Download Download
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Punjab Roads Component
Due Diligence Report on Social Safeguards Loan 3264-PAK: Flood Emergency Reconstruction and Resilience Project (FERRP)–Punjab Roads Component Due Diligence Report on Social Safeguards on Reconstruction of Pasrur – Narowal Road March 2017 Prepared by: Communication and Works Department, Government of the Punjab NOTES (i) The fiscal year (FY) of the Government of the Islamic Republic of Pakistan and its agencies ends on 30 June. (ii) In this report, "$" refers to US dollars. This Social Safeguards due diligence report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. Social Due Diligence Report Document stage: Final Date: March, 2017 PAK: Flood Emergency Reconstruction and Resilience Project, Loan No. 3264 Social Due Diligence Report of Reconstruction of 28 km long Pasrur – Narowal Road from RD 0+000 to RD 28+000), District Sialkot Prepared by: Abdul Hameed, TA Resettlement Specialist for Project Implementation Unit, Communications and Works Department, Government of Punjab, Lahore. This due diligence report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of -

Parcel Post Compendium Online Pakistan Post PKA PK
Parcel Post Compendium Online PK - Pakistan Pakistan Post PKA Basic Services CARDIT Carrier documents international Yes transport – origin post 1 Maximum weight limit admitted RESDIT Response to a CARDIT – destination Yes 1.1 Surface parcels (kg) 50 post 1.2 Air (or priority) parcels (kg) 50 6 Home delivery 2 Maximum size admitted 6.1 Initial delivery attempt at physical Yes delivery of parcels to addressee 2.1 Surface parcels 6.2 If initial delivery attempt unsuccessful, Yes 2.1.1 2m x 2m x 2m No card left for addressee (or 3m length & greatest circumference) 6.3 Addressee has option of paying taxes or Yes 2.1.2 1.5m x 1.5m x 1.5m Yes duties and taking physical delivery of the (or 3m length & greatest circumference) item 2.1.3 1.05m x 1.05m x 1.05m No 6.4 There are governmental or legally (or 2m length & greatest circumference) binding restrictions mean that there are certain limitations in implementing home 2.2 Air parcels delivery. 2.2.1 2m x 2m x 2m No 6.5 Nature of this governmental or legally (or 3m length & greatest circumference) binding restriction. 2.2.2 1.5m x 1.5m x 1.5m Yes (or 3m length & greatest circumference) 2.2.3 1.05m x 1.05m x 1.05m No 7 Signature of acceptance (or 2m length & greatest circumference) 7.1 When a parcel is delivered or handed over Supplementary services 7.1.1 a signature of acceptance is obtained Yes 3 Cumbersome parcels admitted No 7.1.2 captured data from an identity card are Yes registered 7.1.3 another form of evidence of receipt is No Parcels service features obtained 5 Electronic exchange of information -
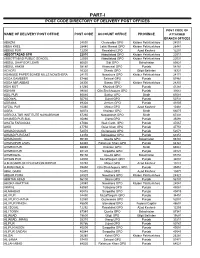
Part-I: Post Code Directory of Delivery Post Offices
