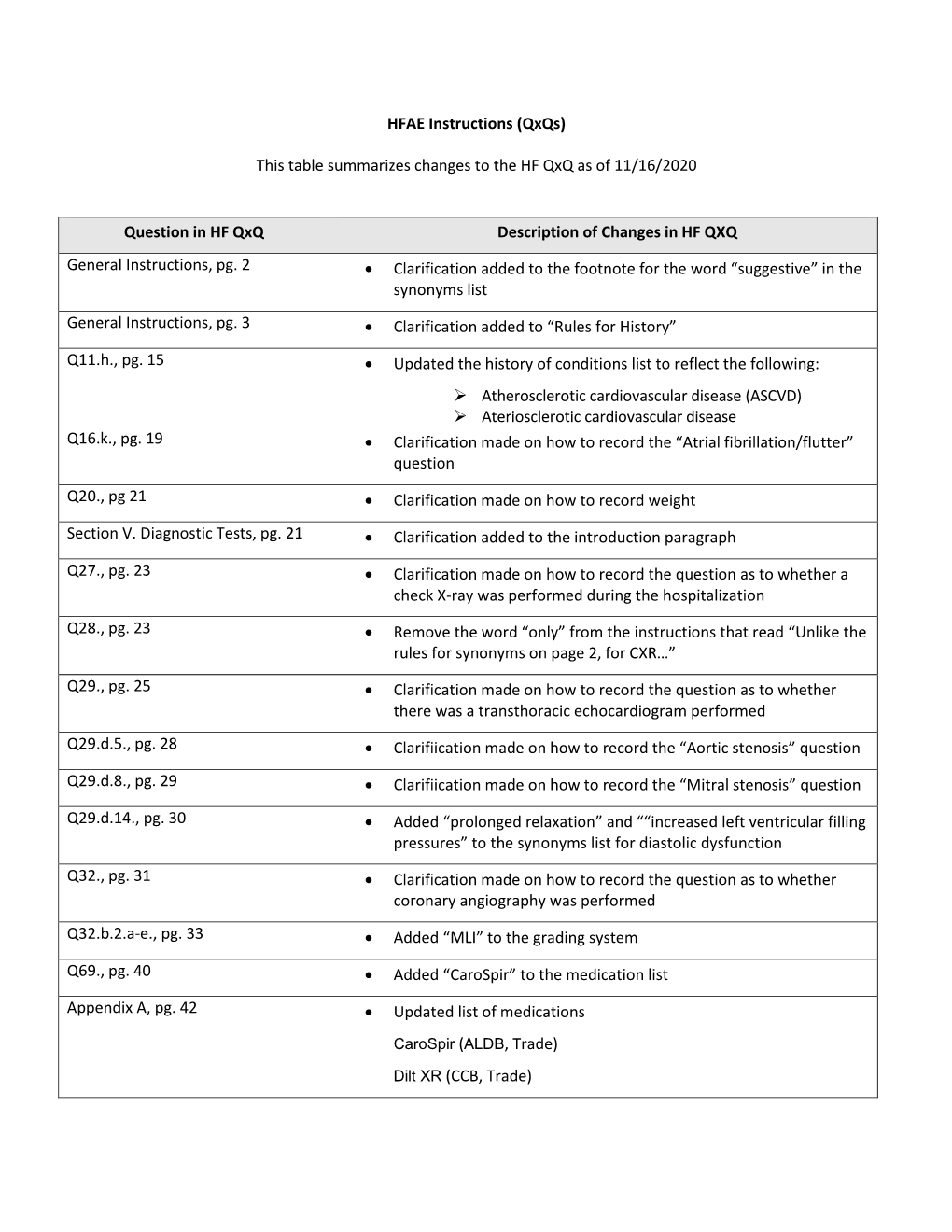
HFAE Instructions (Qxqs) This Table Summarizes Changes to the HF Qxq As of 11/16/2020 Question in HF Qxq Description of Changes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Rx Forum Volume 4 Issue 1
In This Issue Clevidipine for Hypertensive Urgency and Emergency From the Department of Pharmacy Tramadol: No Longer the Codeine Alternative January/February Issue 2016 Volume 4, Issue 1 FDA Medication Safety Alert: Risk of VTE with TestClevidipine for Hypertensive Urgency and Emergency osterone By: Gretchen D’Arcangelo, Pharm.D. Marcia J. Wyman, Pharm.D., BCPS Introduction: Hypertensive emergen- istration (FDA) for the reduction of BP Drug Information Pharmacist cies are deLined by potentially life- when oral therapy is not feasible Editor threatening elevations in blood pres- or desirable. 3 sure (BP) greater than 180/120 mmHg Mandy C. Leonard, Pharm.D., BCPS Pharmacokinetics: Following IV ad- System Director, Drug Use Policy and and are also paired with organ dysfunc- 1 ministration, clevidipine is rapidly me- Formulary Management tion. Hypertensive urgencies, on the Editor other hand, do not have the characteris- tabolized by blood and tissue esterases tic organ dysfunction present. These giving it a very quick onset of action Meghan K. Lehmann, Pharm.D., BCPS hypertensive crises are said to account and short half-life. 3 Its pharmacologic Drug Information Specialist effect starts within 2 to 4 minutes with Editor for up to 3% of emergency department admissions, with about three-fourths of a duration of action of up to 15 minutes. Marigel Constantiner, MSc, BCPS, CGP, CPh those admissions due to hypertensive EfLicacy and Safety: Patients undergo- Drug Information Specialist emergencies. 2 In patients with either Associate Editor ing cardiac surgery diagnosed with hy- hypertensive urgency or emergency, pertension in the past 6 months were immediate BP reduction should be at- Christopher Snyder, B.S., R.Ph. -

