with placebo (P Ͻ 0.05). in the study which used a double-blind crossover Conclusion: In a regimen of postmenopausal hormone design. There were four randomised treatment phases, replacement therapy with a fixed mid-range daily dose each of 4 weeks duration. The four blinded treatments of CEE combined with a cyclical regimen of a C21 pro- were MPA 2.5 mg, MPA 5 mg, MPA 10 mg and matching gestogen spanning the current clinical dose range, the placebo, taken for the last 14 days of each 28 day treat- progestogen has either no effect or a small dose-depen- ment cycle. -

Combined Estrogen–Progestogen Menopausal Therapy
COMBINED ESTROGEN–PROGESTOGEN MENOPAUSAL THERAPY Combined estrogen–progestogen menopausal therapy was considered by previous IARC Working Groups in 1998 and 2005 (IARC, 1999, 2007). Since that time, new data have become available, these have been incorporated into the Monograph, and taken into consideration in the present evaluation. 1. Exposure Data 1.1.2 Progestogens (a) Chlormadinone acetate Combined estrogen–progestogen meno- Chem. Abstr. Serv. Reg. No.: 302-22-7 pausal therapy involves the co-administration Chem. Abstr. Name: 17-(Acetyloxy)-6-chlo- of an estrogen and a progestogen to peri- or ropregna-4,6-diene-3,20-dione menopausal women. The use of estrogens with IUPAC Systematic Name: 6-Chloro-17-hy- progestogens has been recommended to prevent droxypregna-4,6-diene-3,20-dione, acetate the estrogen-associated risk of endometrial Synonyms: 17α-Acetoxy-6-chloro-4,6- cancer. Evidence from the Women’s Health pregnadiene-3,20-dione; 6-chloro-Δ6-17- Initiative (WHI) of adverse effects from the use acetoxyprogesterone; 6-chloro-Δ6-[17α] of a continuous combined estrogen–progestogen acetoxyprogesterone has affected prescribing. Patterns of exposure Structural and molecular formulae, and relative are also changing rapidly as the use of hormonal molecular mass therapy declines, the indications are restricted, O CH and the duration of the therapy is reduced (IARC, 3 C 2007). CH3 CH3 O C 1.1 Identification of the agents CH3 H O 1.1.1 Estrogens HH For Estrogens, see the Monograph on O Estrogen-only Menopausal Therapy in this Cl volume. C23H29ClO4 Relative molecular mass: 404.9 249 IARC MONOGRAPHS – 100A (b) Cyproterone acetate Structural and molecular formulae, and relative Chem. -

Australian Public Assessment Report for Progesterone
Australian Public Assessment Report for Progesterone Proprietary Product Name: Prometrium / Utrogestan Sponsor: Besins Healthcare Australia Pty Ltd June 2017 Therapeutic Goods Administration About the Therapeutic Goods Administration (TGA) • The Therapeutic Goods Administration (TGA) is part of the Australian Government Department of Health and is responsible for regulating medicines and medical devices. • The TGA administers the Therapeutic Goods Act 1989 (the Act), applying a risk management approach designed to ensure therapeutic goods supplied in Australia meet acceptable standards of quality, safety and efficacy (performance) when necessary. • The work of the TGA is based on applying scientific and clinical expertise to decision- making, to ensure that the benefits to consumers outweigh any risks associated with the use of medicines and medical devices. • The TGA relies on the public, healthcare professionals and industry to report problems with medicines or medical devices. TGA investigates reports received by it to determine any necessary regulatory action. • To report a problem with a medicine or medical device, please see the information on the TGA website <https://www.tga.gov.au>. About AusPARs • An Australian Public Assessment Report (AusPAR) provides information about the evaluation of a prescription medicine and the considerations that led the TGA to approve or not approve a prescription medicine submission. • AusPARs are prepared and published by the TGA. • An AusPAR is prepared for submissions that relate to new chemical entities, generic medicines, major variations and extensions of indications. • An AusPAR is a static document; it provides information that relates to a submission at a particular point in time. • A new AusPAR will be developed to reflect changes to indications and/or major variations to a prescription medicine subject to evaluation by the TGA. -

Animal Models of Depression: What Can They Teach Us About the Human Disease?
diagnostics Review Animal Models of Depression: What Can They Teach Us about the Human Disease? Maria Becker 1 , Albert Pinhasov 2 and Asher Ornoy 1,3,* 1 Adelson School of Medicine, Ariel University, Ariel 40700, Israel; [email protected] 2 Department of Molecular Biology and Adelson School of Medicine, Ariel University, Ariel 40700, Israel; [email protected] 3 Hebrew University Hadassah Medical School, Jerusalem 9112102, Israel * Correspondence: [email protected] or [email protected]; Tel.: +972-2-6758-329 Abstract: Depression is apparently the most common psychiatric disease among the mood disorders affecting about 10% of the adult population. The etiology and pathogenesis of depression are still poorly understood. Hence, as for most human diseases, animal models can help us understand the pathogenesis of depression and, more importantly, may facilitate the search for therapy. In this review we first describe the more common tests used for the evaluation of depressive-like symptoms in rodents. Then we describe different models of depression and discuss their strengths and weaknesses. These models can be divided into several categories: genetic models, models induced by mental acute and chronic stressful situations caused by environmental manipulations (i.e., learned helplessness in rats/mice), models induced by changes in brain neuro-transmitters or by specific brain injuries and models induced by pharmacological tools. In spite of the fact that none of the models completely resembles human depression, most animal models are relevant since they mimic many of the features observed in the human situation and may serve as a powerful tool for the study of the etiology, pathogenesis and treatment of depression, especially since only few patients respond to acute treatment. -

