Final Programme
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Procedure Code List Effective Jan. 1, 2020 for Preauthorization for Blue Cross and Blue Shield of New Mexico Medicare Advantage Members Only
Procedure Code List Effective Jan. 1, 2020 for Preauthorization for Blue Cross and Blue Shield of New Mexico Medicare Advantage Members only Beginning Jan. 1, 2020, providers will be required to obtain preauthorization through Blue Cross and Blue Shield of New Mexico (BCBSNM), Optum, or eviCore for certain procedures for Blue Cross Medicare Advantage members as noted in the MAPD Benefit Preauthorization Procedure Code List, Effective 1/1/2020, below. For members NOT attributed to Optum, preauthorization should be obtained from BCBSNM unless the applicable entry in the MAPD Benefit Preauthorization Procedure Code List references eviCore. For members attributed to Optum, preauthorization should be obtained from Optum, even if the applicable entry in the MAPD Benefit Preauthorization Procedure Code List references eviCore. Any entry that references eviCore should be preauthorized through eviCore except for members attributed to Optum. The member's ID Card will indicate that the member is attributed to Optum. Services performed without benefit preauthorization may be denied for payment in whole or in part, and you may not seek reimbursement from members. Member eligibility and benefits should be checked prior to every scheduled appointment. Eligibility and benefit quotes include membership status, coverage status and other important information, such as applicable copayment, coinsurance and deductible amounts. It is strongly recommended that providers ask to see the member's ID card for current information and a photo ID to guard against medical identity theft. A referral to an out-of-plan or out-of-network provider which is necessary due to network inadequacy or continuity of care must be reviewed by the BCBSNM Utilization Management or DMG (if the member is attributed to DMG this information will be reflected on the ID card) prior to a BCBSNM patient receiving care. -
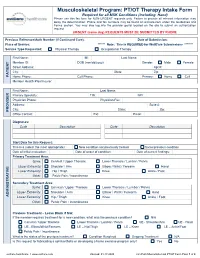
PT/OT Therapy Intake Form Required for All MSK Conditions (Including Hand) Please Use This Fax Form for NON-URGENT Requests Only
Musculoskeletal Program: PT/OT Therapy Intake Form Required for all MSK Conditions (Including Hand) Please use this fax form for NON-URGENT requests only. Failure to provide all relevant information may delay the determination. Phone and fax numbers may be found on eviCore.com under the Guidelines and Forms section. You may also log into the provider portal located on the site to submit an authorization request. URGENT (same day) REQUESTS MUST BE SUBMITTED BY PHONE Previous Reference/Auth Number (If Continued Care): Date of Submission: Place of Service: ****** Note: This is REQUIRED for WellCare Submissions ******* Service Type Requested: Physical Therapy Occupational Therapy First Name: MI: Last Name: Member ID: DOB (mm/dd/yyyy): Gender: Male Female Street Address: Apt #: City: State: Zip: PATIENT Home Phone: Cell Phone: Primary: Home Cell Member Health Plan/Insurer: First Name: Last Name: Primary Specialty: TIN: NPI: Physician Phone: Physician Fax: Address: Suite #: City: State: Zip: PROVIDER Office Contact: Ext: Email: Diagnoses: Code Description Code Description Start Date for this Request: This is a (select the most appropriate): New condition not previously treated Same/previous condition Date of initial evaluation: Date of onset of condition: Date of current findings: Primary Treatment Area: Spine: Cervical / Upper Thoracic Lower Thoracic / Lumbar / Pelvis Upper Extremity: Shoulder / Arm Elbow / Wrist / Forearm Hand Lower Extremity: Hip / Thigh Knee Ankle / Foot Other: Pelvic Pain / Incontinence Secondary Treatment Area: Spine: -
