Diverticulitis of the Appendix: Farminqton, CI 06032, USA, Tel: 305-321-4413; Email
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Print This Article
International Surgery Journal Lew D et al. Int Surg J. 2021 May;8(5):1575-1578 http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902 DOI: https://dx.doi.org/10.18203/2349-2902.isj20211831 Case Report Acute gangrenous appendicitis and acute gangrenous cholecystitis in a pregnant patient, a difficult diagnosis: a case report David Lew, Jane Tian*, Martine A. Louis, Darshak Shah Department of Surgery, Flushing Hospital Medical Center, Flushing, New York, USA Received: 26 February 2021 Accepted: 02 April 2021 *Correspondence: Dr. Jane Tian, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Abdominal pain is a common complaint in pregnancy, especially given the physiological and anatomical changes that occur as the pregnancy progresses. The diagnosis and treatment of common surgical pathologies can therefore be difficult and limited by the special considerations for the fetus. While uncommon in the general population, concurrent or subsequent disease processes should be considered in the pregnant patient. We present the case of a 36 year old, 13 weeks pregnant female who presented with both acute appendicitis and acute cholecystitis. Keywords: Appendicitis, Cholecystitis, Pregnancy, Pregnant INTRODUCTION population is rare.5 Here we report a case of concurrent appendicitis and cholecystitis in a pregnant woman. General surgeons are often called to evaluate patients with abdominal pain. The differential diagnosis list must CASE REPORT be expanded in pregnant woman and the approach to diagnosing and treating certain diseases must also be A 36 year old, 13 weeks pregnant female (G2P1001) adjusted to prevent harm to the fetus. -

Umbilical Hernia with Cholelithiasis and Hiatal Hernia
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Springer - Publisher Connector Yamanaka et al. Surgical Case Reports (2015) 1:65 DOI 10.1186/s40792-015-0067-8 CASE REPORT Open Access Umbilical hernia with cholelithiasis and hiatal hernia: a clinical entity similar to Saint’striad Takahiro Yamanaka*, Tatsuya Miyazaki, Yuji Kumakura, Hiroaki Honjo, Keigo Hara, Takehiko Yokobori, Makoto Sakai, Makoto Sohda and Hiroyuki Kuwano Abstract We experienced two cases involving the simultaneous presence of cholelithiasis, hiatal hernia, and umbilical hernia. Both patients were female and overweight (body mass index of 25.0–29.9 kg/m2) and had a history of pregnancy and surgical treatment of cholelithiasis. Additionally, both patients had two of the three conditions of Saint’s triad. Based on analysis of the pathogenesis of these two cases, we consider that these four diseases (Saint’s triad and umbilical hernia) are associated with one another. Obesity is a common risk factor for both umbilical hernia and Saint’s triad. Female sex, older age, and a history of pregnancy are common risk factors for umbilical hernia and two of the three conditions of Saint’s triad. Thus, umbilical hernia may readily develop with Saint’s triad. Knowledge of this coincidence is important in the clinical setting. The concomitant occurrence of Saint’s triad and umbilical hernia may be another clinical “tetralogy.” Keywords: Saint’s triad; Cholelithiasis; Hiatal hernia; Umbilical hernia Background of our knowledge, no previous reports have described the Saint’s triad is characterized by the concomitant occur- coexistence of umbilical hernia with any of the three con- rence of cholelithiasis, hiatal hernia, and colonic diverticu- ditions of Saint’s triad. -