Fluoxetine Elevates Allopregnanolone in Female Rat Brain but Inhibits A
British Journal of DOI:10.1111/bph.12891 www.brjpharmacol.org BJP Pharmacology RESEARCH PAPER Correspondence Jonathan P Fry, Department of Neuroscience, Physiology and Pharmacology, University College Fluoxetine elevates London, Gower Street, London WC1E 6BT, UK. E-mail: [email protected] allopregnanolone in female ---------------------------------------------------------------- Received 27 March 2014 rat brain but inhibits a Revised 3 July 2014 Accepted steroid microsomal 18 August 2014 dehydrogenase rather than activating an aldo-keto reductase JPFry1,KYLi1, A J Devall2, S Cockcroft1, J W Honour3,4 and T A Lovick5 1Department of Neuroscience, Physiology and Pharmacology, 4Institute of Women’s Health, University College London (UCL), 3Department of Chemical Pathology, University College London Hospital, London, 2School of Clinical and Experimental Medicine, University of Birmingham, Birmingham, and 5School of Physiology and Pharmacology, University of Bristol, Bristol, UK BACKGROUND AND PURPOSE Fluoxetine, a selective serotonin reuptake inhibitor, elevates brain concentrations of the neuroactive progesterone metabolite allopregnanolone, an effect suggested to underlie its use in the treatment of premenstrual dysphoria. One report showed fluoxetine to activate the aldo-keto reductase (AKR) component of 3α-hydroxysteroid dehydrogenase (3α-HSD), which catalyses production of allopregnanolone from 5α-dihydroprogesterone. However, this action was not observed by others. The present study sought to clarify the site of action for fluoxetine in elevating brain allopregnanolone. EXPERIMENTAL APPROACH Adult male rats and female rats in dioestrus were treated with fluoxetine and their brains assayed for allopregnanolone and its precursors, progesterone and 5α-dihydroprogesterone. Subcellular fractions of rat brain were also used to investigate the actions of fluoxetine on 3α-HSD activity in both the reductive direction, producing allopregnanolone from 5α-dihydroprogesterone, and the reverse oxidative direction. -

Early Pregnancy Maternal Progesterone Administration Alters Pituitary and Testis Function and Steroid Profile in Male Fetuses
www.nature.com/scientificreports OPEN Early pregnancy maternal progesterone administration alters pituitary and testis function and steroid profle in male fetuses Katarzyna J. Siemienowicz1,2*, Yili Wang1, Magda Marečková1, Junko Nio‑Kobayashi1,3, Paul A. Fowler4, Mick T. Rae2 & W. Colin Duncan1 Maternal exposure to increased steroid hormones, including estrogens, androgens or glucocorticoids during pregnancy results in chronic conditions in ofspring that manifest in adulthood. Little is known about efects of progesterone administration in early pregnancy on fetal development. We hypothesised that maternal early pregnancy progesterone supplementation would increase fetal progesterone, afect progesterone target tissues in the developing fetal reproductive system and be metabolised to other bioactive steroids in the fetus. We investigated the efects of progesterone treatment during early pregnancy on maternal and fetal plasma progesterone concentrations, transcript abundance in the fetal pituitary and testes and circulating steroids, at day 75 gestation, using a clinically realistic ovine model. Endogenous progesterone concentrations were lower in male than female fetuses. Maternal progesterone administration increased male, but not female, fetal progesterone concentrations, also increasing circulating 11‑dehydrocorticosterone in male fetuses. Maternal progesterone administration altered fetal pituitary and testicular function in ovine male fetuses. This suggests that there may be fetal sex specifc efects of the use of progesterone in early pregnancy, and highlights that progesterone supplementation should be used only when there is clear evidence of efcacy and for as limited time as necessary. Fetal exposure to sex steroids has critical roles in sexual diferentiation and the programming of health and dis- ease in later life1. Exposure to endocrine disrupting compounds is linked to disease development in ofspring2. -

