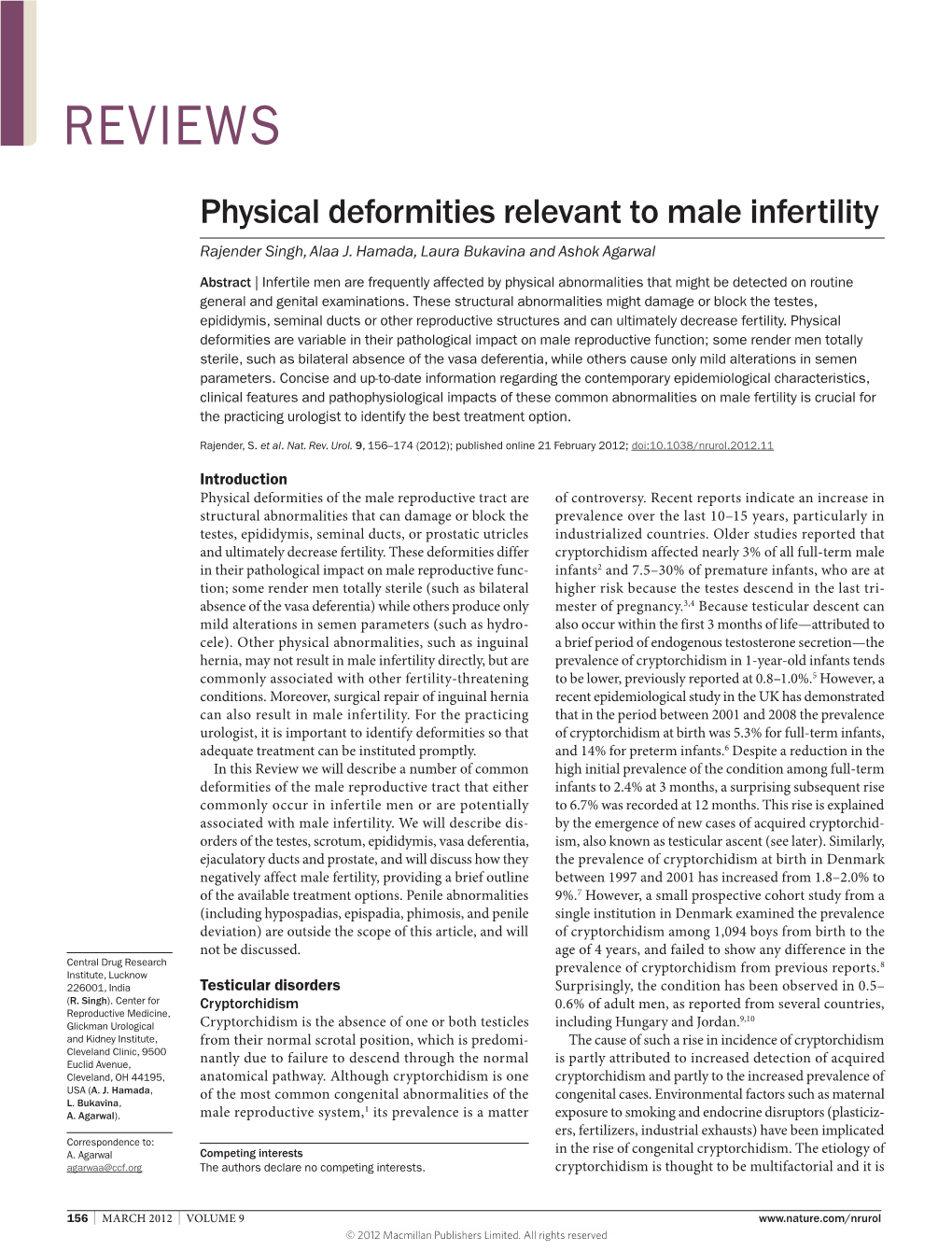
Physical Deformities Relevant to Male Infertility Rajender Singh, Alaa J
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Male Reproductive System
Management of Men’s Reproductive 3 Health Problems Men’s Reproductive Health Curriculum Management of Men’s Reproductive 3 Health Problems © 2003 EngenderHealth. All rights reserved. 440 Ninth Avenue New York, NY 10001 U.S.A. Telephone: 212-561-8000 Fax: 212-561-8067 e-mail: [email protected] www.engenderhealth.org This publication was made possible, in part, through support provided by the Office of Population, U.S. Agency for International Development (USAID), under the terms of cooperative agreement HRN-A-00-98-00042-00. The opinions expressed herein are those of the publisher and do not necessarily reflect the views of USAID. Cover design: Virginia Taddoni ISBN 1-885063-45-8 Printed in the United States of America. Printed on recycled paper. Library of Congress Cataloging-in-Publication Data Men’s reproductive health curriculum : management of men’s reproductive health problems. p. ; cm. Companion v. to: Introduction to men’s reproductive health services, and: Counseling and communicating with men. Includes bibliographical references. ISBN 1-885063-45-8 1. Andrology. 2. Human reproduction. 3. Generative organs, Male--Diseases--Treatment. I. EngenderHealth (Firm) II. Counseling and communicating with men. III. Title: Introduction to men’s reproductive health services. [DNLM: 1. Genital Diseases, Male. 2. Physical Examination--methods. 3. Reproductive Health Services. WJ 700 M5483 2003] QP253.M465 2003 616.6’5--dc22 2003063056 Contents Acknowledgments v Introduction vii 1 Disorders of the Male Reproductive System 1.1 The Male -

Hypospadias by Ronald S
Kapi‘olani Pediatric Urology Hypospadias By Ronald S. Sutherland, M.D., F.A.A.P., F.A.C.S. What is hypospadias? Defined as a congenital deformity where the urethral opening is located beneath the penis rather then the tip, hypospadias ranges from a mild to severe deformity. The more common form is the distal variety, with the opening toward the front of the penis, which can usually be repaired with pleasing cosmetic results. More severe forms may be associated with the opening located at the base of the penis or further back near the anus. Usually hypospadias is also present with downward curvature of the penis (chordee), and a flattening of the foreskin with a hood-like covering. Occasionally the scrotum is also malformed and appears higher around the penis. Hypospadias can be found in a variety of congenital syndromes, including those with cardiac, renal, and testicular anomalies. (see next page) What causes hypospadias? Hypospadias develops early in gestation and occurs for unknown reasons, although there is slight familial tendency. Recent evidence suggests that the incidence is increasing and may be linked to environmental and genetic disruptions during the period when genital development is particularly sensitive to sex-steroid hormone imbalances. Occasionally, hypospadias can be detected by prenatal ultrasound. No pre-natal treatment or intervention is available. Parents should not request a circumcision for their newborn son with hypospadias because the foreskin may be necessary to assist with surgical repair. Sometimes hypospadias is not recognized until after the circumcision is completed. These cases are usually mild forms that can be repaired without the use of foreskin. -