Nuclear Cardiology
1 XA9847621 Chapter 24 NUCLEAR CARDIOLOGY A. Cuardn Introduction. The assessment of cardiovascular performance with radionuclides dates back to 1927, when Blumgart and Weiss conducted the first clinical studies using a natural bismuth radioisotope 214Bi, in that time known as "Radium C". They injected a solution of this radionuclide into the vein of one arm and detected with a cloud chamber the appearance of its highly penetrating gamma rays in the contralateral arm. Their aim was to study the "velocity of the blood". In these pioneering studies, the mean normal arm-to-arm circulation time proved to be 18 sec., but it was found to be prolonged in patients with heart disease. Subsequently, they were able to calculate the pulmonary circulation time and the pulmonary blood volume by using a forerunner of the Geiger counter with platinum needle electrodes over the right atrium and the left elbow, and to study the effects on them of various heart and lung lesions, thyroid disorders, anaemia, polycythaemia, and drugs. Such classical studies, while appearing crude by today's technology, illustrate that minds and methods were fully prepared to exploit the eventual appearance of the artificial radioisotopes of elements of a more physiological character than bismuth, and laid the foundation for the established techniques of present day nuclear medicine. Although these studies on cardiovascular physiology were the first ever performed in humans with the aid of the radiotracer principle, the cardiologist had to wait for the accumulation of decades of research and development in the fields of radiochemistry, radiopharmacy and instrumentation before being able to capitalize this new approach for the non-invasive investigation of cardiac functions. -

Pharmaceutical Compositions of Clevidipine and Methods
(19) TZZ ¥ ZZ_T (11) EP 2 320 740 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61P 9/12 (2006.01) A61K 31/519 (2006.01) 26.03.2014 Bulletin 2014/13 A61K 9/10 (2006.01) (21) Application number: 09803550.4 (86) International application number: PCT/US2009/052127 (22) Date of filing: 29.07.2009 (87) International publication number: WO 2010/014727 (04.02.2010 Gazette 2010/05) (54) PHARMACEUTICAL COMPOSITIONS OF CLEVIDIPINE AND METHODS FOR PRODUCING LOW IMPURITY CONCENTRATIONS OF THE SAME PHARMAZEUTISCHE ZUSAMMENSETZUNGEN VON CLIVIDIPINE UND VERFAHREN ZUR HERSTELLUNG VON KONZENTRATIONEN DARAUS MIT GERINGEM VERUNREINIGUNGSGRAD COMPOSITIONS PHARMACEUTIQUES, COMPRENANT CLIVIDIPINE ET PROCÉDÉS POUR PRODUIRE DE FAIBLES CONCENTRATIONS D’IMPURETÉ DE CELLES-CI (84) Designated Contracting States: • FLOOD Keith AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Cary, NC 27518 (US) HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL • RAMAKRISHNA Kornepati PT RO SE SI SK SM TR Cary, NC 27513 (US) (30) Priority: 03.09.2008 US 93772 P (74) Representative: Wallace, Sheila Jane et al 01.08.2008 US 85597 P Marks & Clerk LLP 90 Long Acre (43) Date of publication of application: London 18.05.2011 Bulletin 2011/20 WC2E 9RA (GB) (60) Divisional application: (56) References cited: 14150954.7 WO-A1-00/31035 WO-A1-2006/118210 US-A1- 2003 119 883 US-A1- 2005 272 763 (73) Proprietors: US-A1- 2005 276 824 US-A1- 2006 047 125 • The Medicines Company US-A1- 2007 196 465 US-A1- 2008 019 978 Parsippany, NJ 07054 (US) • Hospira, Inc. -