ACUTE Yellow Atrophy Ofthe Liver Is a Rare Disease; Ac
ACUTE YELLOW ATROPHY OF THE LIVER AS A SEQUELA TO APPENDECTOMY.' BY MAX BALLIN, M.D., OF DETROIT, MICHIGAN. ACUTE yellow atrophy of the liver is a rare disease; ac- cording to Osler about 250 cases are on record. This affection is also called Icterus gravis, Fatal icterus, Pernicious jaundice, Acute diffuse hepatitis, Hepatic insufficiency, etc. Acute yellow atrophy of the liver is characterized by a more or less sudden onset of icterus increasing to the severest form, headaches. insomnia, violent delirium, spasms, and coma. There are often cutaneous and mucous hiemorrhages. The temperature is usually high and irregular. The pulse, first normal, later rapid; urine contains bile pigments, albumen, casts, and products of incomplete metabolism of albumen, leucin, and tyrosin, the pres- ence of which is considered pathognomonic. The affection ends mostly fatally, but there are recoveries on record. The findings of the post-mortem are: liver reduced in size; cut surface mot- tled yellow, sometimes with red spots (red atrophy), the paren- chyma softened and friable; microscopically the liver shows biliary infiltration, cells in all stages of degeneration. Further, we find parenchymatous nephritis, large spleen, degeneration of muscles, haemorrhages in mucous and serous membranes. The etiology of this affection is not quite clear. We find the same changes in phosphorus poisoning; many believe it to be of toxic origin, but others consider it to be of an infectious nature; and we have even findings of specific germs (Klebs, Tomkins), of streptococci (Nepveu), staphylococci (Bourdil- lier), and also the Bacillus coli is found (Mintz) in the affected organs. The disease seems to occur always secondary to some other ailment, and is observed mostly during pregnancy (about one-third of all cases, hence the predominance in women), after Read before the Wayne County Medical Society, January 5, I903. -

Diverticulosis Beyond the Basics.Xps
Patient education: Diverticular disease (Beyond the Basics) - UpToDate Page 1 of 10 Official reprint from UpToDate® www.uptodate.com ©2017 UpToDate® The content on the UpToDate website is not intended nor recommended as a substitute for medical advice, diagnosis, or treatment. Always seek the advice of your own physician or other qualified health care professional regarding any medical questions or conditions. The use of UpToDate content is governed by the UpToDate Terms of Use. ©2017 UpToDate, Inc. All rights reserved. Patient education: Diverticular disease (Beyond the Basics) Author: John H Pemberton, MD Section Editor: J Thomas Lamont, MD Deputy Editor: Shilpa Grover, MD, MPH All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Dec 2016. | This topic last updated: Sep 16, 2015. DIVERTICULAR DISEASE OVERVIEW — A diverticulum is a pouch-like structure that can form through points of weakness in the muscular wall of the colon (ie, at points where blood vessels pass through the wall) (figure 1). Diverticulosis affects men and women equally. The risk of diverticular disease increases with age. It occurs throughout the world but is seen more commonly in developed countries. WHAT IS DIVERTICULAR DISEASE? Diverticulosis — Diverticulosis merely describes the presence of diverticula. Diverticulosis is often found during a test done for other reasons, such as flexible sigmoidoscopy, colonoscopy, or barium enema. Most people with diverticulosis have no symptoms and will remain symptom free for the rest of their lives. (See 'Diverticular disease prognosis' below.) A person with diverticulosis may have diverticulitis, or diverticular bleeding. -

Diverticular Abscess Presenting As a Strangulated Inguinal Hernia: Case Report and Review of the Literature
Ulster Med J 2007; 76 (2) 107-108 Presidential Address 107 Case Report Diverticular Abscess Presenting as a Strangulated Inguinal Hernia: Case Report and review of the literature. S Imran H Andrabi, Ashish Pitale*, Ahmed AS El-Hakeem Accepted 22 December 2006 ABSTRACT noted nausea, anorexia and increasing abdominal pain. She had no previous history of any surgery or trauma and was on Potentially life threatening diseases can mimic a groin hernia. warfarin for atrial fibrillation. We present an unusual case of diverticulitis with perforation and a resulting abscess presenting as a strangulated inguinal hernia. The features demonstrated were not due to strangulation of the contents of the hernia but rather pus tracking into the hernia sac from the peritoneal cavity. The patient underwent sigmoid resection and drainage of retroperitoneal and pericolonic abscesses. Radiological and laboratory studies augment in reaching a diagnosis. The differential diagnosis of inguinal swellings is discussed. Key Words: Diverticulitis, diverticular perforation, diverticular abscess, inguinal hernia INTRODUCTION The association of complicated inguinal hernia and diverticulitis is rare1. Diverticulitis can present as left iliac fossa pain, rectal bleeding, fistulas, perforation, bowel obstruction and abscesses. Our patient presented with a diverticular perforation resulting in an abscess tracking into the inguinal canal and clinically masquerading as a Fig 2. CT scan showing inflammatory changes with strangulated inguinal hernia. The management warranted an stranding of the subcutaneous fat in the left groin and a exploratory laparotomy and drainage of pus. large bowel diverticulum CASE REPORT On admission, she had a tachycardia (pulse 102 beats/min) and a temperature of 37.5OC. -