Hypospadias Repair
Patient and Family Education Hypospadias Repair What causes it? What is hypospadias? Incomplete development of the urethra causes Hypospadias is a birth defect of the penis. hypospadias. It can occur in families. The The urethral opening, the hole where the urine comes out, is not in the normal position. reason for it happening is usually not known. Instead of the tip, it is on the undersurface of Why is it important to recognize the penis. Boys with hypospadias are usually hypospadias? missing the underside of their foreskin so An abnormally placed urethral opening does that the foreskin forms a hood. For this not allow the urine to pass as it s hould. A reason, most boys born with boy with hypospadias urinates with a hypospadias are not circumcised. There is stream that is often directed downward often a bend or curve (called chordee) in the rather than out and away from the body. This penis when the boy has an erection. causes wet pants and shoes. This condition, Hypospadias may be mild, moderate, or when left uncorrected, may make future severe depending on how far back the opening sexual intercourse difficult, or is and how much curvature is present. The impossible. more severe forms of hypospadias are usually associated with worsening degrees of chordee. Can it be corrected? Yes, surgery can correct the problem. These operations are best done between 6 and 18 months of age. The repair is usually performed in one surgery. If the hypospadias is severe, it may be necessary to have more than one surgery. The Normal position for urethra surgery usually lasts 1-3 hours and the patient goes home the same day. -
1997 Asa Program.Pdf
Friday, February 21 12:00 NOON- 11:00 PM Executive Council Meeting (lunch and supper served) (Chesapeake Room NB) Saturday, February 22 8:00-9:40 AM Postgraduate Course (Constellation 3:00-5:00 PM Postgraduate Course (Constellation Ballroom A) Ballroom A) 9:40-1 0:00 AM Refreshment Break 6:00-7:00 PM Student Mixer (Maryland Suites-Balti 10:00-12:00 NOON Postgraduate Course (Constellation more Room) Ballroom A) 7:00-9:00 PM ASA Welcoming Reception (Atrium 12:00-1 :00 PM Lunch (on your own) Lobby) 7:00-9:00 PM Exhibits Open (Constellation Ball I :00-2:40 PM Postgraduate Course (Constellation Ballroom A) rooms E, F) 2:40-3:00 PM Refreshment Break 9:00- 1 I :00 PM Executive Council Meeting (Chesa peake Room NB) Sunday, February 23 7:45-8:00 AM Welcome and Opening Remarks 12:00-1 :30 PM Women in Andrology Luncheon (Ches (Constellation Ballroom A) apeake Room NB) 8:00-9:00 AM Serono Lecture: "Genetics of Prostate Business Meeting 12:00-12:30 Cancer" Patrick Walsh (Constellation Speaker and Lunch 12:30-1:30 Ballroom A) I :30-3:00 PM Symposium I: "Regulation of Testicu 9:00-10:00 AM American Urological Association Lec lar Growth and Function" (Constellation ture: "New Medical Treatments of Im Ballroom A) potence" Irwin Goldstein (Constella Patricia Morris tion Ballroom A) Martin Matzuk 10:00-10:30 AM Refreshment Break/Exhibits 3:00-3:30 PM Refreshment Break/Exhibits (Constellation Ballrooms E, F) (Constellation Ballrooms E, F) 10:30-12:00 NOON Oral Session I: "Genes and Male Repro 3:30-4:30 PM Oral Session II: "Calcium Channels duction" (Constellation Ballroom A) and Male Reproduction" (Constellation Ballroom A) 12:00- 1 :30 PM Lune (on your own) � 4:30-6:30 PM Poster Session I (Constellation Ball �4·< rooms C, D) \v\wr 7:30-11:00 PM Banquet (National Aquarium) Monday, February 24 7:00-8:00 AM Past Presidents' Breakfast 12:00-1 :30 PM Simultaneous Events: (Pratt/Calvert Rooms) I. -
