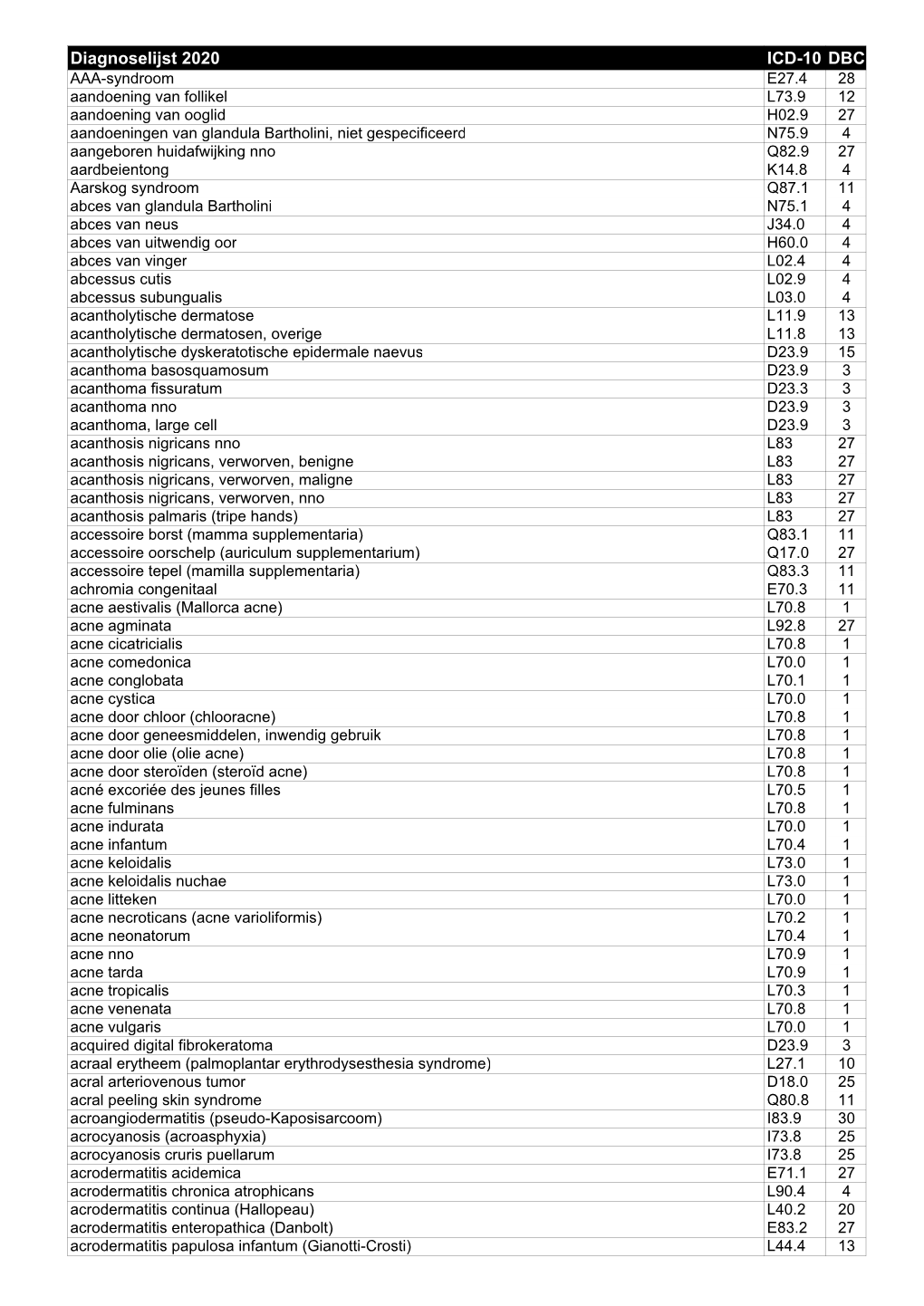
Diagnoselijst Dermatologie 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Systematized Verrucous Epidermal Nevus- a Case Report
Jebmh.com Case Report Systematized Verrucous Epidermal Nevus- A Case Report B.C. Sharathkumar1, N.S. Anitha2 1Professor and HOD, Department of Dermatology, Venereology and Leprosy, Kempegowda Institute of Medical Sciences Hospital and Research Centre, Bengaluru, Karnataka. 2Resident, Department of Dermatology, Venereology and Leprosy, Kempegowda Institute of Medical Sciences Hospital and Research Centre, Bengaluru, Karnataka. INTRODUCTION Veracious epidermal nevus (VEN) is a keratinocyte hematoma, usually present at Corresponding Author: birth or can develop later in life.1,2 It commonly involves trunk and limbs. Less Dr. N. S. Anitha, Resident, commonly, involved sites are head and neck; face is known to involve even more Department of Dermatology, 3,4,5 rarely. Clinical variants of VEN are zosteriform, linear, unilateral or systematized Venereology and Leprosy, 6 patterns with streaks and swirls. We report a case of girl who presented with Kempegowda Institute of Medical extensive VEN causing a lot of disfigurement. Epidermal nevi are hamartomas of Sciences Hospital and Research Centre, cutaneous structures arising from the embryonic ectoderm. The prevalence rate is Bengaluru- 560004, Karnataka. 1 in 1000, without predilection to race and sex.7,8 They are further divided into E-mail: [email protected] nonorganoid (Keratinocytic) types and organoid types (due to hyperplasia of DOI: 10.18410/jebmh/2019/637 adnexal structures such as sebaceous glands, sweat glands and hair follicles).8,9 Financial or Other Competing Interests: All epidermal nevi represents disorder of dermo-epidermal interactions and most None. cases are sporadic. Verrucous epidermal nevus is the most common type of keratinocyte nevus and derives its name from its keratotic and warty appearance. -

3628-3641-Pruritus in Selected Dermatoses
Eur opean Rev iew for Med ical and Pharmacol ogical Sci ences 2016; 20: 3628-3641 Pruritus in selected dermatoses K. OLEK-HRAB 1, M. HRAB 2, J. SZYFTER-HARRIS 1, Z. ADAMSKI 1 1Department of Dermatology, University of Medical Sciences, Poznan, Poland 2Department of Urology, University of Medical Sciences, Poznan, Poland Abstract. – Pruritus is a natural defence mech - logical self-defence mechanism similar to other anism of the body and creates the scratch reflex skin sensations, such as touch, pain, vibration, as a defensive reaction to potentially dangerous cold or heat, enabling the protection of the skin environmental factors. Together with pain, pruritus from external factors. Pruritus is a frequent is a type of superficial sensory experience. Pruri - symptom associated with dermatoses and various tus is a symptom