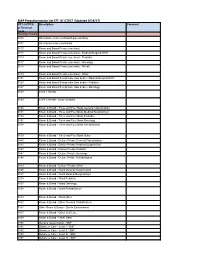
MAP Preauthorization List EFF: 8/1/2017 (Updated 8/24/17)
MAP Preauthorization List EFF: 8/1/2017 (Updated 8/24/17) CPT, HCPCS Description Comment or Revenue Code Revenue Codes 0100 All inclusive room and board plus ancillary 0101 All inclusive room and board 0110 Room and Board Private (one bed) 0111 Room and Board Private (one bed) - Medical/Surgical/GYN 0113 Room and Board Private (one bed) - Pediatric 0117 Room and Board Private (one bed) - Oncology 0118 Room and Board Private (one bed) - Rehab 0119 Room and Board Private (one bed) - Other 0121 Room and Board Semiprivate (two beds) - Medical/Surgical/GYN 0123 Room and Board Semiprivate (two beds) - Pediatric 0127 Room and Board Semiprivate (two beds) - Oncology 0128 Level 1 Rehab 0129 Level 2 Rehab - acute complex 0130 Room & Board - Three and Four Beds General Classification 0131 Room & Board - Three and Four Beds Medical/Surgical/Gyn 0133 Room & Board - Three and Four Beds Pediatric 0137 Room & Board - Three and Four Beds Oncology 0138 Room & Board - Three and Four Beds Rehabilitation 0139 Room & Board - Three and Four Beds Other 0140 Room & Board - Deluxe Private General Classification 0141 Room & Board - Deluxe Private Medical/Surgical/Gyn 0143 Room & Board - Deluxe Private Pediatric 0147 Room & Board - Deluxe Private Oncology 0148 Room & Board - Deluxe Private Rehabilitation 0149 Room & Board - Deluxe Private Other 0150 Room & Board - Ward General Classification 0151 Room & Board - Ward Medical/Surgical/Gyn 0153 Room & Board - Ward Pediatric 0157 Room & Board - Ward Oncology 0158 Room & Board - Ward Rehabilitation 0159 Room & Board - -

114.3 Cmr: Division of Health Care Finance and Policy Ambulatory Care
114.3 CMR: DIVISION OF HEALTH CARE FINANCE AND POLICY AMBULATORY CARE 114.3 CMR 40.00: RATES FOR SERVICES UNDER M.G.L. c. 152, WORKERS’ COMPENSATION ACT Section 40.01: General Provisions 40.02: General Definitions 40.03: Service and Rate Coverage Provisions 40.04: Provisions Affecting Eligible Providers 40.05: Policies for Individual Service Types 40.06: Fees 40.07: Appendices 40.08: Severability 40.01: General Provisions (1) Scope, Purpose and Effective Date. 114.3 CMR 40.00 governs the payment rates effective April 1, 2009 for purchasers of health care services under M.G.L. c. 152, the Workers’ Compensation Act. Payment rates for services provided by hospitals are set forth in 114.1 CMR 41.00. Program policies relating to medical necessity and clinical appropriateness are determined pursuant to M.G.L. c. 152 and 452 CMR 6.00. (2) Coverage. The payment rates set forth in 114.3 CMR 40.06 are full payment for services provided under M.G.L. c. 152, § 13, including any related administrative or overhead costs. The insurer, employer and health care service provider may agree upon a different payment rate for any service set forth in the fee schedule in 114.3 CMR 40.00. No employee may be held liable for the payment for health care services determined compensable under M.G.L. c. 152, § 13. (3) Administrative Bulletins. The Division may issue administrative bulletins to clarify substantive provisions of 114.3 CMR 40.00, or to publish procedure code updates and corrections. For coding updates and correction, the bulletin will list: (a) new code numbers for existing codes, with the corresponding cross references between existing and new codes numbers; (b) deleted codes for which there are no corresponding new codes; and (c) codes for entirely new services that require pricing. -

