IL-33-ST2 Axis Regulates Myeloid Cell Differentiation and Activation Enabling Effective Club Cell Regeneration
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Peking University-Juntendo University Joint Symposium on Cancer Research and Treatment ADAM28 (A Disintegrin and Metalloproteinase 28) in Cancer Cell Proliferation and Progression
Whatʼs New from Juntendo University, Tokyo Juntendo Medical Journal 2017. 63(5), 322-325 Peking University - Juntendo University Joint Symposium on Cancer Research and Treatment ADAM28 (a Disintegrin and Metalloproteinase 28) in Cancer Cell Proliferation and Progression YASUNORI OKADA* *Department of Pathophysiology for Locomotive and Neoplastic Diseases, Juntendo University Graduate School of Medicine, Tokyo, Japan A disintegrinandmetalloproteinase 28 (ADAM28) is overexpressedpredominantlyby carcinoma cells in more than 70% of the non-small cell lung carcinomas, showing positive correlations with carcinoma cell proliferation and metastasis. ADAM28 cleaves insulin-like growth factor binding protein-3 (IGFBP-3) in the IGF-I/IGFBP-3 complex, leading to stimulation of cell proliferation by intact IGF-I released from the complex. ADAM28 also degrades von Willebrand factor (VWF), which induces apoptosis in human carcinoma cell lines with negligible ADAM28 expression, andthe VWF digestionby ADAM28-expressing carcinoma cells facilitates them to escape from VWF-induced apoptosis, resulting in promotion of metastasis. We have developed human antibodies against ADAM28 andshown that one of them significantly inhibits tumor growth andmetastasis using lung adenocarcinoma cells. Our data suggest that ADAM28 may be a new molecular target for therapy of the patients with ADAM28-expressing non-small cell lung carcinoma. Key words: a disintegrin and metalloproteinase 28 (ADAM28), cell proliferation, invasion, metastasis, human antibody inhibitor Introduction human cancers 2). However, development of the synthetic inhibitors of MMPs andtheir application Cancer cell proliferation andprogression are for treatment of the cancer patients failed 3). modulated by proteolytic cleavage of tissue micro- On the other hand, members of the ADAM (a environmental factors such as extracellular matrix disintegrin and metalloproteinase) gene family, (ECM), growth factors andcytokines, receptors another family belonging to the metzincin gene andcell adhesionmolecules. -

Integrative Genome Analysis of Somatic P53 Mutant Osteosarcomas Identifies Ets2-Dependent Regulation of Small Nucleolar Rnas by Mutant P53 Protein
Downloaded from genesdev.cshlp.org on September 30, 2021 - Published by Cold Spring Harbor Laboratory Press Integrative genome analysis of somatic p53 mutant osteosarcomas identifies Ets2-dependent regulation of small nucleolar RNAs by mutant p53 protein Rasoul Pourebrahim,1 Yun Zhang,1 Bin Liu,1 Ruli Gao,1 Shunbin Xiong,1 Patrick P. Lin,2 Mark J. McArthur,3 Michael C. Ostrowski,4 and Guillermina Lozano1 1Department of Genetics, University of Texas MD Anderson Cancer Center, Houston, Texas 77030, USA; 2Department of Orthopedic Oncology, University of Texas MD Anderson Cancer Center, Houston, Texas 77030, USA; 3Department of Veterinary Medicine and Surgery, University of Texas MD Anderson Cancer Center, Houston, Texas 77030, USA; 4Department of Cancer Biology and Genetics, The Ohio State University, Columbus, Ohio 43210, USA TP53 is the most frequently mutated gene in human cancer. Many mutant p53 proteins exert oncogenic gain-of- function (GOF) properties that contribute to metastasis, but the mechanisms mediating these functions remain poorly defined in vivo. To elucidate how mutant p53 GOF drives metastasis, we developed a traceable somatic os- teosarcoma mouse model that is initiated with either a single p53 mutation (p53R172H) or p53 loss in osteoblasts. Our study confirmed that p53 mutant mice developed osteosarcomas with increased metastasis as compared with p53-null mice. Comprehensive transcriptome RNA sequencing (RNA-seq) analysis of 16 tumors identified a cluster of small nucleolar RNAs (snoRNAs) that are highly up-regulated in p53 mutant tumors. Regulatory element analysis of these deregulated snoRNA genes identified strong enrichment of a common Ets2 transcription factor-binding site. Homozygous deletion of Ets2 in p53 mutant mice resulted in strong down-regulation of snoRNAs and reversed the prometastatic phenotype of mutant p53 but had no effect on osteosarcoma development, which remained 100% penetrant. -