(12) Patent Application Publication (10) Pub. No.: US 2014/0296.191 A1 PATEL Et Al
US 20140296.191A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2014/0296.191 A1 PATEL et al. (43) Pub. Date: Oct. 2, 2014 (54) COMPOSITIONS OF PHARMACEUTICAL (52) U.S. Cl. ACTIVES CONTAINING DETHYLENE CPC ............... A61K 47/10 (2013.01); A61 K9/0019 GLYCOL MONOETHYLETHER OR OTHER (2013.01); A61 K9/0048 (2013.01); A61 K ALKYL DERVATIVES 45/06 (2013.01) USPC ........... 514/167: 514/177; 514/178: 514/450; (71) Applicant: THEMIS MEDICARE LIMITED, 514/334: 514/226.5: 514/449; 514/338; Mumbai (IN) 514/256; 514/570; 514/179; 514/174: 514/533; (72) Inventors: Dinesh Shantilal PATEL, Mumbai (IN); 514/629; 514/619 Sachin Dinesh PATEL, Mumbai (IN); Shashikant Prabhudas KURANI, Mumbai (IN); Madhavlal Govindlal (57) ABSTRACT PATEL, Mumbai (IN) (73) Assignee: THEMIS MEDICARE LIMITED, The present invention relates to pharmaceutical compositions Mumbai (IN) of various pharmaceutical actives, especially lyophilic and hydrophilic actives containing Diethylene glycol monoethyl (21) Appl. No.: 14/242,973 ether or other alkyl derivatives thereofas a primary vehicle and/or to pharmaceutical compositions utilizing Diethylene (22) Filed: Apr. 2, 2014 glycol monoethyl ether or other alkyl derivatives thereofas a primary vehicle or as a solvent system in preparation of Such (30) Foreign Application Priority Data pharmaceutical compositions. The pharmaceutical composi Apr. 2, 2013 (IN) ......................... 1287/MUMA2013 tions of the present invention are safe, non-toxic, exhibits enhanced physical stability compared to conventional formu Publication Classification lations containing such pharmaceutical actives and are Suit able for use as injectables for intravenous and intramuscular (51) Int. Cl. administration, as well as for use as a preformed solution/ A647/ (2006.01) liquid for filling in and preparation of capsules, tablets, nasal A6 IK 45/06 (2006.01) sprays, gargles, dermal applications, gels, topicals, liquid oral A6 IK9/00 (2006.01) dosage forms and other dosage forms. -

Package Leaflet
Page 1 PACKAGE LEAFLET Page 2 PACKAGE LEAFLET: INFORMATION FOR THE USER Cleviprex 0.5 mg/ml emulsion for injection Clevidipine Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. - If you have any further questions, ask your doctor. - If you get any of the side effects, talk to your doctor. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet: 1. What Cleviprex is and what it is used for 2. What you need to know before you are given Cleviprex 3. How Cleviprex is used 4. Possible side effects 5. How to store Cleviprex 6. Contents of the pack and other information 1. What Cleviprex is and what it is used for Cleviprex contains the active substance clevidipine. Clevidipine is a calcium channel blocker. Calcium channel blockers are medicines which lower blood pressure. Cleviprex is used to lower blood pressure in adult patients preparing for surgery, undergoing surgery or immediately after surgery. Page 3 2. What you need to know before you are given Cleviprex Do not use Cleviprex: - if you are allergic (hypersensitive) to clevidipine, soybeans, soya-bean oil, soy products, peanut, eggs or egg products or to any of the other ingredients of this medicine (listed in section 6) - if you have disorders of lipid metabolism (difficulties processing fats), such as extremely high levels of fat in your blood (pathologic hyperlipidaemia), a kidney disorder that causes loss of protein in urine (lipoid nephrosis) or inflammation of the pancreas (acute pancreatitis) if it is accompanied by high levels of fat in the blood (hyperlipidaemia) - if you suffer from severe aortic stenosis (severe narrowing of one of the valves in the heart) - Check with your doctor if you are unsure. -

