Choosing Wisely
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Male Reproductive System
Management of Men’s Reproductive 3 Health Problems Men’s Reproductive Health Curriculum Management of Men’s Reproductive 3 Health Problems © 2003 EngenderHealth. All rights reserved. 440 Ninth Avenue New York, NY 10001 U.S.A. Telephone: 212-561-8000 Fax: 212-561-8067 e-mail: [email protected] www.engenderhealth.org This publication was made possible, in part, through support provided by the Office of Population, U.S. Agency for International Development (USAID), under the terms of cooperative agreement HRN-A-00-98-00042-00. The opinions expressed herein are those of the publisher and do not necessarily reflect the views of USAID. Cover design: Virginia Taddoni ISBN 1-885063-45-8 Printed in the United States of America. Printed on recycled paper. Library of Congress Cataloging-in-Publication Data Men’s reproductive health curriculum : management of men’s reproductive health problems. p. ; cm. Companion v. to: Introduction to men’s reproductive health services, and: Counseling and communicating with men. Includes bibliographical references. ISBN 1-885063-45-8 1. Andrology. 2. Human reproduction. 3. Generative organs, Male--Diseases--Treatment. I. EngenderHealth (Firm) II. Counseling and communicating with men. III. Title: Introduction to men’s reproductive health services. [DNLM: 1. Genital Diseases, Male. 2. Physical Examination--methods. 3. Reproductive Health Services. WJ 700 M5483 2003] QP253.M465 2003 616.6’5--dc22 2003063056 Contents Acknowledgments v Introduction vii 1 Disorders of the Male Reproductive System 1.1 The Male -

Sara Aghamohammadi, M.D
Sara Aghamohammadi, M.D. Philosophy of Care It is a privilege to care for children and their families during the time of their critical illness. I strive to incorporate the science and art of medicine in my everyday practice such that each child and family receives the best medical care in a supportive and respectful environment. Having grown up in the San Joaquin Valley, I am honored to join UC Davis Children's Hospital's team and contribute to the well-being of our community's children. Clinical Interests Dr. Aghamohammadi has always had a passion for education, she enjoys teaching principles of medicine, pediatrics, and critical care to medical students, residents, and nurses alike. Her clinical interests include standardization of practice in the PICU through the use of protocols. Her team has successfully implemented a sedation and analgesia protocol in the PICU, and she helped develop the high-flow nasal cannula protocol for bronchiolitis. Additionally, she has been involved in the development of pediatric pain order sets and is part of a multi-disciplinary team to address acute and chronic pain in pediatric patients. Research/Academic Interests Dr. Aghamohammadi has been passionate about Physician Health and Well-being and heads the Wellness Committee for the Department of Pediatrics. Additionally, she is a part of the Department Wellness Champions for the UC Davis Health System and has given presentations on the importance of Physician Wellness. After completing training in Physician Health and Well-being, she now serves as a mentor for the Train-the-Trainer Physician Health and Well-being Fellowship. -

Nutrition in Andrology, Gynaecology and Obstetrics
Appendix No. 2 to the procedure of development and periodical review of syllabuses Nutrition in Andrology, Gynaecology and Obstetrics 1. Imprint Faculty name: English Division Syllabus (field of study, level and educational profile, form of studies, Medicine, 1st level studies, practical profile, full time e.g., Public Health, 1st level studies, practical profile, full time): Academic year: 2019/2020 Nutrition in Andrology, Gynaecology and Module/subject name: Obstetrics Subject code (from the Pensum system): Educational units: Department of Social Medicine and Public Health Head of the unit/s: Dr hab. n. med. Aneta Nitsch - Osuch Study year (the year during which the 1st-6th respective subject is taught): Study semester (the semester during which the respective subject is Winter and Summer semesters taught): Module/subject type (basic, corresponding to the field of study, Optional optional): Teachers (names and surnames and Anna Jagielska, MD degrees of all academic teachers of Aleksandra Kozłowska, BSc respective subjects): ERASMUS YES/NO (Is the subject available for students under the YES ERASMUS programme?): A person responsible for the syllabus (a person to which all comments to Anna Jagielska, MD the syllabus should be reported) Number of ECTS credits: 2 Page 1 of 4 Appendix No. 2 to the procedure of development and periodical review of syllabuses 2. Educational goals and aims The aim of the course is to provide students with: 1. The principles of nutrition during adolescence, adulthood and eldery. 2. The relationship between nutrition and fertility, fetal status and communicable diseases in the adults life. 3. Basics of dietary advices for men and women in the reproductive years. -