Andrology User Handbook
Document code: AY.P001 Version number: 7 Date of issue: 29/06/2020 USER HANDBOOK FOR ANDROLOGY SERVICES Diagnostic Semen Analysis Post Vasectomy Semen Analysis Retrograde Ejaculation Analysis Page 1 of 24 Document code: AY.P001 Version number: 7 Date of issue: 29/06/2020 Contents: 1. Introduction .................................................................................................................... 3 2. Location and Opening Times .......................................................................................... 4 3. Useful contacts ............................................................................................................... 4 4. Services provided by the laboratory ............................................................................... 5 5. Requesting semen analysis ............................................................................................ 5 6. Analysis test types .......................................................................................................... 8 6.1 Diagnostic semen analysis (DSA) test for fertility ......................................................... 8 6.1a Instructions for collection of a semen sample for DSA (fertility)............................... 9 6.1b How Diagnostic Semen Analysis assessments are reported .................................10 6.2 Retrograde Analysis ....................................................................................................11 6.2a Instructions for collection of urine for retrograde ejaculation -
Restoration of Fertility by Gonadotropin Replacement in a Man With
J Rohayem and others Fertility in hypogonadotropic 170:4 K11–K17 Case Report CAH with TARTs Restoration of fertility by gonadotropin replacement in a man with hypogonadotropic azoospermia and testicular adrenal rest tumors due to untreated simple virilizing congenital adrenal hyperplasia Julia Rohayem1, Frank Tu¨ ttelmann2, Con Mallidis3, Eberhard Nieschlag1,4, Sabine Kliesch1 and Michael Zitzmann1 Correspondence should be addressed 1Center of Reproductive Medicine and Andrology, Clinical Andrology, University of Muenster, Albert-Schweitzer- to J Rohayem Campus 1, Building D11, D-48149 Muenster, Germany, 2Institute of Human Genetics and 3Institute of Reproductive Email and Regenerative Biology, Center of Reproductive Medicine and Andrology, University of Muenster, Muenster, Julia.Rohayem@ Germany and 4Center of Excellence in Genomic Medicine Research, King Abdulaziz University, Jeddah, Saudi Arabia ukmuenster.de Abstract Context: Classical congenital adrenal hyperplasia (CAH), a genetic disorder characterized by 21-hydroxylase deficiency, impairs male fertility, if insufficiently treated. Patient: A 30-year-old male was referred to our clinic for endocrine and fertility assessment after undergoing unilateral orchiectomy for a suspected testicular tumor. Histopathological evaluation of the removed testis revealed atrophy and testicular adrenal rest tumors (TARTs) and raised the suspicion of underlying CAH. The remaining testis was also atrophic (5 ml) with minor TARTs. Serum 17-hydroxyprogesterone levels were elevated, cortisol levels were at the lower limit of normal range, and gonadotropins at prepubertal levels, but serum testosterone levels were within the normal adult range. Semen analysis revealed azoospermia. CAH was confirmed by a homozygous mutation g.655A/COG (IVS2-13A/COG) in European Journal of Endocrinology CYP21A2. Hydrocortisone (24 mg/m2) administered to suppress ACTH and adrenal androgen overproduction unmasked deficient testicular testosterone production. -