Mapping the Genetic Architecture of Gene Regulation in Whole Blood
Mapping the Genetic Architecture of Gene Regulation in Whole Blood Katharina Schramm1,2., Carola Marzi3,4,5., Claudia Schurmann6., Maren Carstensen7,8., Eva Reinmaa9,10, Reiner Biffar11, Gertrud Eckstein1, Christian Gieger12, Hans-Jo¨ rgen Grabe13, Georg Homuth6, Gabriele Kastenmu¨ ller14, Reedik Ma¨gi10, Andres Metspalu9,10, Evelin Mihailov10,15, Annette Peters2, Astrid Petersmann16, Michael Roden7,8,17, Konstantin Strauch12,18, Karsten Suhre14,19, Alexander Teumer6,UweVo¨ lker6, Henry Vo¨ lzke20, Rui Wang-Sattler3,4, Melanie Waldenberger3,4, Thomas Meitinger1,2,21, Thomas Illig22, Christian Herder7,8., Harald Grallert3,4,5., Holger Prokisch1,2*. 1 Institute of Human Genetics, Helmholtz Center Munich, German Research Center for Environmental Health, Neuherberg, Germany, 2 Institute of Human Genetics, Technical University Munich, Mu¨nchen, Germany, 3 Research Unit of Molecular Epidemiology, Helmholtz Center Munich, German Research Center for Environmental Health, Neuherberg, Germany, 4 Institute of Epidemiology II, Helmholtz Center Munich, German Research Center for Environmental Health, Neuherberg, Germany, 5 German Center for Diabetes Research (DZD e.V.), Neuherberg, Germany, 6 Interfaculty Institute for Genetics and Functional Genomics, Department of Functional Genomics, University Medicine Greifswald, Greifswald, Germany, 7 Institute for Clinical Diabetology, German Diabetes Center, Leibniz Center for Diabetes Research at Heinrich Heine University Du¨sseldorf, Du¨sseldorf, Germany, 8 German Center for Diabetes Research (DZD e.V.), -

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -

Microarray Analysis of Bone Marrow Lesions in Osteoarthritis
ARD Online First, published on July 13, 2017 as 10.1136/annrheumdis-2017-211396 Basic and translational research Ann Rheum Dis: first published as 10.1136/annrheumdis-2017-211396 on 13 July 2017. Downloaded from EXTENDED REPORT Microarray analysis of bone marrow lesions in osteoarthritis demonstrates upregulation of genes implicated in osteochondral turnover, neurogenesis and inflammation Anasuya Kuttapitiya,1 Lena Assi,1 Ken Laing,1 Caroline Hing,2 Philip Mitchell,2 Guy Whitley,3 Abiola Harrison,1 Franklyn A Howe,3 Vivian Ejindu,2 Christine Heron,2 Nidhi Sofat1 ► Additional material is ABSTRACT affecting the knees in up to 37% of adults over published online only. To view Objective Bone marrow lesions (BMLs) are well 60.1 Pain is a major symptom for people with OA, please visit the journal online described in osteoarthritis (OA) using MRI and are with 16.7% of US adults aged 45 years and above (http:// dx. doi. org/ 10. 1136/ 1 annrheumdis- 2017- 211396). associated with pain, but little is known about their reporting pain as a predominant problem. pathological characteristics and gene expression. We Pain in OA is thought to arise from several 1 Institute for Infection & evaluated BMLs using novel tissue analysis tools to gain structures within the arthritic joint, including the Immunity, St George's, a deeper understanding of their cellular and molecular synovium (from which prostaglandins, leukot- University of London, London, UK expression. rienes and inflammatory mediators are released), 2St George's University Methods We recruited 98 participants, 72 with joint effusions, joint capsule involvement, tendon Hospitals NHS Foundation Trust, advanced OA requiring total knee replacement (TKR), 12 and muscle weakness that all contribute to pain London, UK 3 3 with mild OA and 14 non-OA controls. -
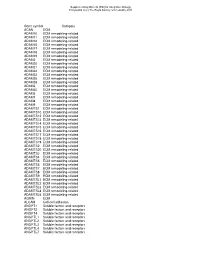
Gene Symbol Category ACAN ECM ADAM10 ECM Remodeling-Related ADAM11 ECM Remodeling-Related ADAM12 ECM Remodeling-Related ADAM15 E
Supplementary Material (ESI) for Integrative Biology This journal is (c) The Royal Society of Chemistry 2010 Gene symbol Category ACAN ECM ADAM10 ECM remodeling-related ADAM11 ECM remodeling-related ADAM12 ECM remodeling-related ADAM15 ECM remodeling-related ADAM17 ECM remodeling-related ADAM18 ECM remodeling-related ADAM19 ECM remodeling-related ADAM2 ECM remodeling-related ADAM20 ECM remodeling-related ADAM21 ECM remodeling-related ADAM22 ECM remodeling-related ADAM23 ECM remodeling-related ADAM28 ECM remodeling-related ADAM29 ECM remodeling-related ADAM3 ECM remodeling-related ADAM30 ECM remodeling-related ADAM5 ECM remodeling-related ADAM7 ECM remodeling-related ADAM8 ECM remodeling-related ADAM9 ECM remodeling-related ADAMTS1 ECM remodeling-related ADAMTS10 ECM remodeling-related ADAMTS12 ECM remodeling-related ADAMTS13 ECM remodeling-related ADAMTS14 ECM remodeling-related ADAMTS15 ECM remodeling-related ADAMTS16 ECM remodeling-related ADAMTS17 ECM remodeling-related ADAMTS18 ECM remodeling-related ADAMTS19 ECM remodeling-related ADAMTS2 ECM remodeling-related ADAMTS20 ECM remodeling-related ADAMTS3 ECM remodeling-related ADAMTS4 ECM remodeling-related ADAMTS5 ECM remodeling-related ADAMTS6 ECM remodeling-related ADAMTS7 ECM remodeling-related ADAMTS8 ECM remodeling-related ADAMTS9 ECM remodeling-related ADAMTSL1 ECM remodeling-related ADAMTSL2 ECM remodeling-related ADAMTSL3 ECM remodeling-related ADAMTSL4 ECM remodeling-related ADAMTSL5 ECM remodeling-related AGRIN ECM ALCAM Cell-cell adhesion ANGPT1 Soluble factors and receptors -