PART-I POST CODE DIRECTORY OF DELIVERY POST OFFICES POST CODE OF NAME OF DELIVERY POST OFFICE POST CODE ACCOUNT OFFICE PROVINCE ATTACHED BRANCH OFFICES ABAZAI 24550 Charsadda GPO Khyber Pakhtunkhwa 24551 ABBA KHEL 28440 Lakki Marwat GPO Khyber Pakhtunkhwa 28441 ABBAS PUR 12200 Rawalakot GPO Azad Kashmir 12201 ABBOTTABAD GPO 22010 Abbottabad GPO Khyber Pakhtunkhwa 22011 ABBOTTABAD PUBLIC SCHOOL 22030 Abbottabad GPO Khyber Pakhtunkhwa 22031 ABDUL GHAFOOR LEHRI 80820 Sibi GPO Balochistan 80821 ABDUL HAKIM 58180 Khanewal GPO Punjab 58181 ACHORI 16320 Skardu GPO Gilgit Baltistan 16321 ADAMJEE PAPER BOARD MILLS NOWSHERA 24170 Nowshera GPO Khyber Pakhtunkhwa 24171 ADDA GAMBEER 57460 Sahiwal GPO Punjab 57461 ADDA MIR ABBAS 28300 Bannu GPO Khyber Pakhtunkhwa 28301 ADHI KOT 41260 Khushab GPO Punjab 41261 ADHIAN 39060 Qila Sheikhupura GPO Punjab 39061 ADIL PUR 65080 Sukkur GPO Sindh 65081 ADOWAL 50730 Gujrat GPO Punjab 50731 ADRANA 49304 Jhelum GPO Punjab 49305 AFZAL PUR 10360 Mirpur GPO Azad Kashmir 10361 AGRA 66074 Khairpur GPO Sindh 66075 AGRICULTUR INSTITUTE NAWABSHAH 67230 Nawabshah GPO Sindh 67231 AHAMED PUR SIAL 35090 Jhang GPO Punjab 35091 AHATA FAROOQIA 47066 Wah Cantt. GPO Punjab 47067 AHDI 47750 Gujar Khan GPO Punjab 47751 AHMAD NAGAR 52070 Gujranwala GPO Punjab 52071 AHMAD PUR EAST 63350 Bahawalpur GPO Punjab 63351 AHMADOON 96100 Quetta GPO Balochistan 96101 AHMADPUR LAMA 64380 Rahimyar Khan GPO Punjab 64381 AHMED PUR 66040 Khairpur GPO Sindh 66041 AHMED PUR 40120 Sargodha GPO Punjab 40121 AHMEDWAL 95150 Quetta GPO Balochistan 95151 -

List of Branches Authorized for Overnight Clearing (Annexure - II) Branch Sr
List of Branches Authorized for Overnight Clearing (Annexure - II) Branch Sr. # Branch Name City Name Branch Address Code Show Room No. 1, Business & Finance Centre, Plot No. 7/3, Sheet No. S.R. 1, Serai 1 0001 Karachi Main Branch Karachi Quarters, I.I. Chundrigar Road, Karachi 2 0002 Jodia Bazar Karachi Karachi Jodia Bazar, Waqar Centre, Rambharti Street, Karachi 3 0003 Zaibunnisa Street Karachi Karachi Zaibunnisa Street, Near Singer Show Room, Karachi 4 0004 Saddar Karachi Karachi Near English Boot House, Main Zaib un Nisa Street, Saddar, Karachi 5 0005 S.I.T.E. Karachi Karachi Shop No. 48-50, SITE Area, Karachi 6 0006 Timber Market Karachi Karachi Timber Market, Siddique Wahab Road, Old Haji Camp, Karachi 7 0007 New Challi Karachi Karachi Rehmani Chamber, New Challi, Altaf Hussain Road, Karachi 8 0008 Plaza Quarters Karachi Karachi 1-Rehman Court, Greigh Street, Plaza Quarters, Karachi 9 0009 New Naham Road Karachi Karachi B.R. 641, New Naham Road, Karachi 10 0010 Pakistan Chowk Karachi Karachi Pakistan Chowk, Dr. Ziauddin Ahmed Road, Karachi 11 0011 Mithadar Karachi Karachi Sarafa Bazar, Mithadar, Karachi Shop No. G-3, Ground Floor, Plot No. RB-3/1-CIII-A-18, Shiveram Bhatia Building, 12 0013 Burns Road Karachi Karachi Opposite Fresco Chowk, Rambagh Quarters, Karachi 13 0014 Tariq Road Karachi Karachi 124-P, Block-2, P.E.C.H.S. Tariq Road, Karachi 14 0015 North Napier Road Karachi Karachi 34-C, Kassam Chamber's, North Napier Road, Karachi 15 0016 Eid Gah Karachi Karachi Eid Gah, Opp. Khaliq Dina Hall, M.A. -

FLOOD RISK ASSESSMENT REPORT a Hi-Tech Knowledge Management Tool for Disaster Risk Assessment at UNION COUNCIL Level
2015 FLOOD RISK ASSESSMENT REPORT A Hi-Tech Knowledge Management Tool for Disaster Risk Assessment at UNION COUNCIL Level A PROPOSAL IN VIEW OF LESSONS LEARNED ISBN (P) 978-969-638-093-1 ISBN (D) 978-969-638-094-8 205-C 2nd Floor, Evacuee Trust Complex, F-5/1, Islamabad 195-1st Floor, Deans Trade Center, Peshawar Cantt; Peshawar Landline: +92.51.282.0449, +92.91.525.3347 E-mail: [email protected], Website: www.alhasan.com ALHASAN SYSTEMS PRIVATE LIMITED A Hi-Tech Knowledge Management, Business Psychology Modeling, and Publishing Company 205-C, 2nd