GERONTOLOGICAL NURSE PRACTITIONER Review and Resource M Anual
13 Male Reproductive System Disorders Vaunette Fay, PhD, RN, FNP-BC, GNP-BC GERIATRIC APPRoACH Normal Changes of Aging Male Reproductive System • Decreased testosterone level leads to increased estrogen-to-androgen ratio • Testicular atrophy • Decreased sperm motility; fertility reduced but extant • Increased incidence of gynecomastia Sexual function • Slowed arousal—increased time to achieve erection • Erection less firm, shorter lasting • Delayed ejaculation and decreased forcefulness at ejaculation • Longer interval to achieving subsequent erection Prostate • By fourth decade of life, stromal fibrous elements and glandular tissue hypertrophy, stimulated by dihydrotestosterone (DHT, the active androgen within the prostate); hyperplastic nodules enlarge in size, ultimately leading to urethral obstruction 398 GERONTOLOGICAL NURSE PRACTITIONER Review and Resource M anual Clinical Implications History • Many men are overly sensitive about complaints of the male genitourinary system; men are often not inclined to initiate discussion, seek help; important to take active role in screening with an approach that is open, trustworthy, and nonjudgmental • Sexual function remains important to many men, even at ages over 80 • Lack of an available partner, poor health, erectile dysfunction, medication adverse effects, and lack of desire are the main reasons men do not continue to have sex • Acute and chronic alcohol use can lead to impotence in men • Nocturia is reported in 66% of patients over 65 – Due to impaired ability to concentrate urine, reduced -

Male Infertility
www.livestrong.org.livestrong.org Male Infertility Some male cancer survivors find that they are not able to have children due to the effects of cancer treatment. By identifying your risk for infertility, you can take steps before treatment to preserve your fertility. For survivors who have already completed treatment, there are other options for having children. Male Infertility: Detailed Information This infinformationormation is meant to be a general introduction to this topic. The purpose is to provide a starting point for you to become more informed about important matters that may be affecting your life as a survivor and to provide ideas about steps you can take to learn more. This information is not intended nor should it be interpreted as providing professional medical, legal and financial advice. You should consult a trained professional for more information. Please read the Suggestions (http://www.livestrong.org/Get-Help/Learn-About-Cancer/Cancer-Support-Topics/Physical-Effects-of- Cancer/Male-Infertility#a#a) and Additional Resources (http://www.livestrong.org/Get-Help/Learn- About-Cancer/Cancer-Support-Topics/Physical-Effects-of-Cancer/Male-Infertility#a#a) sections for questions to ask and for more resources. Cancer and treatment may put survivors at risk for infertility. Male infertility generally means an inability to produce healthy sperm or to ejaculate sperm. There are many different causes of infertility in cancer survivors including physical and emotional. Certain treatments can cause or contribute to this condition. It is best to discuss the risks of infertility with your doctor before cancer treatment begins. However, there are options for survivors who experience infertility as a result of cancer or treatment. -