Proquest Dissertations
urn u Ottawa L'Universitd canadienne Canada's university FACULTE DES ETUDES SUPERIEURES l^^l FACULTY OF GRADUATE AND ET POSTDOCTORALES u Ottawa POSTDOCTORAL STUDIES I.'University emiadienne Canada's university Charles Gyamera-Acheampong AUTEUR DE LA THESE / AUTHOR OF THESIS Ph.D. (Biochemistry) GRADE/DEGREE Biochemistry, Microbiology and Immunology FACULTE, ECOLE, DEPARTEMENT / FACULTY, SCHOOL, DEPARTMENT The Physiology and Biochemistry of the Fertility Enzyme Proprotein Convertase Subtilisin/Kexin Type 4 TITRE DE LA THESE / TITLE OF THESIS M. Mbikay TIRECTWRTDIRICTR^ CO-DIRECTEUR (CO-DIRECTRICE) DE LA THESE / THESIS CO-SUPERVISOR EXAMINATEURS (EXAMINATRICES) DE LA THESE/THESIS EXAMINERS A. Basak G. Cooke F .Kan V. Mezl Gary W. Slater Le Doyen de la Faculte des etudes superieures et postdoctorales / Dean of the Faculty of Graduate and Postdoctoral Studies Library and Archives Bibliotheque et 1*1 Canada Archives Canada Published Heritage Direction du Branch Patrimoine de I'edition 395 Wellington Street 395, rue Wellington OttawaONK1A0N4 Ottawa ON K1A 0N4 Canada Canada Your file Votre reference ISBN: 978-0-494-59504-6 Our file Notre reference ISBN: 978-0-494-59504-6 NOTICE: AVIS: The author has granted a non L'auteur a accorde une licence non exclusive exclusive license allowing Library and permettant a la Bibliotheque et Archives Archives Canada to reproduce, Canada de reproduire, publier, archiver, publish, archive, preserve, conserve, sauvegarder, conserver, transmettre au public communicate to the public by par telecommunication ou par I'lnternet, prefer, telecommunication or on the Internet, distribuer et vendre des theses partout dans le loan, distribute and sell theses monde, a des fins commerciales ou autres, sur worldwide, for commercial or non support microforme, papier, electronique et/ou commercial purposes, in microform, autres formats. -