In 6861.Indd
Original Article Sexuality during gestation DOI: 10.5020/18061230.2018.6861 MALE PERCEPTION OF SEXUAL ACTIVITY IN THE GESTATIONAL PERIOD Percepção masculina sobre atividade sexual no período gestacional Percepción masculina sobre la actividad sexual en el período gestacional Dailon de Araújo Alves Regional University of Cariri (Universidade Regional do Cariri - URCA) - Crato (CE) - Brazil Brunna Suélli de Souza Alves Faculty of Juazeiro do Norte (Faculdade de Juazeiro do Norte - FJN) - Juazeiro do Norte (CE) - Brazil Willma José de Santana Faculty of Juazeiro do Norte (Faculdade de Juazeiro do Norte - FJN) - Juazeiro do Norte (CE) - Brazil Felice Teles Lira dos Santos Moreira Regional University of Cariri (Universidade Regional do Cariri - URCA) - Crato (CE) - Brazil Dayanne Rakelly de Oliveira Regional University of Cariri (Universidade Regional do Cariri - URCA) - Crato (CE) - Brazil Grayce Alencar Albuquerque Regional University of Cariri (Universidade Regional do Cariri - URCA) - Crato (CE) - Brazil ABSTRACT Objective: To describe men’s perception of the sexual activity during the gestational period, in the context of the daily life experienced with their pregnant partners. Methods: This is a descriptive study with a qualitative approach. The study included 10 spouses of pregnant women attended to at Basic Health Units in the city of Juazeiro do Norte, Ceará, Brazil. Data was collected between September and October 2015, through a semi-structured interview and evaluated through the systematic technique of content analysis, and analyzed in light of the pertinent literature. Results: The majority of interviewees belonged to the age group between 24 and 29 years, attended high school and were married. For the study participants, when it comes to sexuality, some understand it as something beyond sexual intercourse, whereas, for others, sexuality is related only to intercourse. -