Floor, Evacuee Trust Complex, Sector F-5/1, Islamabad, Pakistan 44000 195-1st Floor, Dean Trade Center, Peshawar Can ; Peshawar, Pakistan 25000 Landline: +92.51.282.0449, +92.91.525.3347 Fax: +92.51.835.9287 Email: [email protected] Website: www.alhasan.com Facebook: www.facebook.com/alhasan.com Twi er: @alhasansystems w3w address: *Alhasan COPYRIGHT © 2015 BY ALHASAN SYSTEMS All rights reserved. No part of this publica on may be reproduced, stored in a retrieval system, or transmi ed, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior wri en permission of ALHASAN SYSTEMS. 58 p.; 8.5x11.5 = A3 Size Map ISBN (P) 978-969-638-093-1 ISBN (D) 978-969-638-094-8 CATALOGING REFERENCE: Disaster Risk Reduc on – Disaster Risk Management – Disaster Risk Assessment Hyogo Framework for Ac on 2005-2015 Building the Resilience of Na ons and Communi es to Disasters IDENTIFY, ACCESS, AND MONITOR DISASTER RISKS AND ENHANCE EARLY WARNING x Risk assessments -

Organic Matter Status of Gujar Khan Tehsil
Pakistan Journal of Biological Sciences 3 (12): 2033-2034, 2000 © Copyright by the Capricorn Publications, 2000 Organic Matter Status of Gujar Khan Tehsil Sohail Jamil Qureshi1, Rizwana A. Qureshi1 2Muhammad Yousuf and M. Rizwan3 1Department of Biological Sciences, Quaid-I-Azam University, Islamabad, Pakistan 2Department of Soil Science, University of Arid Agriculture, Rawalpindi, Pakistan 3Soil Fertility Survey and Soil Testing Institute, Rawalpindi, Pakistan Abstract: A study was conducted to investigate the organic matter status of Tehsil Gujar Khan of district Rawalpindi. Forty eight composite soil samples were collected from different sites of Tehsil. These samples were analyzed for organic matter. Organic matter was deficient or poor <0.86% in all the soil samples analyzed. The maximum organic matter of 0.8% were recorded at Bardiana site and minimum organic matter of 0.25% were observed at Gulliana site. The average maximum organic matter of 0.6% were observed at Bardiana and Daultala sites in the Tehsil. The low organic matter at most of the sites may be due to eroded nature of soils in this area. Fertilizer recommendations were advised to farmers according to soil condition and organic matter status of the soil. Key words: Organic matter, Tehsil Gujar Khan, fertility status, recommendation Introduction supplies of different nutrients and changes affecting nutrient Most of the soils in Pakistan have been exhausted due to availability. In almost all the countries soil testing survey is continuous crop production and meager replenishment, available for making fertilizer recommendations (Chaudhary, 1980). It is a rapid and less expensive method for evaluation particularly in rainfed areas. -

Village List of Gujranwala , Pakistan
Census 51·No. 30B (I) M.lnt.6-18 300 CENSUS OF PAKISTAN, 1951 VILLAGE LIST I PUNJAB Lahore Divisiona .,.(...t..G.ElCY- OF THE PROVINCIAL TEN DENT CENSUS, JUr.8 1952 ,NO BAHAY'(ALPUR Prleo Ps. 6·8-0 FOREWORD This Village List has been pr,epared from the material collected in con" nection with the Census of Pakistan, 1951. The object of the List is to present useful information about our villages. It was considered that in a predominantly rural country like Pakistan, reliable village statistics should be avaflable and it is hoped that the Village List will form the basis for the continued collection of such