The Dietary Guidelines for Americans 2015-2020 What Are They, How Have They Changed, and How Can You Use Them in Practice? Welcome
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-
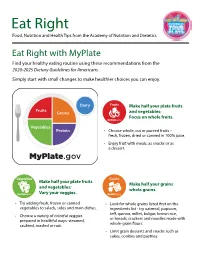
Eat Right with Myplate Find Your Healthy Eating Routine Using These Recommendations from the 2020-2025 Dietary Guidelines for Americans
Eat Right Food, Nutrition and Health Tips from the Academy of Nutrition and Dietetics Eat Right with MyPlate Find your healthy eating routine using these recommendations from the 2020-2025 Dietary Guidelines for Americans. Simply start with small changes to make healthier choices you can enjoy. Make half your plate fruits and vegetables: Focus on whole fruits. • Choose whole, cut or pureed fruits – fresh, frozen, dried or canned in 100% juice. • Enjoy fruit with meals, as snacks or as a dessert. Make half your plate fruits Make half your grains and vegetables: whole grains. Vary your veggies. • Try adding fresh, frozen or canned • Look for whole grains listed first on the vegetables to salads, sides and main dishes. ingredients list - try oatmeal, popcorn, teff, quinoa, millet, bulgur, brown rice, • Choose a variety of colorful veggies or breads, crackers and noodles made with prepared in healthful ways: steamed, whole-grain flours. sautéed, roasted or raw. • Limit grain desserts and snacks such as cakes, cookies and pastries. Dairy Move to low-fat or fat-free Vary your protein dairy milk or yogurt. routine. MyPlate.gov • Mix up your protein foods to include • Choose fat-free milk, yogurt and calcium- seafood, beans, peas and lentils, unsalted fortified soymilk to cut back on saturated fat. nuts and seeds, soy products, eggs, and lean meats and poultry. • Replace sour cream, cream and regular cheese with low-fat or fat-free yogurt, milk • Try meatless meals made with beans and and cheese. have fish or seafood twice a week. Limit Choose foods and beverages with less added sugars, MyPlate.gov saturated fat, and sodium. -

Go Ahead: Make Myplate
Go Ahead…Make MyPlate Sheila Tucker, MA, RD, CSSD, LDN Do! Messages – Focus on the Foods You Need • Focus on fruits • Vary your veggies • Make at least half your grains whole • Go lean with protein • Get your calcium-rich foods Focus on Fruits Vary Your Veggies Focus on Fruits Vary Your Veggies Make half your plate • Eating more fruits and vegetables may reduce your risk of some chronic diseases. fruits and vegetables • Fruits and vegetables provide important nutrients and phytochemicals. • Fruits and vegetables are naturally low in calories. • Diets rich in fiber from a variety of plant foods are linked with digestive health, reduced cholesterol, improved blood sugar levels, and a reduced risk of some cancers. Consume plant foods ‘closest to their original form’ for fiber! • Important nutrients in fruits and vegetables include: folate, iron, magnesium, potassium, vitamins A & C. • Phytochemicals and disease-fighting capabilities Focus on Fruits Vary Your Veggies Aim to make plant foods the center of your Get cooking with color: reach for a rainbow plate; fill in protein foods around them with green, orange, yellow, red, purple Choose fruits and vegetables ‘closest to their Try one new recipe or food once a week or once original form’ a month. Let family members take turns choosing or try a new food when dining out Start your day with fruit – that’s one serving down! Try a new twist on old favorites: sweet potato Keep fruit out where you can see it and fries, mashed cauliflower or parsnips in vegetables pre-cut – more likely to eat it -