View Pdf Copy of Original Document
Phenotype definition for the Vanderbilt Genome-Electronic Records project Identifying genetics determinants of normal QRS duration (QRSd) Patient population: • Patients with DNA whose first electrocardiogram (ECG) is designated as “normal” and lacking an exclusion criteria. • For this study, case and control are drawn from the same population and analyzed via continuous trait analysis. The only difference will be the QRSd. Hypothetical timeline for a single patient: Notes: • The study ECG is the first normal ECG. • The “Mildly abnormal” ECG cannot be abnormal by presence of heart disease. It can have abnormal rate, be recorded in the presence of Na-channel blocking meds, etc. For instance, a HR >100 is OK but not a bundle branch block. • Y duration = from first entry in the electronic medical record (EMR) until one month following normal ECG • Z duration = most recent clinic visit or problem list (if present) to one week following the normal ECG. Labs values, though, must be +/- 48h from the ECG time Criteria to be included in the analysis: Criteria Source/Method “Normal” ECG must be: • QRSd between 65-120ms ECG calculations • ECG designed as “NORMAL” ECG classification • Heart Rate between 50-100 ECG calculations • ECG Impression must not contain Natural Language Processing (NLP) on evidence of heart disease concepts (see ECG impression. Will exclude all but list below) negated terms (e.g., exclude those with possible, probable, or asserted bundle branch blocks). Should also exclude normalization negations like “LBBB no longer present.” -

Contrast Echocardiography
4MEDICAL REVIEW Contrast Echocardiography Mark A. Friedman Echocardiography Laboratory Barnes-Jewish Hospital Washington University School of Medicine St. Louis, MO 53110 ABSTRACT CONTRAST AGENTS Ultrasound contrast agents are widely used in clinical The ability to opacify vascular structures on echocardio- practice for left ventricle opacification in sub-optimal grams by injecting agitated saline solution has been well echocardiograms. Recently, significant research has recognized for more than thirty years (Gramiak and Shah, focused on the use of contrast echocardiography as a 1968). Early contrast agents were produced by manually non-invasive means to evaluate myocardial perfusion. agitating solutions such as saline, yielding bubbles that Advances in contrast agents as well as ultrasound tech- provided brief ultrasound contrast by scattering the nology have enabled investigations into myocardial con- incoming ultrasound energy before dissolving rapidly in trast echocardiography as a possible alternative to blood. These hand-agitated intravenous solutions have nuclear imaging studies. This review will focus on the been shown to be safe and are still used clinically to pro- development and current uses of contrast echocardiog- vide brief contrast during echocardiograms for evaluating raphy, as well as future indications, including myocardial cardiac shunts and patent foramen ovale (Bommer et al., perfusion and risk stratification following myocardial 1984). Hand-agitated intravenous solutions, however, infarction. cannot be used to evaluate left-sided cardiac chambers because the bubbles have neither a small enough size nor the stability to cross the pulmonary vasculature. (Table 1) INTRODUCTION Echocardiography has become a standard tool in the TABLE 1 PROPERTIES OF AN IDEAL ECHOCARDIOGRAPHIC CONTRAST AGENT evaluation and diagnosis of a wide range of cardiac con- ditions. -