Artificial Finger Joint Replacement Due to a Giant Cell Tumor of the Tendon Sheath with Bone Destruction: a Case Report
3502 ONCOLOGY LETTERS 10: 3502-3504, 2015 Artificial finger joint replacement due to a giant cell tumor of the tendon sheath with bone destruction: A case report HUI LU, HUI SHEN, QIANG CHEN, XIANG-QIAN SHEN and SHOU-CHENG WU Department of Hand Surgery, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, Zhejiang 310003, P.R. China Received October 24, 2014; Accepted September 25, 2015 DOI: 10.3892/ol.2015.3813 Abstract. The current study presents the case of a 25-year-old excised completely and the function of the joints was recov- male who developed tumor recurrence of the proximal ered. phalange of the ring finger on the right hand 4 years after partial tumor resection surgery. An X-ray of the right hand Case report showed that the distal bone of the proximal phalange on the ring finger was destroyed. An artificial finger joint replace- A 25-year-old male was admitted to The First Affiliated ment was performed using a silicone joint for this unusual Hospital, College of Meicine, ZheJiang University (Hangzhou, tumor recurrence. The pathological findings were indicative of Zhejiang, China) with tumor recurrence of the proximal a giant cell tumor of the tendon sheath. As a result of surgery, phalange of the ring finger on the right hand 4 years after the patient's proximal interphalangeal point motion recovered partial tumor resection surgery. The patient had no history to the pre-operative level. The pre-operative and post-operative of trauma or infection and was previously healthy. A physical disabilities of the arm, at shoulder and hand and total activity examination revealed swelling of the proximal phalange of the measurement values were 1.67 and 3.33, and 255 and 243˚, finger without clear cause, multiple nodules in the local areas respectively. -
Final Scientific Programme Revised
SICOT/SIROT 2008 XXIV Triennial World Congress Scientific Programme 24-28 August 2008 Hong Kong Convention and Exhibition Centre Hong Kong, China 1 Programme Colour Key SICOT - Spine SICOT - Joint SICOT - Sports Medicine SICOT - Paediatrics SICOT - Foot & Ankle SICOT - Trauma SICOT - Tumours SICOT - Hand & Wrist SICOT - Shoulder & Elbow SICOT - Basic Science SICOT - General Orthopaedics SIROT Participating Associations and Societies 2 Sunday, 24 August 2008 Theatre 1 Theatre 2 Grand Hall 08:00 Free Papers Free Papers -09:00 SIROT: Biomechanics SIROT: Osteoporosis 09:00 Free Papers Free Papers -10:30 SIROT: Infections SIROT: Joint Replacement Break 11:00 Free Papers Free Papers -12:00 SIROT: Fracture Healing SIROT: Tissue Engineering 12:00 Free Papers Free Papers -13:00 SIROT: Infections / SIROT: Tumours Tissue Engineering Lunch 14:00 SICOT/SIROT -16:45 Research Commission: Stem Cells and Orthopaedics 17:30 SICOT Opening Ceremony -19:00 Sunday, 24 August 2008 Theatre 1 08:00-09:00 Free Papers – SIROT: Biomechanics Moderator : Ping-Chung LEUNG (Hong Kong) 18395 RADIOSTEREOMETRIC ANALYSIS (RSA) OF THREE-DIMENSIONAL MICROMOTION IN A FRACTURE MODEL OF FEMUR Saravana Vail KARUPPIAH, Martin DOWNING, George P. ASHCROFT, Alan J. JOHNSTONE, Blair ASHCROFT (United Kingdom) 18359 SUTURE ANCHORS FOR BANKART REPAIR REVISITED Ilias BISBINAS, Petros MIKALEF, Evangelos MAGNISSALIS, Theodoros BESLIKAS, Ioannis CHRISTOFORIDIS (Greece) 18270 INFLUENCE OF A SINGLE SHAFT ANGLE-STABLE SCREW IN OSTEOPOROTIC DISTAL RADIUS FRACTURES TREATED WITH VOLAR FIXED-ANGLE -