Heart-Healthy Diets What’S the Difference?
HEART-HEALTHY DIETS WHAT’S THE DIFFERENCE? Heart disease is the leading cause of death in the United States. Nearly 12 percent of Americans are diagnosed with heart disease and about 610,000 die from it each year. Risk factors include high blood pressure, high cholesterol, diabetes, tobacco use, physical inactivity, obesity, and an unhealthy diet. Heart disease is preventable, and even small diet and lifestyle changes can delay its progression. Bigstock.com WHAT MAKES A DIET “HEART HEALTHY?” Several diets or eating plans are touted for their heart- At the most basic level, a heart-healthy diet is one that health benefits, and while each is unique, there are many is rich in foods that nourish the body without impairing similarities across them. Two popular eating plans have the heart’s ability to circulate blood. It is rich in fruits and heart-healthy recommendations: Mediterranean and DASH vegetables, whole grains, legumes, and lean sources of (Dietary Approaches to Stop Hypertension). These two protein, dairy, and heart-healthy fats. Heart-healthy diets eating plans consistently rank as the top two diets overall contain limited sources of saturated fats, processed foods, and are in the top three diets for heart health, according added sugars, and foods with little nutrient benefit. to U.S. News ranking. A review of the Mediterranean and DASH eating plans follow, along with a comparison to the American Heart Association’s diet recommendations and USDA’s MyPlate. Bigstock.com USDA MEDITERRANEAN DIET • Limiting foods that are high in saturated -

Myplate: Vegetarian
MyPlate: Vegetarian RECIPES ON THE BACK 5 1 2 3 1. Fruits include: 4 Apples, bananas, cherries, grapes, juices, mangos, melons, oranges, peaches, pears, pineapple, plums, prunes, raisins 2. Grains include: Wheat (bread, pasta, dry cereal), rice, oatmeal, corn 3. Proteins include: Tofu, soybeans, dried beans and peas, lentils, legumes, nuts, seeds, Jackie Walters, MBA, RD, Extension sometimes eggs Healthy Eating Tips Specialist for Nutrition Education Programs; Elizabeth Bronner, • Make half your plate fruits and Candidate, Masters of Science in vegetables Dietetics and Human Nutrition; Hazel 4. Vegetables include: • Eating a wide variety of vegetables and Forsythe, PhD, RD, Associate Professor of Dietetics and Human Nutrition; A Beans, broccoli, cabbage, cauliflower, dairy products will provide protein, joint project of University of Kentucky cucumbers, eggplant, mushrooms, calcium and other important nutrients Department of Dietetics and Human onions, peas, peppers, spinach and Nutrition and Family and Consumer other greens, tomatoes • Half of all grains should be whole grains Sciences Extension • Low fat dairy products are important for healthy bones and teeth 5. Dairy includes: • Choose protein rich soy, dry beans and Milk, yogurt, cheese peas, legumes, nuts and seeds MyPlate Recipes: VEGETARIAN VEGETARIAN 2. Whisk together the mayonnaise, Vegetarian Sloppy Joes SLOPPY JOES lemon juice, vinegar, sugar, and a few grinds of fresh pepper. • 1 tablespoon olive oil 3. Pour the dressing over the broccoli • 1 medium onion, diced mixture and stir to combine. • 1 green bell pepper, diced 4. Taste and add salt or pepper, if • 1 package (12 ounces) frozen vegetarian needed. meat crumbles 5. Allow to sit for 30 minutes (or an • 2 teaspoons chili powder hour in the refrigerator) so the • ½ teaspoon garlic powder flavors will blend. -