Detectx® Allopregnanolone Enzyme Immunoassay Kit
DetectX® Allopregnanolone Enzyme Immunoassay Kit 1 Plate Kit Catalog Number K061-H1 5 Plate Kit Catalog Number K061-H5 Species Independent Sample Types Validated: Extracted Serum, Plasma, and Dried Fecal Samples, or Urine and Tissue Culture Media Please read this insert completely prior to using the product. For research use only. Not for use in diagnostic procedures. www.ArborAssays.com K061-H WEB 210302 TABLE OF CONTENTS Background 3 Assay Principle 4 Related Products 4 Supplied Components 5 Storage Instructions 5 Other Materials Required 6 Precautions 6 Sample Types 7 Sample Preparation 7 Reagent Preparation 8 Assay Protocol 9 Calculation of Results 10 Typical Data 10-11 Validation Data Sensitivity, Linearity, etc. 11-13 Samples Values and Cross Reactivity 14 Warranty & Contact Information 15 Plate Layout Sheet 16 ® 2 EXPECT ASSAY ARTISTRY™ K061-H WEB 210302 BACKGROUND Allopregnanolone (3α-hydroxy-5α-pregnan-20-one) is a neurosteroid present in the blood and the brain. Allopregnanolone is made from progesterone which is converted into 5α-dihydroprogesterone by 5α-reductase type I. 3α-hydroxysteroid oxidoreductase isoenzymes convert this intermediate into allopregnanolone. 3α-hydroxysteroids do not interact with classical intracellular steroid receptors but bind stereoselectively and with high affinity to receptors for the major inhibitory neurotransmitter in brain, 1 g-amino-butyric acid (GABA) . While allopregnanolone, like other GABAA receptor active neurosteroids, such as allotetrahydrodeoxycorticosterone, positively modulates all GABAA receptor isoforms, those isoforms containing δ-subunits exhibit greater magnitude potentiation. It may be involved in neuronal plasticity, learning and memory processes, aggression, epilepsy, in addition to the modulation of stress responses, anxiety and depression. -
Dosage and Administration
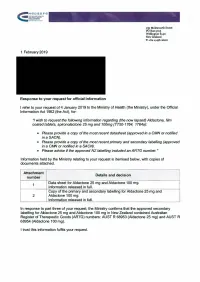
HGDS"'FG ·-···--··-· ..---- ·---·' .. e ·--··---····~·----- 133 Molesworth Street PO Box5013 Wellington 6140 New Zealand T +64 4 496 2000 1 February 2019 Response to your request for official information I refer to your request of 4 January 2019 to the Ministry of Health (the Ministry), under the Official Information Act 1982 (the Act), for. "I wish to request the following information regarding (the now lapsed) Aldactone, film coated tablets, spironolactone 25 mg and 100mg (TTS0-1764, 1764a): • Please provide a copy of the most recent datasheet (approved in a CMN or notified ina SACN). • Please provide a copy of the most recent primary and secondary labelling (approved in a CMN or notified in a SACN). • Please advise if the approved NZ labelling included an ARTG number." Information held by the Ministry relating to your request is itemised below, with copies of documents attached. Attachment Details and decision number - Data sheet for Aldactone 25 mg and Aldactone 100 mg. 1 Information released in full. Copy of the primary and secondary labelling for Aldactone 25 mg and 2 Aldactone 100 mg. Information released in full. In response to part three of your request, the Ministry confirms that the approved secondary labelling for Aldactone 25 mg and Aldactone 100 mg in New Zealand contained Australian Register of Therapeutic Goods (ARTG) numbers: AUST R 68953 (Aldactone 25 mg) and AUST R 68954 (Aldactone 100 mg). I trust this information fulfils your request. Please note this response (with your personal details removed) may be published on the Ministry of Health website. Yours si r;,c;:arely ~ r,,..~-~/___/ / /.. -

Changes in Brain Testosterone and Allopregnanolone Biosynthesis Elicit Aggressive Behavior
Changes in brain testosterone and allopregnanolone biosynthesis elicit aggressive behavior Graziano Pinna*, Erminio Costa, and Alessandro Guidotti Psychiatric Institute, Department of Psychiatry, College of Medicine, University of Illinois, Chicago, IL 60612 Contributed by Erminio Costa, December 23, 2004 In addition to an action on metabolism, anabolic͞androgenic ste- of testosterone results in the development of GABAergic trans- roids also increase sex drive and mental acuity. If abused, such mission down-regulation (8, 16). Hence, GABAergic transmis- steroids can cause irritability, impulsive aggression, and signs of sion may be an important mechanism underlying the action major depression [Pearson, H. (2004) Nature 431, 500–501], but the of AAS. mechanisms that produce these symptoms are unknown. The Several studies in mice unrelated to AAS have unequivocally present study investigates behavioral and neurochemical alter- shown that a GABAergic transmission impairment plays a ations occurring in association with protracted (3-week) adminis- pivotal role in the expression of aggressive behavior (18–20). For tration of testosterone propionate (TP) to socially isolated (SI) and example, the down-regulation of GABAA receptor signal trans- group-housed male and female mice. Male but not female SI mice duction (18–23) in socially isolated (SI) aggressive male mice is exhibit aggression that correlates with the down-regulation of associated with a down-regulation of 3␣-hydroxysteroid-5␣- brain neurosteroid biosynthesis. However, in female mice, long- pregnan-20-one (allopregnanolone, Allo) biosynthesis (19–21, term TP administration induces aggression associated with a de- 24). Allo acts as a potent (nM concentrations) positive allosteric crease of brain allopregnanolone (Allo) content and a decrease Ϸ ␣ modulator of signal transduction at several GABAA receptor ( 40%) of 5 -reductase type I mRNA expression.