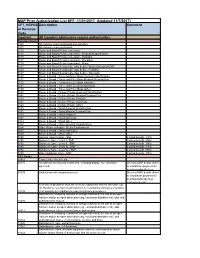
MAP Prior Authorization List EFF: 11/01/2017 (Updated 11/7/2017)
MAP Prior Authorization List EFF: 11/01/2017 (Updated 11/7/2017) CPT, HCPCS Description Comment or Revenue Code Inpatient All Inpatient admissions require authorization Revenue Codes 0100 All inclusive room and board plus ancillary 0101 All inclusive room and board 0110 Room and Board Private (one bed) 0111 Room and Board Private (one bed) - Medical/Surgical/GYN 0113 Room and Board Private (one bed) - Pediatric 0117 Room and Board Private (one bed) - Oncology 0119 Room and Board Private (one bed) - Other 0121 Room and Board Semiprivate (two beds) - Medical/Surgical/GYN 0123 Room and Board Semiprivate (two beds) - Pediatric 0127 Room and Board Semiprivate (two beds) - Oncology 0130 Room & Board - Three and Four Beds General Classification 0131 Room & Board - Three and Four Beds Medical/Surgical/Gyn 0133 Room & Board - Three and Four Beds Pediatric 0137 Room & Board - Three and Four Beds Oncology 0139 Room & Board - Three and Four Beds Other 0140 Room & Board - Deluxe Private General Classification 0141 Room & Board - Deluxe Private Medical/Surgical/Gyn 0143 Room & Board - Deluxe Private Pediatric 0147 Room & Board - Deluxe Private Oncology 0149 Room & Board - Deluxe Private Other 0150 Room & Board - Ward General Classification 0151 Room & Board - Ward Medical/Surgical/Gyn 0153 Room & Board - Ward Pediatric 0157 Room & Board - Ward Oncology 0159 Room & Board - Ward Other 0160 Room & Board - Other General Classification 0164 Other Room & Board - Sterile Environment 0167 Room & Board - Other Self Care 0169 Room & Board - Other Other 0190 General -

Facts Around the Saddle Joint (CMC1 Joint) Instructional Course SGH 17.09.2020
Facts around the saddle joint (CMC1 joint) Instructional Course SGH 17.09.2020 Esther Vögelin, MD, Prof Hand Surgery and Surgery of Peripheral Nerves Anatomy • Thumb • STT and midcarpal joints • CMC joint • MCP joint • IP joint Anatomy • How many trapezial articulations? • Two more important joints: 2 - Scaphotrapezoidal joint (5) 3 - MCP joint 1 5 4 • Skeletal Radiol 2015;44:165-77 Anatomy • Two opposing saddles à wide range of motion • Skeletal Radiol 2015;44:165-77 Anatomy • Stability à 3 main ligament complexes • Palmar (anterior)[2]: • AOL („beak“), ulnar collateral • Dorsal (posterior)[3]: • POL, DRL • Intermetacarpal [2] • Skeletal Radiol 2015;44:165-77 Radiology • Robert‘s view (pa), oblique, lateral Staging Stages Radiological disease change 1 Slight widening of joint space, < 1/3 subluxation of joint 2 <2mm osteophytes present, 1/3 subluxation of joint 3 >2mm osteophytes present, > 1/3 subluxation of joint, joint space narrowing 4 Erosion of scaphotrapezial joint, significant joint space narrowing, major subluxation of joint Early stage treatment • Stabilization of CMC joint • Synovectomy • CMC joint alignement • CMC joint arthroscopy à debridement, synovectomy, electrothermal shrinkage of ligaments - Normal radiographs, - Restricted painful mobility • J AM Acad Orthop Surg 2008;16(3):140-51 Early stage treatment • Ligament reconstruction for stabilization of the CMC joint - Littler Eaton procedure: ½ FCR à AOL, intermetacarpal, dorsoradial ligaments J Bone Joint Surg Am 1973;55(8):1655-66 J Hand Surg Am 2000;25(2):297-304 - Brunelli procedure: APL Tendon à 1st and 2nd MC J Hand Surg Br Vol 1989;14B:209-212 - Pechlaner technique: ECRL strip through 1st MC and trapezium Pechlaner S. -

Three-Ligament Tenodesis” Procedure Restore Carpal Architecture in Static Chronic Scapholunate Dissociation ?