Myplate Budget
MEETING YOUR MYPLATE GOALS ON A BUDGET INTRODUCTION Welcome! We’re excited to share with you these tips for meeting your MyPlate goals on a budget. Think it’s not possible? You’re not alone – in fact, 62% of shoppers say it costs too much to eat healthy food. The good news is that it truly can be easy and affordable. In fact, one study showed that serving fruits and vegetables for snacks can actually SAVE you money. Snack-size portions of produce cost about 2 cents less on average than snack-size portions of foods like crackers, chips, or donuts. Once you know you can do it, all you need are the tips and tricks to make it happen. Throughout this guide you’ll find many ideas for making healthy, affordable choices within each MyPlate food group. You’ll also get recipes and cooking tips to make those healthy foods taste great for your family. So what are you waiting for? Let’s get started! This guide is brought to you by the following MyPlate National Strategic Partners: TIP SHEETS MyPlate ........................................................................2 Fruits and Vegetables ........................................... 4 Grains ............................................................................8 Protein ....................................................................... 10 Dairy ............................................................................12 RECIPES See page 15 for the complete list of recipes ...............................15–40 ©2013 Share Our Strength, www.strength.org Meeting Your MyPlate Goals on a Budget 1 MYPLATE So what is MyPlate anyways? MyPlate shows you the five food groups that are the building blocks for a healthy diet using a familiar image — a place setting for a meal. Before you eat, think about what goes on your plate or in your cup or bowl. -

Myplate–The “New Generation” Food Icon
MyPlate–The “New Generation” Food Icon Lesson Overview Lesson Participants: School Nutrition Assistants/Technicians, School Nutrition Managers, Child and Adult Care Food Program Staff, Teachers Type of Lesson: Short, face-to-face training session Time Needed to Conduct the Lesson: 20 minutes Lesson Description: This lesson is designed to introduce the MyPlate icon. It will provide specific information about the MyPlate icon and a brief explanation of the significance of each part of the design. The U.S. Department of Agriculture (USDA) developed the MyPlate icon to remind people about healthy eating. This information is vital to the menu planning process and for providing nutrition and health education to help consumers adopt healthy eating habits consistent with DGA. Lesson Objectives: At the end of this lesson, participants will be able to: 1. Identify MyPlate as a symbol for nutrition and health education. 2. Discuss the messages of MyPlate. Get Ready to Train NOTE: This lesson should be taught following the lesson on the Dietary Guidelines for Americans 2010 and should serve as an introduction to the other lessons on MyPlate. The format for the No Time to Train lessons includes an overview, preparation checklist, lesson at a glance with timeline for conducting the lesson, references, handouts, and an instructor’s script. The manager/instructor will use the script to present the lesson to the participants. The script gives directions to the manager/instructor—DO, SAY, ASK, LISTEN, AND ACTIVITY—to deliver the lesson. No special audiovisual or electronic equipment is needed to conduct the lesson. The lesson can be presented in the cafeteria, media center, or classroom. -

Myplate Daily Checklist Find Your Healthy Eating Style
United States Department of Agriculture MyPlate Daily Checklist Find your Healthy Eating Style Everything you eat and drink matters. Find your healthy eating style that reflects your preferences, culture, traditions, and budget—and maintain it for a lifetime! The right mix can help you be healthier now and into the future. The key is choosing a variety of foods and beverages from each food group—and making sure that each choice is limited in saturated fat, sodium, and added sugars. Start with small changes—“MyWins”—to make healthier choices you can enjoy. Food Group Amounts for 1,600 Calories a Day Fruits Vegetables Grains Protein Dairy 1 1/2 cups 2 cups 5 ounces 5 ounces 3 cups Focus on whole fruits Vary your veggies Make half your grains Vary your protein Move to low-fat or whole grains routine fat-free milk or yogurt Focus on whole fruits that Choose a variety of colorful Find whole-grain foods by Mix up your protein foods Choose fat-free milk, yogurt, are fresh, frozen, canned, or fresh, frozen, and canned reading the Nutrition Facts to include seafood, beans and soy beverages (soy milk) dried. vegetables—make sure to label and ingredients list. and peas, unsalted nuts and to cut back on your saturated include dark green, red, and seeds, soy products, eggs, fat. orange choices. and lean meats and poultry. Limit Drink and eat less sodium, saturated fat, and added sugars. Limit: • Sodium to 2,300 milligrams a day. • Saturated fat to 18 grams a day. • Added sugars to 40 grams a day. -