Sexual Dysfunction and Related Factors in Pregnancy
Banaei et al. Systematic Reviews (2019) 8:161 https://doi.org/10.1186/s13643-019-1079-4 PROTOCOL Open Access Sexual dysfunction and related factors in pregnancy and postpartum: a systematic review and meta-analysis protocol Mojdeh Banaei1, Maryam Azizi2, Azam Moridi3, Sareh Dashti4, Asiyeh Pormehr Yabandeh3 and Nasibeh Roozbeh3* Abstract Background: Sexual dysfunction refers to a chain of psychiatric, individual, and couple’s experiences that manifests itself as a dysfunction in sexual desire, sexual arousal, orgasm, and pain during intercourse. The aim of this systematic review will be to assess the sexual dysfunction and determine the relevant factors to sexual dysfunction during pregnancy and postpartum. Methods and analysis: All observational studies, including descriptive, descriptive-analytic, case-control, and cohort studies published between 1990 and 2019, will be included in the study. Review articles, case studies, case reports, letter to editors, pilot studies, and editorial will be excluded from the study. The search will be conducted in the Cochrane Central Register, MEDLINE, Google Scholar, EMBASE, ProQuest, Scopus, WOS, and CINAHL databases. Eligible studies should assess at least one of the sexual dysfunction symptoms in pregnant women orinthefirstyearpostpartum.Quality assessment of studies will be performed by two authors independently based on the NOS checklist. This checklist is designed to assess the quality of observational studies. Data will be analyzed using Stata software ver. 11. Considering that the index investigated in the present study will be the level of sexual disorder, standard error will be calculated for each study using binomial distribution. The heterogeneity level will be investigated using Cochran’sQstatisticandI2 index in a chi-square test at a significance level of 1.1. -
An Alcohol-Free Pregnancy Is the Best Choice for Your Baby
AN ALCOHOL-FREE PREGNANCY IS THE BEST CHOICE FOR YOUR BABY. PREGNANCY AND ALCOHOL DON’T MIx. Helpful Resources The organizations and resources below can provide you with more information on FASDs, drinking and pregnancy, and how to get help if you are pregnant or trying to get pregnant and cannot stop drinking. Centers for Disease Control and Prevention’s National Center on Birth Defects and Developmental Disabilities www.cdc.gov/fasd or call 800–CDC–INFO Substance Abuse and Mental Health Services Administration (SAMHSA) FASD Center for Excellence www.fasdcenter.samhsa.gov National Organization on Fetal Alcohol Syndrome (NOFAS) www.nofas.org or call 800–66–NOFAS (66327) National Council on Alcoholism and Drug Dependence (NCADD) www.ncadd.org or call 800–NCA–CALL (622-2255) Substance Abuse Treatment Facility Locator www.findtreatment.samhsa.gov or call 800–622–HELP (4357) Alcoholics Anonymous www.aa.org March of Dimes www.marchofdimes.com National Institute on Alcohol Abuse and Alcoholism www.niaaa.nih.gov This chart shows vulnerability of the fetus to defects throughout 38 weeks of pregnancy.* Fetal DevelopMent Chart • = Most common site of birth defects PERIOD OF THE OvuM perioD oF the eMBryo PERIOD OF THE FETUS Weeks Weeks 1-2 Week 3 Week 4 Week 5 Week 6 Week 7 Week 8 Week 12 Week 16 20–36 Week 38 Period of early embryo ear brain development CNS eye ear palate and implantation. eye heart heart limbs teeth external genitals Central nervous System (CnS)–Brain and Spinal Cord Heart arms/legs Eyes teeth Palate external Genitals Pregnancy loss Ears Adapted from Moore, 1993 and Period of development when major defects in bodily structure can occur. -
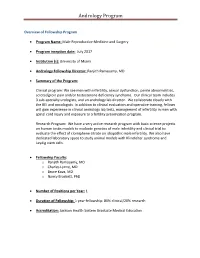
Andrology Program
Andrology Program Overview of Fellowship Program Program Name: Male Reproductive Medicine and Surgery Program inception date: July 2017 Institution (s): University of Miami Andrology Fellowship Director: Ranjith Ramasamy, MD Summary of the Program: Clinical program: We see men with infertility, sexual dysfunction, penile abnormalities, scrotal/groin pain and/or testosterone deficiency syndrome. Our clinical team includes 3 sub-specialty urologists, and an andrology lab director. We collaborate closely with the REI and oncologists. In addition to clinical evaluation and operative training, fellows will gain experience in clinical andrology lab tests, management of infertility in men with spinal cord injury and exposure to a fertility preservation program. Research Program: We have a very active research program with basic science projects on human testis models to evaluate genetics of male infertility and clinical trial to evaluate the effect of clomiphene citrate on idiopathic male infertility. We also have dedicated laboratory space to study animal models with Klinefelter syndrome and Leydig stem cells. Fellowship Faculty: o Ranjith Ramasamy, MD o Charles Lynne, MD o Bruce Kava, MD o Nancy Brackett, PhD Number of Positions per Year: 1 Duration of Fellowship: 1 year fellowship: 80% clinical/20% research Accreditation: Jackson Health System Graduate Medical Education Andrology Program Who to contact regarding the program: Millie Ferro Urology Administration M-814 Leonard M. Miller School of Medicine Contact e-mail: [email protected] Contact phone number: (305) 243-3246 Fax: (305) 243-6597 Contact Website: Overview of Fellowship Program / Description of Program: The Male Reproductive Medicine and Surgery Fellowship will enable the fellow to acquire an advanced body of knowledge and level of skill in the management of reproductive and sexual health diseases in order to assume a leadership role in teaching and research in the field. -