Acta Orthop. Belg., 2013, 79, 271-274 ORIGINAL STUDY Does the “three-ligament tenodesis” procedure restore carpal architecture in static chronic scapholunate dissociation ? Luc DE SMET, Sofie GOEMINNE, Ilse DEGREEF From the University Hospitals Leuven, Pellenberg, Belgium The effect of the three-ligament tenodesis on the angle on the lateral view (normally between 45 and scapholunate angle and scapholunate gap was stud- 60°). Both parameters assess the SL malalignment ied. A comparison was made between these angles in patients before surgery. Procedures such as sca- preoperatively and postoperatively in 12 patients. photrapeziotrapezoid (STT) arthrodesis (15) and the There was a significant decrease in the scapholunate original Brunelli procedure (3) concentrate on re- angle from 77 to 68°, and the scapholunate gap was ducing the SL angle without addressing the SL gap. reduced from 4.25 mm to 3.29 mm. We also studied the correlation between scapholunate angle and When rotatory disassociation is seen, some at- scapholunate gap postoperatively in a cohort of 25 pa- tenuation of extrinsic ligaments must have occurred. tients and found a significant correlation. This was the rationale for the flexor carpi radialis This suggests that the principle of the procedure is (FCR) tenodesis described by Brunelli and correct, but the aims are not fully achieved, and that Brunelli (3). A distally based strip of the FCR is the procedure has a similar effect on SL gap and SL passed through a drill hole through the scaphoid and angle. fixed on the dorsal rim of the distal radius. Later Keywords : wrist ; scapholunate ; carpus ; instability ; Van den Abbeele et al (14) and Garcia-Elias et ligamentoplasty ; Brunelli ; DISI. -

184591/2021/Estt-Ne Hr
168 184591/2021/ESTT-NE_HR PUSHPAWATI SINGHANIA HOSPITAL & RESEARCH INSTITUTE A MULTISPECIALITY HOSPITAL (formally known as Puspawati Singhania Research Institute for liver,Renal & Digestive Diseases) (w.e.f. 01.04.2020) OPD CHARGES FEES (Rs) SR. NO. CONSULTANT NAME FIRST SUBS. GASTROENTEROLOGY 1PROF.(DR). R.K.TANDON 20001500 2LT. COL. (DR) ARUN KUMAR 12001200 3DR. DINESH SINGHAL 10001000 4DR. MANOJ KUMAR 10001000 5DR. NRIPEN SAIKIA 10001000 6DR. RAJIV BAIJAL 10001000 7DR. RAHUL GUPTA 20002000 8DR. SHUBHAM VATSYA 900900 SURGICAL GASTROENTEROLOGY & LIVER TRANSPLANT 1DR. K.R VASUDEVAN 12001200 2DR. MANOJ GUPTA 10001000 3DR. BHUSHAN P. BHOLA 12001200 NEPHROLOGY 1DR. SANJEEV SAXENA 12001200 2DR. RAVI BANSAL 10001000 3DR. RAJESH GOEL 800800 UROLOGY 1DR. P.P.SINGH 12001200 2DR. JAGDEEP BALYAN 11001100 3DR. A.S.MALHOTRA 11001100 CARDIOLOGIST 1DR. T.S.KLER 10001000 2DR. VINAYAK AGRAWAL 12001200 3DR. AVINASH VERMA 10001000 4DR. S. N. PATHAK 10001000 5DR. ABHINAV AGGARWAL 10001000 CARDIO SURGERY 1DR. BALRAM AIRAN 10001000 2DR. VIJAY MOHAN KOHLI 12501250 3DR GAURAV GUPTA 10001000 NEUROLOGOY 1DR. SHAMSHER DWIVEDEE 20001800 NEURO SURGERY 1DR. SUMIT GOYAL 10001000 ENDOCRINOLOGY 1DR. MONIKA SHARMA 1001000 PULMONOLOGY 1DR. G.C. KHILNANI 15001500 2DR. NEETU JAIN 10001000 G.I SURGERY 1DR. SANJAY CHAUREY 15001500 2DR. RAJEEV KHANNA 12001000 3DR. HARISH KAPILA 15001500 ONCOLOGY (SURGERY) 1DR. ARVIND KUMAR 15001500 2DR. SALEEM NAYAK 15001500 3DR. VIVEK GUPTA 15001500 4DR. VIKRANT SHARMA 15001500 ONCOLOGY 1DR. AMISH VORA 15001500 2DR. AMIT UPADHYAY 15001500 ORTHOPEDICS 1DR. P.P. KOTWAL 15001500 2DR. GAURAV PRAKASH BHARDWAJ 12001200 Page 1 169 184591/2021/ESTT-NE_HR 3DR. U.K.SADHOO 12001200 4DR. G.S.TUCKER 12001200 5DR. ANIL MISHRA 10001000 6DR. -

Radio-Luno-Triquetral Bone-Ligament Transfer As an Additional Stabilizer