This Document Was Released in November 2020. This Document Will Continue to Be Periodically Updated to Reflect the Growing Body of Literature Related to This Topic
MEDICAL STUDENT CURRICULUM This document was released in November 2020. This document will continue to be periodically updated to reflect the growing body of literature related to this topic. Help: Andrew Gusev - [email protected] MALE INFERTILITY KEYWORDS: infertility, azoospermia, oligospermia, semen analysis, varicocele LEARNING OBJECTIVES: At the end of medical school, the medical student will be able to… 1. Describe the hypothalamus-pituitary-gonadal (HPG) axis 2. Describe the workup for male infertility, including the importance of the physical exam 3. Restate the limitations of the semen analysis 4. List some common reversible causes of infertility and their treatments 5. Recognize when to refer a patient for ART Introduction Approximately 15% of couples will be unable to conceive after attempting unprotected intercourse for one year. Of these couples, about 50% of them will have some male factor to that is contributing to their infertility (a male factor is the sole reason in approximately 20% of infertile couples). (Thonneau P, 1991) Male infertility can be due to a variety of genetic, anatomic, and environmental conditions, many of which will be briefly discussed below. When a cause for an abnormal semen analysis cannot be found, it is termed idiopathic. When a man is infertile with a normal semen analysis and workup, the term unexplained infertility is used. As the word suggests, these men do not have a known cause for their infertility but it is thought to likely be due genetic defects that have not been described yet. The purpose of evaluation is to identify possible conditions causing infertility and treating reversible conditions which may improve a man’s fertility potential. -
Guidelines on Paediatric Urology S
Guidelines on Paediatric Urology S. Tekgül, H. Riedmiller, E. Gerharz, P. Hoebeke, R. Kocvara, R. Nijman, Chr. Radmayr, R. Stein European Society for Paediatric Urology © European Association of Urology 2011 TABLE OF CONTENTS PAGE 1. INTRODUCTION 6 1.1 Reference 6 2. PHIMOSIS 6 2.1 Background 6 2.2 Diagnosis 6 2.3 Treatment 7 2.4 References 7 3. CRYPTORCHIDISM 8 3.1 Background 8 3.2 Diagnosis 8 3.3 Treatment 9 3.3.1 Medical therapy 9 3.3.2 Surgery 9 3.4 Prognosis 9 3.5 Recommendations for crytorchidism 10 3.6 References 10 4. HYDROCELE 11 4.1 Background 11 4.2 Diagnosis 11 4.3 Treatment 11 4.4 References 11 5. ACUTE SCROTUM IN CHILDREN 12 5.1 Background 12 5.2 Diagnosis 12 5.3 Treatment 13 5.3.1 Epididymitis 13 5.3.2 Testicular torsion 13 5.3.3 Surgical treatment 13 5.4 Prognosis 13 5.4.1 Fertility 13 5.4.2 Subfertility 13 5.4.3 Androgen levels 14 5.4.4 Testicular cancer 14 5.4.5 Nitric oxide 14 5.5 Perinatal torsion 14 5.6 References 14 6. Hypospadias 17 6.1 Background 17 6.1.1 Risk factors 17 6.2 Diagnosis 18 6.3 Treatment 18 6.3.1 Age at surgery 18 6.3.2 Penile curvature 18 6.3.3 Preservation of the well-vascularised urethral plate 19 6.3.4 Re-do hypospadias repairs 19 6.3.5 Urethral reconstruction 20 6.3.6 Urine drainage and wound dressing 20 6.3.7 Outcome 20 6.4 References 21 7. -