Conservation and Divergence of ADAM Family Proteins in the Xenopus Genome
Wei et al. BMC Evolutionary Biology 2010, 10:211 http://www.biomedcentral.com/1471-2148/10/211 RESEARCH ARTICLE Open Access ConservationResearch article and divergence of ADAM family proteins in the Xenopus genome Shuo Wei*1, Charles A Whittaker2, Guofeng Xu1, Lance C Bridges1,3, Anoop Shah1, Judith M White1 and Douglas W DeSimone1 Abstract Background: Members of the disintegrin metalloproteinase (ADAM) family play important roles in cellular and developmental processes through their functions as proteases and/or binding partners for other proteins. The amphibian Xenopus has long been used as a model for early vertebrate development, but genome-wide analyses for large gene families were not possible until the recent completion of the X. tropicalis genome sequence and the availability of large scale expression sequence tag (EST) databases. In this study we carried out a systematic analysis of the X. tropicalis genome and uncovered several interesting features of ADAM genes in this species. Results: Based on the X. tropicalis genome sequence and EST databases, we identified Xenopus orthologues of mammalian ADAMs and obtained full-length cDNA clones for these genes. The deduced protein sequences, synteny and exon-intron boundaries are conserved between most human and X. tropicalis orthologues. The alternative splicing patterns of certain Xenopus ADAM genes, such as adams 22 and 28, are similar to those of their mammalian orthologues. However, we were unable to identify an orthologue for ADAM7 or 8. The Xenopus orthologue of ADAM15, an active metalloproteinase in mammals, does not contain the conserved zinc-binding motif and is hence considered proteolytically inactive. We also found evidence for gain of ADAM genes in Xenopus as compared to other species. -

Protein Disulfide Isomerase Homolog PDILT Is Required for Quality Control
Correction DEVELOPMENTAL BIOLOGY Correction for “Protein disulfide isomerase homolog PDILT is required for quality control of sperm membrane protein ADAM3 and male infertility,” by Keizo Tokuhiro, Masahito Ikawa, Adam M. Benham, and Masaru Okabe, which appeared in issue 10, March 6, 2012, of Proc Natl Acad Sci USA (109: 3850–3855; first published February 22, 2012; 10.1073/pnas. 1117963109). The authors note that the title appeared incorrectly. The title should instead appear as “Protein disulfide isomerase homolog PDILT is required for quality control of sperm membrane protein ADAM3 and male fertility.” The online version has been corrected. www.pnas.org/cgi/doi/10.1073/pnas.1204275109 CORRECTION www.pnas.org PNAS | April 10, 2012 | vol. 109 | no. 15 | 5905 Downloaded by guest on September 24, 2021 Protein disulfide isomerase homolog PDILT is required for quality control of sperm membrane protein ADAM3 and male fertility Keizo Tokuhiroa, Masahito Ikawaa,1, Adam M. Benhama,b, and Masaru Okabea,c,d aResearch Institute for Microbial Diseases, cGraduate School of Pharmaceutical Sciences, and dImmunology Frontier Research Center, Osaka University, Suita, Osaka 565-0871, Japan; and bSchool of Biological and Biomedical Sciences, Durham University, Durham DH1 3LE, United Kingdom Edited by Ryuzo Yanagimachi, Institute for Biogenesis Research, University of Hawaii, Honolulu, HI, and approved January 31, 2012 (received for review November 1, 2011) A disintegrin and metalloproteinase 3 (ADAM3) is a sperm mem- misfolded proteins. Whereas homologous lectin chaperones, brane protein critical for both sperm migration from the uterus calnexin/calreticulin (CANX/CALR), chiefly mediate nascent into the oviduct and sperm primary binding to the zona pellucida glycoprotein folding in the somatic cells (14), testicular germ (ZP). -

Identification of Platform-Independent Diagnostic Biomarker Panel For
bioRxiv preprint doi: https://doi.org/10.1101/758250; this version posted September 5, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 Identification of Platform-Independent Diagnostic Biomarker Panel for 2 Hepatocellular Carcinoma using Large-scale Transcriptomics Data 3 Harpreet Kaur1,2, Anjali Dhall2, Rajesh Kumar1,2, Gajendra P. S. Raghava2,* 4 1 Bioinformatics Center, CSIR-Institute of Microbial Technology, Chandigarh, India 5 2 Department of Computational Biology, Indraprastha Institute of Information Technology, New 6 Delhi, India 7 8 Emails of Authors: 9 Harpreet Kaur: [email protected] , [email protected] 10 Anjali Dhall: [email protected] 11 Rajesh Kumar: [email protected] 12 Gajendra P.S. Raghava: [email protected] 13 14 15 * Correspondence 16 Professor, Department of Computational Biology 17 Indraprastha Institute of Information Technology, 18 Okhla Industrial Estate, Phase III, New Delhi 110020, 19 India. Tel.: +91 011 26907444; E-mail address: [email protected] 20 21 22 23 24 25 26 27 28 bioRxiv preprint doi: https://doi.org/10.1101/758250; this version posted September 5, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 29 Abstract 30 The high mortality rate of hepatocellular carcinoma (HCC) is primarily due to its late diagnosis. -