Diverticular Disease of the Colon
® ® GasTroenTerology DepArTmenT Diverticular Disease of the Colon WHAT is DiverTiculosis? Diverticulosis refers to the presence of small out-pouchings (called diverticula) or sacs that can develop in the lining of the gastrointestinal tract. While diverticula can be present anywhere in the entire digestive tract, they are most common on the left side of the large intestine, the area known as the descending and sigmoid colon (Figure 1). HoW common is DiverTiculosis? Diverticulosis is a common disorder especially in older people. The condition is rarely seen in people under the age of 30 and is most common in those over 60. Both men and women are equally affected. What cAuses DiverTiculosis? Figure 1 No one knows for certain why diverticulosis develops; however, a few theories have been suggested. Some experts believe that abnormal contraction and spasm (resulting in intermittent high pressure in the colon) may cause diverticula to form in a weak spot of the intestinal wall. Low fiber diets may play a role in the development of diverticulosis. In rural Africa where diet is high in roughage, diverticulosis is rare. There also appears to be a genetic predisposition to diverticulosis, that is, if your parent or grandparent had diverticulosis you may develop it as well. What Are the sympToms of DiverTiculosis Most patients with diverticulosis have no symptoms. Many will never know they have the condition until it is discovered during an endoscopic or radiographic (X-ray) examination. While most people have no symptoms, some individuals may experience pain or discomfort in the left lower abdomen, bloating, and/or change in bowel habits. -

Case Report Perforated Acute Appendicitis Misdiagnosed As Colonic Perforation in Colon Cancer Patients After Colonoscopy: a Report of Two Cases and Literature Reviews
Int J Clin Exp Pathol 2017;10(6):7256-7260 www.ijcep.com /ISSN:1936-2625/IJCEP0050313 Case Report Perforated acute appendicitis misdiagnosed as colonic perforation in colon cancer patients after colonoscopy: a report of two cases and literature reviews Kaiyuan Zheng, Ji Wang, Wenhao Lv, Yongjia Yan, Zhicheng Zhao, Weidong Li, Weihua Fu Department of General Surgery, Tianjin Medical University General Hospital, Tianjin 300052, China Received January 23, 2017; Accepted May 9, 2017; Epub June 1, 2017; Published June 15, 2017 Abstract: Free gas in the abdominal cavity usually indicates that the perforation of the gastrointestinal tract from many factors including perforated ulcer, tumor perforation and severe infection, etc. But the pneumoperitoneum in perforated acute appendix secondary to the colonoscopy was rare relative. We reported two colon cancer patients with signs of abdominal free air after the operation of colonoscopy, considered the diagnosis of colon perforation at first, but eventually they were confirmed as perforated appendicitis. This report highlights that purulent perforated appendicitis should be considered especially for elderly patients with colon tumor presenting as signs of pneumo- peritoneum after the endoscopic operation. Keywords: Pneumoperitoneum, perforated appendicitis, colon cancer perforation, colonoscopy Introduction Acute perforated appendicitis is one of the common causes of acute abdomen and is Pneumoperitoneum is defined as free gas ap- needed emergency surgery. Its incidence was pears in the abdominal cavity, is usually caused higher in elderly population [6]. However, acute by the perforation of the alimentary tract sec- appendicitis following the operation of colonos- ondary to pathological or iatrogenic factors, but copy as a rare complication, with a consider- caused by purulent perforated appendix was ed incidence of 0.038%, and the appendix is rare relative. -