Torsion of the Testicular Appendages in Adult Acute Scrotum
International Journal of Clinical Urology 2019; 3(2): 40-45 http://www.sciencepublishinggroup.com/j/ijcu doi: 10.11648/j.ijcu.20190302.13 ISSN: 2640-1320 (Print); ISSN: 2640-1355 (Online) Torsion of the Testicular Appendages in Adult Acute Scrotum Seiichi Saito Art Park Urology Hospital & Clinic, Sapporo, Japan Email address: To cite this article: Seiichi Saito. Torsion of the Testicular Appendages in Adult Acute Scrotum. International Journal of Clinical Urology. Vol. 3, No. 2, 2019, pp. 40-45. doi: 10.11648/j.ijcu.20190302.13 Received: August 28, 2019; Accepted: October 15, 2019; Published: October 26, 2019 Abstract: Adult patients with acute scrotum sometimes tend to be treated for epididymitis without undergoing ultrasonographic examination, although precise ultrasonography reveals that there are some patients with torsion of the testicular appendages. In this report, I investigate the incidence of patients with torsion of the testicular appendages among patients with adult acute scrotum, who mainly used to be treated for epididymitis. In the last 5 years, 46 patients (23~62, average age 43.5 years) with scrotal pain and swelling visited our clinic for diagnosis and treatment. On an outpatient basis, their symptoms were evaluated, and blood tests, urinalysis, and grey scale and color Doppler ultrasonography with a 5-12 MHz linear scan were performed. Five (10.9%) of the 46 patients were diagnosed as having torsion of the testicular appendages. Although none of them had a high fever, 4 of the 5 (80%) had nausea and abdominal pain. Leukocytosis and pyuria were not found in any case. Typical ultrasound appearances were reactive hydrocele and a hyperechoic swollen mass or enlarged hyperechoic, spherical mass of the appendage. -

Let's Talk About What's Hard
Let’s Talk About What’s Hard “Bobby” Duc Tran, MD, MSc Assistant Professor, Emory University 2017 HoG State Meeting Case Presentation March 3, 2017 WARNING The following presentation contains some foul language, nudity, and images that some viewers may find upsetting Case Presentation • 32yo white male • Past medical history: • severe hemophilia B • hemophilic arthropathy of bilateral knees and elbows • Marfan’s syndrome • atrial fibrillation • blind in one eye • hepatitis C • Current hemophilia treatment: Aprolix • Previous issues with mixing the factor. Case Presentation • Past surgeries: • Aortic root repair • Full dentition extraction • Bilateral knee arthroscopic synevectomies at 5 and 7 yo • Left orchiectomy for testicular torsion • Last seen in clinic for his annual comprehensive visit in 9/2016 Case Presentation • Called to the HTC clinic nurse on 12/5/2016 • Embarrassingly he reported: • This morning “my penis and testicles are blackish purple and feels like a bleed” • I had sex with my wife last night • Last infused 3 days ago and is not due for next infusion until tomorrow • “This has never happened before” How to talk about this? • Approach from a professional standpoint • Discuss these topics when discussing safe sexual practices • Gauge the patient’s comfort with using medical terms • Nicknames used: • Dick, dong, schlong, wiener, peen, so many more • Not wenis What to do first? • When was the bleeding recognized? • Did you hear/feel a “pop”? • Recognize associated injuries • Urethra, bladder, vascular • Consider GU referral