statistics. A summary table of the totals for each tehsil showing its area to the nearest square mile. and Its population and the number of houses to the nearest hundred is given on page I together with the page number on which each tehsil begins. The general village table, which has been compiled district-wise and arranged tehsil-wise, appears on page 3 et seq. Within each tehsil the Revenue Kanungo holqos are shown according to their order in the census records. The Village in which the Revenue Kanungo usually resides is printed in bold type at the beginning of each Kanungo holqa and the remaining Villages comprising the ha/qas, are shown thereunder in the order of their revenue hadbast numbers, which are given in column o. Rokhs (tree plantations) and other similar areas even where they are allotted separate revenue hadbast numbers have not been shown as they were not reported in the Charge and Household summaries. -

Appendix - II Pakistani Banks and Their Branches (December 31, 2008)
Appendix - II Pakistani Banks and their Branches (December 31, 2008) Allied Bank Ltd. Bhalwal (2) Chishtian (2) -Grain Market -Grain Market (743) -Noor Hayat Colony -Mohar Sharif Road Abbaspur 251 RB Bandla Bheli Bhattar (A.K.) Chitral Chungpur (A.K.) Abbottabad (4) Burewala (2) Dadu -Bara Towers, Jinnahabad -Grain Market -Pineview Road -Housing Scheme Dadyal (A.K) (2) -Supply Bazar -College Road -The Mall Chak Jhumra -Samahni Ratta Cross Chak Naurang Adda Johal Chak No. 111 P Daharki Adda Nandipur Rasoolpur Chak No. 122/JB Nurpur Danna (A.K.) Bhal Chak No. 142/P Bangla Danyor Adda Pansra Manthar Darband Adda Sarai Mochiwal Chak No. 220 RB Dargai Adda Thikriwala Chak No. 272 HR Fortabbas Darhal Gaggan Ahmed Pur East Chak No. 280/JB (Dawakhri) Daroo Jabagai Kombar Akalgarh (A.K) Chak No. 34/TDA Daska Arifwala Chak No. 354 Daurandi (A.K.) Attock (Campbellpur) Chak No. 44/N.B. Deenpur Bagh (A.K) Chak No. 509 GB Deh Uddhi Bahawalnagar Chak No. 76 RB Dinga Chak No. 80 SB Bahawalpur (5) Chak No. 88/10 R Dera Ghazi Khan (2) Chak No. 89/6-R -Com. Area Sattelite Town -Azmat Road -Dubai Chowk -Model Town -Farid Gate Chakwal (2) -Ghalla Mandi -Mohra Chinna Dera Ismail Khan (3) -Settelite Town -Talagang Road -Circular Road -Commissionery Bazar Bakhar Jamali Mori Talu Chaman -Faqirani Gate (Muryali) Balagarhi Chaprar Balakot Charsadda Dhamke (Faisalabad) Baldher Chaskswari (A.K) Dhamke (Sheikhupura) Bucheke Chattar (A.K) Dhangar Bala (A.K) Chhatro (A.K.) Dheed Wal Bannu (2) Dina -Chai Bazar (Ghalla Mandi) Chichawatni (2) Dipalpur -Preedy Gate -College Road Dir Barja Jandala (A.K) -Railway Road Dunyapur Batkhela Ellahabad Behari Agla Mohra (A.K.) Chilas Eminabad More Bewal Bhagowal Faisalabad (20) Bhakkar Chiniot (2) -Akbarabad Bhaleki (Phularwan Chowk) -Muslim Bazar (Main) -Sargodha Road -Chibban Road 415 ABL -Factory Area -Zia Plaza Gt Road Islamabad (23) -Ghulam Muhammad Abad Colony Gujrat (3) -I-9 Industrial Area -Gole Cloth Market -Grand Trunk Road -Aabpara -Gole Kiryana Bazar -Rehman Saheed Road -Blue Area ABL -Gulburg Colony -Shah Daula Road. -

Rawalpindi 1 Rawalpindi Leprosy Hospital, Zafar-Ul-Haq Road P.O Box No