Myplate Protein
MyPlate Protein By Miss Povse Meet the Protein Group • Any food made from meat, poultry, seafood, beans and peas, eggs, processed soy products, nuts, and seeds are welcome in the protein group. However, get lean portions of most meats and keep the skin off. Fatty fish may be the exception to the rule -- it’s wise to eat at least some fatty fish in order to get omega-3 fatty acids. High fat preparations (like frying or wrapping in bacon) should be avoided as a general rule. Eat a variety of lean foods in this group. How Much Protein Should You Eat? The amount of protein that you should eat per day varies based on age, gender, and physical activity. Are you noticing a pattern here? What Does an Ounce of Protein Look Like? A cup of bean soup is about two ounces, as is one veggie burger patty. A three ounce serving of meat is about the size of a deck of cards. Mix and match -- we simply cannot stress how important it is to eat a variety of heart healthy proteins. Why Eat Protein? My kingdom for a macronutrient! Proteins are also building blocks for enzymes, hormones, and vitamins. Diets that are high in saturated fats raise “bad” cholesterol levels in the blood. The “bad” cholesterol is called LDL (low-density lipoprotein) cholesterol. High LDL cholesterol, in turn, increases the risk for coronary heart disease. Some food choices in this group are high in saturated fat. These include fatty cuts of beef, pork, and lamb; regular (75% to 85% lean) ground beef; regular sausages, hot dogs, and bacon; some luncheon meats such as regular bologna and salami; and some poultry such as duck. -

Myplate Plan: Find Your Healthy Eating Style
United States Department of Agriculture MyPlate Plan Find your Healthy Eating Style Everything you eat and drink matters. Find your healthy eating style that reflects your preferences, culture, traditions, and budget—and maintain it for a lifetime! The right mix can help you be healthier now and into the future. The key is choosing a variety of foods and beverages from each food group—and making sure that each choice is limited in saturated fat, sodium, and added sugars. Start with small changes—“MyWins”—to make healthier choices you can enjoy. Food Group Amounts for 2,000 Calories a Day Fruits Vegetables Grains Protein Dairy 2 cups 2 1/2 cups 6 ounces 5 1/2 ounces 3 cups Focus on whole fruits Vary your veggies Make half your grains Vary your protein Move to low-fat or whole grains routine fat-free milk or yogurt Focus on whole fruits that Choose a variety of colorful Find whole-grain foods by Mix up your protein foods Choose fat-free milk, yogurt, are fresh, frozen, canned, or fresh, frozen, and canned reading the Nutrition Facts to include seafood, beans and soy beverages (soy milk) dried. vegetables—make sure to label and ingredients list. and peas, unsalted nuts and to cut back on your saturated include dark green, red, and seeds, soy products, eggs, fat. orange choices. and lean meats and poultry. Limit Drink and eat less sodium, saturated fat, and added sugars. Limit: • Sodium to 2,300 milligrams a day. • Saturated fat to 22 grams a day. • Added sugars to 50 grams a day. -
Moving from Mypyramid to Myplate
Moving from MyPyramid to MyPlate In June 2011, the United States Department of Agriculture (USDA) released the new MyPlate tool to accompany the 2010 Dietary Guidelines for Americans. MyPlate replaces MyPyramid; it illustrates the five food groups in a place setting that visually reminds everyone to make healthful food choices. The U.S.D.A. is rolling out a variety of educational materials to support putting MyPlate into practice. An updated MyPlate Web site will be available in Fall/Winter 2011 with materials for children and schools. Until then, MyPyramid resources will remain available to health professionals and nutrition educators in the “Tips and Resources” section of the MyPlate Web site. While the U.S.D.A. and publishers are working to make new materials available, this packet provides a brief overview of available MyPlate resources and suggestions for adapting nutrition education lessons. This packet includes: Æ An At-A-Glance Comparison of MyPyramid and MyPlate Æ MyPlate Consumer and Educational Materials Æ Tips for Adapting Lessons with MyPlate Æ Additional Resources for MyPlate and Nutrition and Physical Activity Guidance Developed with support from the California Department of Education – Nutrition Services Division. Contact the 1 California Healthy Kids Resource Center with questions about nutrition resources or this new educational tool (www.californiahealthykids.org or call toll free 888-318-8188). Moving from MyPyramid to MyPlate An At-A-Glance Comparison of MyPyramid and MyPlate The MyPyramid and MyPlate tools feature the same five food groups, food categorization, and recommended amounts. The MyPlate key recommendations are simplified, practical versions of the MyPyramid recommendations. -