Table 6.12: Deaths from Poisoning, by Sex and Cause, Scotland, 2015
Table 6.12: Deaths from poisoning, by sex and cause, Scotland, 2015 ICD code(s), cause of death and substance(s) 1 Both Males Females ALL DEATHS FROM POISONING 2 941 632 309 ACCIDENTS 662 471 191 X40 - X49 Accidental poisoning by and exposure to … X40 - Nonopioid analgesics, antipyretics and antirheumatics Paracetamol 2 0 2 Paracetamol, Codeine || Diazepam, Amitriptyline, Mirtazapine, Dihydrocodeine, Cannabis, Alcohol 1 0 1 Paracetamol, Dihydrocodeine, Tramadol || 1 1 0 X41 - Antiepileptic, sedative-hypnotic, antiparkinsonism and psychotropic drugs, not elsewhere classified Amitriptyline || Tramadol, Diazepam 1 0 1 Amitriptyline || Venlafaxine, Dihydrocodeine 1 0 1 Amitriptyline, Alcohol 1 0 1 Amitriptyline, Alcohol || Fluoxetine 1 0 1 Amitriptyline, Clomipramine, Gabapentin, Tramadol, Methadone 1 0 1 Amitriptyline, Gabapentin, Fluoxetine || Paracetamol, Diazepam, Tramadol, Cannabis 1 0 1 Amitriptyline, Oxycodone || Pregabalin 1 0 1 Amitriptyline, Zopiclone, Oxycodone, Venlafaxine, Pregabalin 1 0 1 Amphetamine || Diazepam 1 0 1 Amphetamine || Diazepam, Cannabis 1 0 1 Amphetamine || Diazepam, Paracetamol, Alcohol 1 1 0 Amphetamine || Dihydrocodeine, Alcohol 1 0 1 Amphetamine, Citalopram || Diazepam, Cannabis, Alcohol 1 0 1 Citalopram, Alcohol 2 1 1 Citalopram, Cyclizine || Temazepam 1 1 0 Diazepam, Alcohol || 2 2 0 Diazepam, Dihydrocodeine || Pregabalin, Venlafaxine, Quetiapine 1 1 0 Diazepam, Dihydrocodeine, Alcohol || 1 1 0 Diazepam, Methadone, Mirtazapine || 1 0 1 Dothiepin 1 0 1 Ecstasy, Cocaine, Alcohol 1 1 0 Ethylphenidate, Diazepam, -

Variation in Outcomes Among 24/7 Percutaneous Coronary Intervention Centres For
Title: Variation in Outcomes Among 24/7 Percutaneous Coronary Intervention Centres for Patients Resuscitated from Out-of-Hospital Cardiac Arrest. Authors: Bryn E. Mumma, MD, MAS1; Machelle D. Wilson, PhD2; María F. García-Pintos, MD1; Pablo J. Erramouspe, MD1 Daniel J. Tancredi, PhD3 Author Affiliations: Departments of 1Emergency Medicine, 2Public Health Sciences, and 3Pediatrics, University of California Davis, Sacramento, CA. Address for Correspondence: Bryn E. Mumma, MD, MAS 4150 V Street, PSSB #2100 Sacramento, CA 95817 Fax: 916-734-7950 Email: [email protected] Phone: 916-734-5010 Running Title: Variation in OHCA Outcomes Source of support: The project described was supported by the National Heart, Lung, and Blood Institute (NHLBI) through grant #5K08HL130546. Word count abstract: 250 Word count paper: 2,409 Number of figures and tables: 5 Conflict of Interest declaration: The authors have no conflicts of interest to disclose. All authors have reviewed and approved the final manuscript. ABSTRACT Background: Patients treated at 24/7 percutaneous coronary intervention (PCI) centres following out-of-hospital cardiac arrest (OHCA) have better outcomes than those treated at non-24/7 PCI centres. However, variation in outcomes between 24/7 PCI centres is not well studied. Objectives: To evaluate variation in outcomes among 24/7 PCI centres and to assess stability of 24/7 PCI centre performance. Methods: Adult patients in the California Office of Statewide Health Planning and Development Patient Discharge Database with a "present on admission" diagnosis of cardiac arrest admitted to a 24/7 PCI centre from 2011 to 2015 were included. Primary outcome was good neurologic recovery at hospital discharge. -

Real-Time Magnetic Resonance Imaging-Guided Coronary Catheterization in Swine
Real-Time Magnetic Resonance Imaging-Guided Coronary Catheterization in Swine R. A. Omary1, J. D. Green1, B. Schirf1, Y. Li1, J. Carr1, J. P. Finn1, D. Li1 1Northwestern University, Chicago, IL, United States Synopsis: In 11 swine, we performed real-time MRI-guided left coronary artery catheterization from a percutaneous femoral artery approach. A 0.30-inch diameter active guidewire was coaxially inserted within 6 or 7-French Judkins left coronary catheters. The catheter was filled with 4% contrast agent and tracked using an inversion-recovery-prepared spoiled gradient echo sequence at 7 frames/s. The guidewire was tracked using steady-state precession imaging at 9 frames/s. Selective MR coronary angiography with injections of dilute contrast agent was used to verify catheter positioning. Left coronary artery catheterization under MRI guidance was successful in 11/11 pigs (100%). Introduction: Catheter-based coronary MR angiography is feasible using dilute contrast agent injections (1). The coronary catheterization for these injections has been performed under x-ray (1) or MRI (2) guidance, using surgical carotid artery access. The surgical carotid approach is less technically demanding than the percutaneous femoral artery approach because of the more direct and shorter route to the coronary ostium. An active internal guidewire used in conjunction with a contrast agent-filled catheter is one technique (3) to improve signal detection of endovascular devices, which in turn can be used to improve the spatial and temporal resolution of endovascular device tracking. Using this technique, we tested the hypothesis that MRI can guide coronary artery catheterization in swine via a percutaneous femoral artery approach. -