Crohn's Disease Manifesting As Acute Appendicitis: Case Report and Review of the Literature
Case Report World Journal of Surgery and Surgical Research Published: 20 Jan, 2020 Crohn's Disease Manifesting as Acute Appendicitis: Case Report and Review of the Literature Terrazas-Espitia Francisco1*, Molina-Dávila David1, Pérez-Benítez Omar2, Espinosa-Dorado Rodrigo2 and Zárate-Osorno Alejandra3 1Division of Digestive Surgery, Hospital Español, Mexico 2Department of General Surgery Resident, Hospital Español, Mexico 3Department of Pathology, Hospital Español, Mexico Abstract Crohn’s Disease (CD) is one of the two clinical presentations of Inflammatory Bowel Disease (IBD) which involves the GI tract from the mouth to the anus, presenting a transmural pattern of inflammation. CD has been described as being a heterogenous disorder with multifactorial etiology. The diagnosis is based on anamnesis, physical examination, laboratory finding, imaging and endoscopic findings. There have been less than 200 cases of Crohn’s disease confined to the appendix since it was first described by Meyerding and Bertram in 1953. We present the case of a 24 year old male, who presented with acute onset, right lower quadrant pain, mimicking acute appendicitis with histopathological report of Crohn’s disease confined to the appendix. Introduction Crohn’s Disease (CD) is a chronic entity which clinical diagnosis represents one of the two main presentations of Inflammatory Bowel Disease (IBD), and it occurs throughout the gastrointestinal tract from the mouth to the anus, presenting a transmural pattern of inflammation of the gastrointestinal wall and non-caseating small granulomas. The exact origin of the disease remains OPEN ACCESS unknown, but it has been proposed as an interaction of genetic predisposition, environmental risk *Correspondence: factors and immune dysregulation of intestinal microbiota [1,2]. -

MANAGEMENT of ACUTE ABDOMINAL PAIN Patrick Mcgonagill, MD, FACS 4/7/21 DISCLOSURES
MANAGEMENT OF ACUTE ABDOMINAL PAIN Patrick McGonagill, MD, FACS 4/7/21 DISCLOSURES • I have no pertinent conflicts of interest to disclose OBJECTIVES • Define the pathophysiology of abdominal pain • Identify specific patterns of abdominal pain on history and physical examination that suggest common surgical problems • Explore indications for imaging and escalation of care ACKNOWLEDGEMENTS (1) HISTORICAL VIGNETTE (2) • “The general rule can be laid down that the majority of severe abdominal pains that ensue in patients who have been previously fairly well, and that last as long as six hours, are caused by conditions of surgical import.” ~Cope’s Early Diagnosis of the Acute Abdomen, 21st ed. BASIC PRINCIPLES OF THE DIAGNOSIS AND SURGICAL MANAGEMENT OF ABDOMINAL PAIN • Listen to your (and the patient’s) gut. A well honed “Spidey Sense” will get you far. • Management of intraabdominal surgical problems are time sensitive • Narcotics will not mask peritonitis • Urgent need for surgery often will depend on vitals and hemodynamics • If in doubt, reach out to your friendly neighborhood surgeon. Septic Pain Sepsis Death Shock PATHOPHYSIOLOGY OF ABDOMINAL PAIN VISCERAL PAIN • Severe distension or strong contraction of intraabdominal structure • Poorly localized • Typically occurs in the midline of the abdomen • Seems to follow an embryological pattern • Foregut – epigastrium • Midgut – periumbilical • Hindgut – suprapubic/pelvic/lower back PARIETAL/SOMATIC PAIN • Caused by direct stimulation/irritation of parietal peritoneum • Leads to localized -