Valid X-ray License Holder Sr. Facility Rawalpindi 1 Rawalpindi Leprosy Hospital, Zafar-ul-Haq Road P.O Box No. 135, Rawalpindi 2 Al-Shifa Eye Hospital, Jehlum Road, Rawalpindi 3 Health Ways Medical Centre, 8-111, Murree Road Opp. Ministry of Defence Secretrait, Saddar, Rawalpindi 4 Habib Hospital, Saidpur Road, Banni, Rawalpindi 5 Armed Forces Institute of Cadialogy(AFIC), The Mall Road, Rawalpindi 6 Christian Hospital, Faisal Shahid Road, Taxila, Rawalpindi 7 Islamic International Medical Complex Trust, Railway Hospital, Westridge, Rawalpindi 8 Abrar Surgery (Pvt.) Ltd, 219-B(1), Peshawar Road, Rawalpindi 9 Abrar Diagnostic Centre, 312-E, Chairing Cross Peshawar Road, Rawalpindi 10 WAPDA Hospital, Marrier Hassan, Rawalpindi 11 Combined Military Hospital, Murree, Rawalpindi 12 Attock Hospital(Pvt.) Ltd., P. O. Refinary Morgah, Rawalpindi 13 Kahuta Research Laboratories (KRL) Hospital, P. O. Sumbulgah, Tehsil Kahuta, Rawalpindi 14 KRL Medical Center, Dr. A. Q. Khan Road, P. O. Box 502, Rawalpindi 15 Urgent Medical Centre, Medical Tower, 101-A 6th Road, Satellite Town, Rawalpindi 16 Adil Diagnostics, B-1315, Saidpur Road, Rawalpindi 17 Valley Clinic (Pvt.) Ltd., 213, Peshawar Road, Lane 4, Rawalpindi 18 Maryam Memorial Hospital, Peshawar Road, Rawalpindi 19 Dr. Aslam Uppal Hospital & Labs, 3-Quaid Avenue Near Aslam Uppal Square, Lalazar, Wah Cantt., Rawalpindi 20 C/o Dr. Amenah Dental Clinic, 167/3A, Adamjee Road, Rawalpindi, Rawalpindi 21 Margalla Hospital, Pirwadahi Road, Pirwadahi, Rawalpindi 22 Al-Noor Dental Clinic, Mushtaq Plaza Holy Family Chowk Saidpur Raod, Rawalpindi 23 Hearts International Hospital, 192-A, The Mall, Rawalpindi 24 Al-Mustafa Trust Medical Center, Street No. 14, Mini Market Chaklala Scheme-III, Rawalpindi 25 Aman Hospital, 519/8-A, Misrial Road, Rawalpindi 26 DHQ Hospital, Raja Bazar, Rawalpindi 27 HIT Hospital, Taxila Cantt., Taxila, Rawalpindi 28 Syed Mohd Hussain Govt. -

Find Address of Your Nearest Loan Center and Phone Number of Concerned Focal Person
Find address of your nearest loan center and phone number of concerned focal person Loan Center/ S.No. Province District PO Name City / Tehsil Focal Person Contact No. Union Council/ Location Address Branch Name Akhuwat Islamic College Chowk Oppsite Boys College 1 Azad Jammu and Kashmir Bagh Bagh Bagh Nadeem Ahmed 0314-5273451 Microfinance (AIM) Sudan Galli Road Baagh Akhuwat Islamic Muzaffarabad Road Near main bazar 2 Azad Jammu and Kashmir Bagh Dhir Kot Dhir Kot Nadeem Ahmed 0314-5273451 Microfinance (AIM) dhir kot Akhuwat Islamic Mang bajri arja near chambar hotel 3 Azad Jammu and Kashmir Bagh Harighel Harighel Nadeem Ahmed 0314-5273451 Microfinance (AIM) Harighel Akhuwat Islamic 4 Azad Jammu and Kashmir Bhimber Bhimber Bhimber Arshad Mehmood 0346-4663605 Kotli Mor Near Muslim & School Microfinance (AIM) Akhuwat Islamic 5 Azad Jammu and Kashmir Bhimber Barnala Barnala Arshad Mehmood 0346-4663605 Main Road Bimber & Barnala Road Microfinance (AIM) Akhuwat Islamic Main choki Bazar near Sir Syed girls 6 Azad Jammu and Kashmir Bhimber Samahni Samahni Arshad Mehmood 0346-4663605 Microfinance (AIM) College choki Samahni Helping Hand for Adnan Anwar HHRD Distrcict Office Relief and Hattian,Near Smart Electronics,Choke 7 Azad Jammu and Kashmir Hattian Hattian UC Hattian Adnan Anwer 0341-9488995 Development Bazar, PO, Tehsil and District (HHRD) Hattianbala. Helping Hand for Adnan Anwar HHRD Distrcict Office Relief and Hattian,Near Smart Electronics,Choke 8 Azad Jammu and Kashmir Hattian Hattian UC Langla Adnan Anwer 0341-9488995 Development Bazar, PO, Tehsil and District (HHRD) Hattianbala. Helping Hand for Relief and Zahid Hussain HHRD Lamnian office 9 Azad Jammu and Kashmir Hattian Hattian UC Lamnian Zahid Hussain 0345-9071063 Development Main Lamnian Bazar Hattian Bala. -