Early Outcomes of Percutaneous Pulmonary Valve Implantation with Pulsta and Melody Valves: the First Report from Korea
Journal of Clinical Medicine Article Early Outcomes of Percutaneous Pulmonary Valve Implantation with Pulsta and Melody Valves: The First Report from Korea Ah Young Kim 1,2 , Jo Won Jung 1,2, Se Yong Jung 1,2 , Jae Il Shin 1,2 , Lucy Youngmin Eun 1,2 , Nam Kyun Kim 3 and Jae Young Choi 1,2,* 1 Division of Pediatric Cardiology, Center for Congenital Heart Disease, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul 03722, Korea; [email protected] (A.Y.K.); [email protected] (J.W.J.); [email protected] (S.Y.J.); [email protected] (J.I.S.); [email protected] (L.Y.E.) 2 Department of Pediatrics, Yonsei University College of Medicine, Seoul 03722, Korea 3 Department of Pediatrics, Emory University, Atlanta, GA 30322, USA; [email protected] * Correspondence: [email protected] Received: 25 July 2020; Accepted: 24 August 2020; Published: 26 August 2020 Abstract: Percutaneous pulmonary valve implantation (PPVI) is used to treat pulmonary stenosis (PS) or pulmonary regurgitation (PR). We described our experience with PPVI, specifically valve-in-valve transcatheter pulmonary valve replacement using the Melody valve and novel self-expandable systems using the Pulsta valve. We reviewed data from 42 patients undergoing PPVI. Twenty-nine patients had Melody valves in mostly bioprosthetic valves, valved conduits, and homografts in the pulmonary position. Following Melody valve implantation, the peak right ventricle-to-pulmonary artery gradient decreased from 51.3 11.5 to 16.7 3.3 mmHg and right ventricular systolic pressure ± ± fell from 70.0 16.8 to 41.3 17.8 mmHg. -

Reference ID: 3055639 Cleviprex™ (Clevidipine) Draft Labeling, Page 2
HIGHLIGHTS OF PRESCRIBING INFORMATION ----------------------------CONTRAINDICATIONS------------------------------ These highlights do not include all the information needed to use Cleviprex is contraindicated in patients with: Cleviprex safely and effectively. See full prescribing information for • Allergy to soy or eggs (4.1) Cleviprex. • Defective lipid metabolism (4.2) • Severeaortic stenosis (4.3) Cleviprex (clevidipine)injectableemulsion, for intravenous use Initial U.S. Approval: 2008 ---------------------WARNINGS AND PRECAUTIONS-------------------------- • Maintain aseptic technique.Discard unused portion 12 hours after stopper -------------------------INDICATIONS AND USAGE---------------------------- puncture. (5.1) Cleviprex is a dihydropyridine calcium channel blocker indicated for the • Hypotension and reflex tachycardiaare potential consequences of rapid reduction of blood pressure when oral therapy is not feasible or not desirable. upward titration of Cleviprex. (5.2) (1) • Dihydropyridine calcium channel blockers can produce negative inotropic effects and exacerbate heart failure. Monitor heart failure patients -----------------------DOSAGE AND ADMINISTRATION-------------------- carefully(5.4) For intravenous use:Cleviprex is intended for intravenous use.Titrate • Cleviprex gives no protection against the effects of abrupt beta-blocker Cleviprex to achieve the desired blood pressure reduction. Individualize withdrawal. (5.5) dosage depending on the blood pressure response of the patient and the goal • Patients who receive prolonged Cleviprex infusions and are not blood pressure. (2.2) transitioned to other antihypertensive therapies should be monitored for the Monitoring: Monitor blood pressure and heart rate during infusion, and until possibility of rebound hypertension for at least 8 hours after the infusion is vital signs stabilize. (2.1) stopped. (5.6) Initial dose:Initiate intravenous infusion of Cleviprex at 1- 2 mg/hour. (2.2) Dose titration:Double the dose at short (90 second) intervalsinitially.