Human Lectins, Their Carbohydrate Affinities and Where to Find Them
biomolecules Review Human Lectins, Their Carbohydrate Affinities and Where to Review HumanFind Them Lectins, Their Carbohydrate Affinities and Where to FindCláudia ThemD. Raposo 1,*, André B. Canelas 2 and M. Teresa Barros 1 1, 2 1 Cláudia D. Raposo * , Andr1 é LAQVB. Canelas‐Requimte,and Department M. Teresa of Chemistry, Barros NOVA School of Science and Technology, Universidade NOVA de Lisboa, 2829‐516 Caparica, Portugal; [email protected] 12 GlanbiaLAQV-Requimte,‐AgriChemWhey, Department Lisheen of Chemistry, Mine, Killoran, NOVA Moyne, School E41 of ScienceR622 Co. and Tipperary, Technology, Ireland; canelas‐ [email protected] NOVA de Lisboa, 2829-516 Caparica, Portugal; [email protected] 2* Correspondence:Glanbia-AgriChemWhey, [email protected]; Lisheen Mine, Tel.: Killoran, +351‐212948550 Moyne, E41 R622 Tipperary, Ireland; [email protected] * Correspondence: [email protected]; Tel.: +351-212948550 Abstract: Lectins are a class of proteins responsible for several biological roles such as cell‐cell in‐ Abstract:teractions,Lectins signaling are pathways, a class of and proteins several responsible innate immune for several responses biological against roles pathogens. such as Since cell-cell lec‐ interactions,tins are able signalingto bind to pathways, carbohydrates, and several they can innate be a immuneviable target responses for targeted against drug pathogens. delivery Since sys‐ lectinstems. In are fact, able several to bind lectins to carbohydrates, were approved they by canFood be and a viable Drug targetAdministration for targeted for drugthat purpose. delivery systems.Information In fact, about several specific lectins carbohydrate were approved recognition by Food by andlectin Drug receptors Administration was gathered for that herein, purpose. plus Informationthe specific organs about specific where those carbohydrate lectins can recognition be found by within lectin the receptors human was body. -

The Emerging Role of Matrix Metalloproteases of the ADAM Family in Male Germ Cell Apoptosis
review REVIEW Spermatogenesis 1:3, 195-208; July/August/September 2011; © 2011 Landes Bioscience The emerging role of matrix metalloproteases of the ADAM family in male germ cell apoptosis Ricardo D. Moreno,* Paulina Urriola-Muñoz and Raúl Lagos-Cabré Departamento de Fisiología; Pontificia Universidad Católica de Chile; Santiago, Chile Key words: spermatogenesis, apoptosis, metalloprotease, infertility Constitutive germ cell apoptosis during mammalian sperm- Despite that some data suggest that germ cell apoptosis is autono- atogenesis is a key process for controlling sperm output and to mous (independent of the environment), the role of the Sertoli eliminate damaged or unwanted cells. An increase or decrease cell should not be disregarded, because it may provide important in the apoptosis rate has deleterious consequences and leads survival and/or dead clues to germ cells (see below). Germ cell to low sperm production. Apoptosis in spermatogenesis has been widely studied, but the mechanism by which it is induced apoptosis has been shown to play an important role in control- under physiological or pathological conditions has not been ling sperm output in many species, and in humans it has been 5-10 clarified. We have recently identified the metalloprotease related to infertility. Additionally, it has been proposed that ADAM17 (TACE) as a putative physiological inducer of germ the purported decline in global sperm production is caused by cell apoptosis. The mechanisms involved in regulating the environmental xenoestrogens that induce germ cell apoptosis.11 shedding of the ADAM17 extracellular domain are still far In the same way, a modern lifestyle and the use of underwear has from being understood, although they are important in order been proposed to induce elevated scrotal temperature that may to understand cell-cell communications.