18 Percent of Pregnant Women Drink Alcohol During Early
National Survey on Drug Use and Health The NSDUH Report Data Spotlight September 9, 2013 18 Percent of Pregnant VA60 Women Drink Alcohol during Early Pregnancy Women who drink alcohol while pregnant increase the risk that their infants will have physical, learning, and/or behavior problems, including Fetal Alcohol Spectrum Disorder (FASD).1 These problems are caused by alcohol and can be lifelong. Combined 2011 to 2012 data from the National Survey on Drug Use and Health (NSDUH) show that 8.5 percent of pregnant women aged 15 to 44 drank alcohol in the past month (Figure). Also, 2.7 percent binge drank.2 Among women aged 15 to 44 who were not pregnant, 55.5 percent drank alcohol in the past month, and 24.7 percent binge drank. Most alcohol use by pregnant women occurred during the first trimester. Alcohol use was lower during the second and third trimesters than during the first (4.2 and 3.7 percent vs. 17.9 percent). These findings suggest that many pregnant women are getting the message and not drinking alcohol. Alcohol can disrupt fetal development at Past Month Alcohol Use and Binge Alcohol Use among Pregnant Women Aged any stage during a pregnancy, even before a 15 to 44, Overall and by Trimester*: 2011 and 2012 woman knows she is pregnant.3 If a woman is pregnant, there is no known amount 20 Any Alcohol Use 17.9 or type of alcohol that is safe for her to Binge Alcohol Use drink.4 To prevent problems like FASD, a woman who is pregnant or likely to become 15 pregnant should not drink alcohol. -

Andrology Lab Booklet
or Reprod er f uc nt ti e ve C M n a e c d i i r c e i Andrology Center and n m e A C e 3 9 n 9 tr 1 um t. E Es Reproductive Tissue Bank xcellentiae Who We Are What We Offer The Andrology Center and Reproductive Tissue Bank - The Andrology Center and Reproductive Tissue a section of the Glickman Urological & Kidney Institute Bank’s specialized laboratory offers a wide variety at Cleveland Clinic - provides specialized tests and of comprehensive tests and the latest technology services to evaluate male infertility. Our laboratory to meet patient needs. The Andrology Center offers offers referring physicians and patient’s quantifiable both research and clinical services. Our laboratory results using the latest state-of-the art technology. uses the latest World Health Organization (WHO, We are located in the Building X, which is part of the Fifth Edition, 2010) guidelines and reference ranges Downtown Main campus. in the evaluation of semen samples. Additionally, our laboratory’s Therapeutic Sperm Banking As part of the American Center for Reproductive program provides a complete fertility preservation Medicine, the Andrology Center and Reproductive service including a reliable system for the long-term Tissue Bank is staffed with highly qualified and preservation of human semen, epididymal aspirate experienced laboratory technologists who are well and testicular tissue. trained in fertility testing and certified by the American Society of Clinical Pathologists (ASCP). Our laboratory is certified by the Clinical Laboratory Improvement Table of Contents Amendments (CLIA) and the Department of Health and Human Services. -

Ejaculation Problems3 9
1 6 Fact Sheet 7 12 2 8 11 Ejaculation Problems3 9 4 10 5 What is ejaculation? 1 Bladder 2 Vas deferens Ejaculation is the release of semen from the penis 3 Urethra at orgasm (sexual climax). When a man is sexually 1 stimulated, the brain sends signals to the genital 6 4 Penis area through nerves in the spinal cord to make the 5 Scrotum 7 12 pelvic muscles contract. 2 8 6 Seminal vesicle 11 7 Rectum At orgasm, waves of muscle contractions transport 3 the sperm, with a small amount of fluid, from the 8 Prostate gland testes through to the vas deferens. The seminal 9 9 Epididymis vesicles and prostate contribute extra fluid to 4 10 Testicle protect the sperm. 10 11 Cowper’s gland 5 This mixture of sperm and fluid (semen) travels 12 Ejaculatory duct along the urethra to the tip of the penis where it is ejaculated (released). What are ejaculation problems? More details about premature ejaculation can be found in a separate1 Bladder Andrology Australia fact Men can experience different kinds of ejaculation sheet. 2 Vas deferens problems, including: 3 Urethra The other ejaculation4 Penis problems are less common • premature ejaculation than premature ejaculation5 Scrotum but can also cause distress for the man and his partner. • retrograde ejaculation 6 Seminal vesicle 7 Rectum • delayed ejaculation (or no ejaculation) What causes ejaculation problems? 8 Prostate gland • painful ejaculation. Ejaculation problems9 Epididymis can have a variety of 10 Testicle How common are ejaculation causes, both physical and psychological. Physical causes include11 Cowper’s some gland illnesses such problems? as diabetes, some 12typesEjaculatory of surgery duct or trauma, some types of inflammation or infection, certain Premature ejaculation is the most common male medicines, and chemical imbalances in the brain sexual problem and affects men of all ages. -