1 Annexure - D Names of Village / Neighbourhood Councils Alongwith Seats Detail of Khyber Pakhtunkhwa
1 Annexure - D Names of Village / Neighbourhood Councils alongwith seats detail of Khyber Pakhtunkhwa No. of General Seats in No. of Seats in VC/NC (Categories) Names of S. Names of Tehsil Councils No falling in each Neighbourhood Village N/Hood Total Col Peasants/Work S. No. Village Councils (VC) S. No. Women Youth Minority . district Council Councils (NC) Councils Councils 7+8 ers 1 2 3 4 5 6 7 8 9 10 11 12 13 Abbottabad District Council 1 1 Dalola-I 1 Malik Pura Urban-I 7 7 14 4 2 2 2 2 Dalola-II 2 Malik Pura Urban-II 7 7 14 4 2 2 2 3 Dabban-I 3 Malik Pura Urban-III 5 8 13 4 2 2 2 4 Dabban-II 4 Central Urban-I 7 7 14 4 2 2 2 5 Boi-I 5 Central Urban-II 7 7 14 4 2 2 2 6 Boi-II 6 Central Urban-III 7 7 14 4 2 2 2 7 Sambli Dheri 7 Khola Kehal 7 7 14 4 2 2 2 8 Bandi Pahar 8 Upper Kehal 5 7 12 4 2 2 2 9 Upper Kukmang 9 Kehal 5 8 13 4 2 2 2 10 Central Kukmang 10 Nawa Sher Urban 5 10 15 4 2 2 2 11 Kukmang 11 Nawansher Dhodial 6 10 16 4 2 2 2 12 Pattan Khurd 5 5 2 1 1 1 13 Nambal-I 5 5 2 1 1 1 14 Nambal-II 6 6 2 1 1 1 Abbottabad 15 Majuhan-I 7 7 2 1 1 1 16 Majuhan-II 6 6 2 1 1 1 17 Pattan Kalan-I 5 5 2 1 1 1 18 Pattan Kalan-II 6 6 2 1 1 1 19 Pattan Kalan-III 6 6 2 1 1 1 20 Sialkot 6 6 2 1 1 1 21 Bandi Chamiali 6 6 2 1 1 1 22 Bakot-I 7 7 2 1 1 1 23 Bakot-II 6 6 2 1 1 1 24 Bakot-III 6 6 2 1 1 1 25 Moolia-I 6 6 2 1 1 1 26 Moolia-II 6 6 2 1 1 1 1 Abbottabad No. -

Audit Report on the Accounts of City District Government Rawalpindi Audit
AUDIT REPORT ON THE ACCOUNTS OF CITY DISTRICT GOVERNMENT RAWALPINDI AUDIT YEAR 2016-17 AUDITOR GENERAL OF PAKISTAN TABLE OF CONTENTS ABBREVIATIONS & ACRONYMS............................................................................................. I PREFACE...................................................................................................................................... III EXECUTIVE SUMMARY .......................................................................................................... IV SUMMARY TABLE & CHARTS ............................................................................................ VIII TABLE 1: AUDIT WORK STATISTICS ................................................................................... VIII TABLE 2: AUDIT OBSERVATIONS ........................................................................................ VIII TABLE3: OUTCOME STATISTICS ............................................................................................ IX TABLE4: IRREGULARITIES POINTED OUT ............................................................................. X TABLE 5 COST BENEFIT ............................................................................................................. X CHAPTER 1 .................................................................................................................................... 1 1.1 CITY DISTRICT GOVERNMENT RAWALPINDI ........................................................ 1 1.1.1 INTRODUCTION OF DEPARTMENTS ........................................................................