Problems in Family Practice Acute Abdominal Pain in Children
dysuria. The older child may start bed wetting with or without dysuria. A problems in Family Practice drop of fresh, clean unspun urine will usually reveal pyuria, but in the early case relatively few white blood cells may be seen compared to gross bacillu- Acute Abdominal Pain ria. The infection may have underlying urinary tract abnormality, stone, in Children hydronephrosis, polycystic kidney or renal neoplasms. The IVP is important Hyman Shrand, M D in detecting these underlying prob lems. Cambridge, M assachusetts 4. Viral Hepatitis. Malaise, anorexia, abdominal pain, and tenderness over Acute abdominal pain in children is a common and challenging prob the liver occur with hepatitis A or B. lem for the family physician. The many causes of this problem require Later, patients who become jaundiced a systematic approach to making the diagnosis and planning specific have dark urine and pale stools. In therapy. A careful history and physical examination, together with a teenagers, “needle tracks” suggest sy ringe transmitted Type B (H.A.A.) small number of selected laboratory studies, provide a rational basis hepatitis. Youngsters with infectious for effective management in most cases. This paper reviews the more mononucleosis may present as hepati common causes of acute abdominal pain in children with special em tis. phasis on their clinical differentiation. 5. Upper Respiratory Tract. Strepto coccal pharyngitis, a common cause of Abdominal pain in a child is always followed by vomiting is more likely an vomiting and abdominal pain, can be an emergency. The primary physician intra-abdominal disorder. recognized by looking at the throat must identify a “medical” cause in or with confirmatory throat culture. -
Diverticulitis of the Appendix
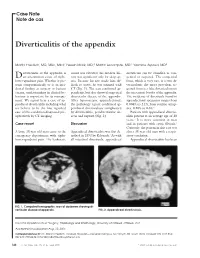
Case Note Note de cas Diverticulitis of the appendix Martin Friedlich, MD, MSc, MEd;* Neesh Malik, MD;† Martin Lecompte, MD;† Yasmine Ayroud, MD‡ iverticulitis of the appendix is count was elevated; his medical his- diverticula can be classified as con- Dan uncommon cause of right- tory was significant only for sleep ap- genital or acquired. The congenital lower-quadrant pain. Whether it pre- nea. Because his size made him dif- form, which is very rare, is a true di- sents symptomatically or is an inci- ficult to assess, he was scanned with verticulum; the more prevalent ac- dental finding at surgery or barium CT (Fig. 1). The scan confirmed ap- quired form is a false diverticulum on enema, understanding its clinical be- pendicitis, but also showed suspected the mesenteric border of the appendix. haviour is important for its manage- diverticular disease of the appendix. The incidence of diverticula found in ment. We report here a case of ap- After laparoscopic appendectomy, appendectomy specimens ranges from pendiceal diverticulitis including what the pathology report confirmed ap- 0.004% to 2.1%; from routine autop- we believe to be the first reported pendiceal diverticulosis complicated sies, 0.20% to 0.6%.2 case of this condition diagnosed pre- by diverticulitis, peridiverticular ab- Patients with appendiceal divertic- operatively by CT imaging. scess and rupture (Fig. 2). ulitis present at an average age of 38 years.3 It is more common in men Case report Discussion and in patients with cystic fibrosis.2 Curiously, the patient in this case was A large 38-year-old man came to the Appendiceal diverticulitis was first de- also a 38-year-old man with a respir- emergency department with right- scribed in 1893 by Kelynack.1 As with atory condition. -

Assessment of Small Bowel Obstruction in Patients Following Appendicitis: an Institutional Based Study
Original Research Article. Assessment of Small Bowel Obstruction in Patients Following Appendicitis: An Institutional Based Study Atahussain Poonawala1, Nilofer Poonawala2* 1Assistant Professor, Department of General Surgery, Vedantaa Institute of Medical Sciences, Palghar, Maharashtra, India. 2Assistant Professor, Department of Obstetrics and Gynaecology, Vedantaa Institute of Medical Sciences, Palghar, Maharashtra, India. ABSTRACT Background: Small bowel obstruction (SBO) is a pathological may be seen in few cases of appendectomy. condition which occurs when the intestinal contents are prevented from moving along the length of the intestine. The Key words: Appendectomy, Phlegmonous, Small Bowel present study was conducted to assess the cases of small Obstruction. bowel obstruction following appendectomy. *Correspondence to: Materials & Methods: The present study was conducted on Dr. Nilofer Poonawala, 42 cases of appendicitis of both genders. In all patients, Assistant Professor, laparoscopic appendectomy was planned. Patients were Department of Obstetrics and Gynaecology, recalled to note any kind of complication arising from the Vedantaa Institute of Medical Sciences, procedure. Palghar, Maharashtra, India. Results: Out of 42 patients, males were 26 and females were Article History: 16. Age group 20-30 years had 5 males and 3 females, 30-40 Received: 28-11-2019, Revised: 25-12-2019, Accepted: 21-01-2020 years had 9 males and 5 females and 40-50 years had 12 Access this article online males and 8 females. The difference was significant (P< 0.05). Website: Quick Response code Macroscopic feature of appendix during procedure was www.ijmrp.com phlegmonous in 12 and gangrenous in 30 cases. The DOI: difference was significant (P< 0.05). 10.21276/ijmrp.2020.6.1.016 Conclusion: Small bowel obstruction is a complication which INTRODUCTION Appendectomy is one of the most common procedures performed Intestinal obstruction is most commonly caused by intra- which may be due to appendicitis or frequent pain in appendix.