Male Anorgasmia: from “No” to “Go!”
Male Anorgasmia: From “No” to “Go!” Alexander W. Pastuszak, MD, PhD Assistant Professor Center for Reproductive Medicine Division of Male Reproductive Medicine and Surgery Scott Department of Urology Baylor College of Medicine Disclosures • Endo – speaker, consultant, advisor • Boston Scientific / AMS – consultant • Woven Health – founder, CMO Objectives • Understand what delayed ejaculation (DE) and anorgasmia are • Review the anatomy and physiology relevant to these conditions • Review what is known about the causes of DE and anorgasmia • Discuss management of DE and anorgasmia Definitions Delayed Ejaculation (DE) / Anorgasmia • The persistent or recurrent delay, difficulty, or absence of orgasm after sufficient sexual stimulation that causes personal distress Intravaginal Ejaculatory Latency Time (IELT) • Normal (median) à 5.4 minutes (0.55-44.1 minutes) • DE à mean IELT + 2 SD = 25 minutes • Incidence à 2-11% • Depends in part on definition used J Sex Med. 2005; 2: 492. Int J Impot Res. 2012; 24: 131. Ejaculation • Separate event from erection! • Thus, can occur in the ABSENCE of erection! Periurethral muscle Sensory input - glans (S2-4) contraction Emission Vas deferens contraction Sympathetic input (T12-L1) SV, prostate contraction Bladder neck contraction Expulsion Bulbocavernosus / Somatic input (S1-3) spongiosus contraction Projectile ejaculation J Sex Med. 2011; 8 (Suppl 4): 310. Neurochemistry Sexual Response Areas of the Brain • Pons • Nucleus paragigantocellularis Neurochemicals • Norepinephrine, serotonin: • Inhibit libido, -

Sperm Motility Index and Intrauterine Insemination Pregnancy Outcomes
Original Research Sperm Motility Index and Intrauterine Insemination Pregnancy Outcomes Chanel L. Bonds, MD; William E. Roudebush, PhD; and Bruce A. Lessey, MD, PhD From the Department of OB/GYN, Greenville Health System, Greenville, SC, (C.L.B., B.A.L.); De- partment of Biomedical Sciences, University of South Carolina School of Medicine Greenville, Greenville, SC (W.E.R.); and Department of Surgery, Division of Urology, Greenville Health System, Greenville, SC (W.E.R.) Abstract Background: This study determined if sperm motility index affects pregnancy outcome following intrauterine insemination between various ovulation induction protocols. Methods: Calculated sperm motility (determined via computer-assisted semen analyzer) indices were correlated with pregnancy outcomes following intrauterine insemination. Results: Pregnancy rates for different ranges of sperm motility index values showed a trend of in- creasing pregnancy success across increasing ranges of grouped sperm motility index values, but none of these differences between groups was statistically significant. Within the clomid/letrozole cycles, male age differed significantlyP ( = .022) between the pregnant and non-pregnant groups. The difference in sperm motility index between pregnant and non-pregnant groups approached significance P( = .066). Conclusions: A trend exists for an increased pregnancy rate as the sperm motility index approaches 200. Furthermore, our research suggests that as the male partner becomes advanced in age, the chance for getting his partner pregnant declines significantly. ntrauterine insemination (IUI) has been a first- Published pregnancy rates following IUI reveal line treatment for many infertile couples since wide variation. A review article of 18 IUI studies Ithe early 1980s.1 In theory, IUI is successful in revealed a pregnancy rate that ranged from 5% to establishing pregnancy because the procedure 62%.