Archives of Orthopaedic and Trauma Surgery https://doi.org/10.1007/s00402-020-03690-2 HANDSURGERY Radio‑luno‑triquetral bone‑ligament transfer as an additional stabilizer in scapholunate‑instability Luzian C. P. Haug1 · Tom Adler1 · Dietmar Bignion1 · Esther Voegelin1 Received: 23 April 2020 / Accepted: 11 November 2020 © The Author(s) 2020 Abstract Introduction Reconstruction of the scapho-lunate (SL) ligament is still challenging. Many diferent techniques, such as capsulodesis, tendon graft and bone-ligament-bone graft have been described to stabilize reducible SL dissociation. If primary ligament repair alone is not possible, an additional stabilizer is needed to achieve scapho-lunate stability. A new local bone-ligament transfer using half of the radio-luno-triquetral ligament is performed. The direction of traction of the transposed ligament is very similar to the original ligament. Ideal tension can be attained by fxation of the bone block at the dorsal ridge of the scaphoid. The biomechanical stability of this bone-ligament transfer shall be examined biomechanically. Material and methods Computed tomography imaging was performed using eight cadaveric forearms with a defned posi- tion of the wrist. Axial load was accomplished with tension springs attached to the extensor and fexor tendons. Three series ([a] native, [b] divided SL ligament and [c]) after reconstruction with bone-ligament transfer] were reconstructed three- dimensionally to determine the angles between radius, scaphoid and lunate. The radial distal part including a bone fragment of the radio-luno-triquetral ligament was transferred from its insertion at the distal edge of the radius to be attached to the dorsal ridge of the scaphoid. -

Sentinel Report Cder Mpl1r Wp155
Disclaimer The following report(s) provides findings from an FDA‐initiated query using Sentinel. While Sentinel queries may be undertaken to assess potential medical product safety risks, they may also be initiated for various other reasons. Some examples include determining a rate or count of an identified health outcome of interest, examining medical product use, exploring the feasibility of future, more detailed analyses within Sentinel, and seeking to better understand Sentinel capabilities. Data obtained through Sentinel are intended to complement other types of evidence such as preclinical studies, clinical trials, postmarket studies, and adverse event reports, all of which are used by FDA to inform regulatory decisions regarding medical product safety. The information contained in this report is provided as part of FDA’s commitment to place knowledge acquired from Sentinel in the public domain as soon as possible. Any public health actions taken by FDA regarding products involved in Sentinel queries will continue to be communicated through existing channels. FDA wants to emphasize that the fact that FDA has initiated a query involving a medical product and is reporting findings related to that query does not mean that FDA is suggesting health care practitioners should change their prescribing practices for the medical product or that patients taking the medical product should stop using it. Patients who have questions about the use of an identified medical product should contact their health care practitioners. The following report contains a description of the request, request specifications, and results from the modular program run(s). If you are using a web page screen reader and are unable to access this document, please contact the Sentinel Operations Center for assistance at [email protected].