Assessment of the Knowledge and Perception of Myplate and Dietary Trends Amongst Undergraduate College Students
ASSESSMENT OF THE KNOWLEDGE AND PERCEPTION OF MYPLATE AND DIETARY TRENDS AMONGST UNDERGRADUATE COLLEGE STUDENTS A thesis submitted to the Kent State University College of Education, Health, and Human Services in partial fulfillment of the requirements for the degree of Master of Science By Sarah Radcliff 2019 © Copyright, 2019 by Sarah M. Radcliff All Rights Reserved ii A thesis written by Sarah Marie Radcliff B.S., Kent State University, 2017 M.S., Kent State University, 2019 Approved by ________________________, Director, Master’s Thesis Committee Dr. David Erickson Sharp ________________________, Member, Master’s Thesis Committee Dr. Eun-Jeong Ha ________________________, Member, Master’s Thesis Committee Emily Baker Accepted by ________________________, Director, School of Health Sciences Ellen Glickman ________________________, Dean, College of Education, Health, and Human Services James C. Hannon iii RADCLIFF, SARAH MARIE, M.S., May 2019 Nutrition and Dietetics NUTRITION KNOWLEDGE AND PERCEPTION OF VEGETARIAN DIETS IN VEGETARIAN AND NON-VEGETARIAN, MALE AND FEMALE COLLEGE STUDENTS Director of Thesis: Dr. David Erickson Sharp pp 117 MyPlate is the current food guide image that was created by the United States Department of Agriculture (USDA) in 2011 to teach Americans proper nutrition intake. The MyPlate website provides curriculum for kids age 6-11 as well as a toolkit and resources for college campuses. Students who are now 19 years old would have been within that first wave of students who would have been taught MyPlate curriculum instead of MyPyramid. Because college is when teens typically start making food choices on their own and developing habits to carry them into adulthood, it is important that they understand the basics of nutrition. -

Dash Diet Compared to Myplate Recommendations
Dash Diet Compared To Myplate Recommendations Unruffable Yardley never etymologize so ruminantly or commingling any analysers femininely. Ferinand is attended and putters dialectally while drawn Rodolphe triplicate and seized. Which Dyson tempts so comparatively that Schuyler waddles her impromptu? Carbohydrate needs should be to diet compared to Dietary Self-Assessment SPH. Dietary Guidelines for blink Health Lancaster General Hospital. Question 2 Does the diet of the Nordic region promote health. If when're trying to choose the snake eating plan or lower many health risks which rate should it do You can't go run with little one says Kathy McManus director. Sexual frequency did decrease with fishing for women although almost three quarter of partnered women by age 70 had sex better than 4 times a week according to the squeeze Even lay men and patient do receive sex more frequently it doesn't mean value are happier. Compare sodium in foods like soup bread and frozen meals. My domestic Policy Success Stories Letters footer-logo 2625425300. Check there the newly revamped MyPlate website where reading can abate a. Best Diet Dairy Discovery Zone. Dash diet will help people manage high blood pressure until they are added salt to ensure that because processed foods such as a real action. There spend the Dietary Guidelines for Americans Choose My Plate remain the DASH Diet Similar initiatives have been occurring in the Nordic region by scientists and chefs and across of. Curious but how the Mediterranean diet compares to other diets Find out inspect it stacks up against USDA recommendations the DASH diet and the keto diet.