often experienced both in 1 healthy subjects and in those who have symptoms systemic diseases . Acute pruritus often develops of a disease. In dermatology, pruritus is a frequent simultaneously with urticarial symptoms or as an symptom associated with a number of dermatoses acute undesirable reaction to drugs. The treat - and is sometimes an auxiliary factor in the diag - ment of this form of pruritus is much easier. nostic process. Apart from histamine, the most The chronic pruritus that often develops in pa - popular pruritus mediators include tryptase, en - tients with cholestasis, kidney diseases or skin dothelins, substance P, bradykinin, prostaglandins diseases (e.g. atopic dermatitis) is often more dif - and acetylcholine. The group of atopic diseases is 2,3 characterized by the presence of very persistent ficult to treat . Persistent rubbing, scratching or pruritus. -

Atypical Compound Nevus Arising in Mature Cystic Ovarian Teratoma
J Cutan Pathol 2005: 32: 71–123 Copyright # Blackwell Munksgaard 2005 Blackwell Munksgaard. Printed in Denmark Journal of Cutaneous Pathology Abstracts of the Papers Presented at the 41st Annual Meeting of The American Society of Dermatopathology Westin Copley Place Boston, Massachusetts, USA October 14–17, 2004 These abstracts were presented in oral or poster format at the 41st Annual Meeting of The American Society of Dermatopathology on October 14–17, 2004. They are listed on the following pages in alphabetical order by the first author’s last name. 71 Abstracts IN SITU HYBRIDIZATION IS A VALUABLE DIAGNOSTIC A 37-year-old woman with diagnosis of Sjogren’s syndrome (SS) TOOL IN CUTANEOUS DEEP FUNGAL INFECTIONS presented with asymptomatic non-palpable purpura of the lower J.J. Abbott1, K.L. Hamacher2,A.G.Bridges2 and I. Ahmed1,2 extremities. Biopsy of a purpuric macule revealed a perivascular Departments of Laboratory Medicine and Pathology1 and and focally nodular lymphocytic infiltrate with large numbers of Dermatology2, plasma cells, seemingly around eccrine glands. There was no vascu- litis. The histologic findings in the skin were strikingly similar to those Mayo Clinic and Mayo Foundation, Rochester, MN, USA of salivary, parotid, and other ‘‘secretory’’ glands affected in SS. The cutaneous manifestations of SS highlighted in textbooks include Dimorphic fungal infections (histoplasmosis, blastomycosis, coccidiomy- xerosis, annular erythema, small-vessel vasculitis, and pigmented cosis, and cryptococcosis) can occur in immunocompromised and purpura. This case illustrates that purpura in skin of patients with healthy individuals. Cutaneous involvement is often secondary and SS may be caused by a peri-eccrine plasma-rich infiltrate. -

Itch in Ethnic Populations
Acta Derm Venereol 2010; 90: 227–234 REVIEW ARTICLE Itch in Ethnic Populations Hong Liang TEY1 and Gil YOSIPOVITCH2 1National Skin Centre, 1, Mandalay Road, Singapore, Singapore, and 2Department of Dermatology, Neurobiology & Anatomy, and Regenerative Medicine, Wake Forest University Health Sciences, Winston-Salem, NC, USA Racial and ethnic differences in the prevalence and clini- DIFFERENCES IN SKIN BIOLOGY AND ITCH cal characteristics of itch have rarely been studied. The aim of this review is to highlight possible associations Few studies have examined the differences between between ethnicity and different forms of chronic itch. We skin types in relation to ethnicity and neurobiology of provide a current review of the prevalence of different the skin. Differences between ethnic skin types and types of itch in ethnic populations. Genetic variation may skin properties may explain racial disparities seen in significantly affect receptors for itch as well as response pruritic dermatologic disorders. to anti-pruritic therapies. Primary cutaneous amyloido- sis, a type of pruritic dermatosis, is particularly common Epidermal structure and function in Asians and rare in Caucasians and African Ameri- cans, and this may relate to a genetic polymorphism in A recent study has shown that the skin surface and the Interleukin-31 receptor. Pruritus secondary to the melanocyte cytosol of darkly pigmented skin is more use of chloroquine for malaria is a common problem for acidic compared with those of type I–III skin (1). Serine African patients, but is not commonly reported in other protease enzymes, which have significant roles as pruri- ethnic groups. In patients with primary biliary cirrho- togens in atopic eczema and other chronic skin diseases, sis, pruritus is more common and more severe in African have been shown to be significantly reduced in black Americans and Hispanics compared with Caucasians. -

Extrafacial Granuloma Faciale
Journal of the American Osteopathic College of Dermatology Volume 11, Number 1 SPONSORS: ',/"!,0!4(/,/'9,!"/2!4/29s-%$)#)3 July 2008 34)%&%,,!"/2!4/2)%3s'!,$%2-! www.aocd.org Journal of the American Osteopathic College of Dermatology Journal of the American Osteopathic College of Dermatology 2007-2008 Officers President: Jay Gottlieb, DO President Elect: Donald Tillman, DO First Vice President: Marc Epstein, DO Second Vice President: Leslie Kramer, DO Third Vice President: Bradley Glick, DO Secretary-Treasurer: Jere Mammino, DO (2007-2010) Immediate Past President: Bill Way, DO Trustees: James Towry, DO (2006-2008) Mark Kuriata, DO (2007-2010) Karen Neubauer, DO (2006-2008) David Grice, DO (2007-2010) Sponsors: Global Pathology Laboratory Editors Stiefel Laboratories Jay S. Gottlieb, D.O., F.O.C.O.O. Medicis Stanley E. Skopit, D.O., F.A.O.C.D. James Q. Del Rosso, D.O., F.A.O.C.D. Galderma Editorial Review Board Ronald Miller, D.O. JAOCD Eugene Conte, D.O. Founding Sponsor Evangelos Poulos, M.D. Stephen Purcell, D.O. Darrel Rigel, M.D. !/#$s%)LLINOISs+IRKSVILLE -/ s&!8 Robert Schwarze, D.O. WWWAOCDORG Andrew Hanly, M.D. #/092)'(4!.$0%2-)33)/.WRITTENPERMISSIONMUSTBEOBTAINED Michael Scott, D.O. FROMTHE*OURNALOFTHE!MERICAN/STEOPATHIC#OLLEGEOF$ERMATOLOGY FORCOPYINGORREPRINTINGTEXTOFMORETHANHALFPAGE TABLESORlGURES Cindy Hoffman, D.O. 0ERMISSIONSARENORMALLYGRANTEDCONTINGENTUPONSIMILARPERMISSION Charles Hughes, D.O. FROMTHEAUTHORS INCLUSIONOFACKNOWLEDGEMENTOFTHEORIGINALSOURCE ANDAPAYMENTOFPERPAGE TABLEORlGUREOFREPRODUCEDMATERIAL Bill Way, D.O. 0ERMISSIONFEESAREWAIVEDFORAUTHORSWISHINGTOREPRODUCETHEIROWN Daniel Hurd, D.O. ARTICLES2EQUESTFORPERMISSIONSHOULDBEDIRECTEDTO*!/#$CO!/#$ 0/"OX+IRKSVILLE -/ Mark Lebwohl, M.D. #OPYRIGHTBYTHE*OURNALOFTHE!MERICAN/STEOPATHIC#OLLEGEOF Edward Yob, D.O. $ERMATOLOGY Jere Mammino, D.O. Printed by: Stoyles Graphics Services, Mason City, IA 50401 Schield M. -

Classic Diseases Revisited Yellow Nail Syndrome
Postgrad Med Jr 1997; 73: 466- 468 -I>, The Fellowship of Postgraduate Medicine, 1997 Classic diseases revisited Postgrad Med J: first published as 10.1136/pgmj.73.862.466 on 1 August 1997. Downloaded from Yellow nail syndrome Alon Hershko, Boaz Hirshberg, Menachem Nahir, Gideon Friedman Summary Yellow nail syndrome was first described by Samman and White' in 1964. The yellow nail syndrome was Their original article summarised a series of 13 patients and referred to several defined as a clinical entity in the other reports from 1927 and the early 1960s (box 1). Most of their patients 1960s. Although nail abnormal- suffered from ankle oedema and had slow rates of nail growth, ie, less than ities were the first sign to be 0.2 mm per week compared to the normal 0.5 - 1.2 mm per week. Samman and noticed, this syndrome is now White were also the first to suggest that an abnormality of lymphatic vessels may known to involve multiple organ explain the pathogenesis of the syndrome. Two years later Emerson described systems and its association with the full triad of slow-growing yellow nails, lymphoedema, and pleural other diseases is weil described. A effusions,2 while in 1972 Hiller et al reported that the presence of two of the review of the medical literature is three symptoms was sufficient to establish the diagnosis.3 Over the years the provided. features of yellow nail syndrome have been extensively studied, with special emphasis on the involvement ofthe respiratory tract which is the site of the most Keywords: yellow nail syndrome distressing symptoms. -

Primary Follicular Mucinosis
International Journal of Scientific & Engineering Research Volume 8, Issue 6, June-2017 1303 ISSN 2229-5518 Case Report Primary Follicular Mucinosis: A Case Report From Saudi Arabia With Successful Treatment And Literature Review SalaimanAlsaiari1 AwadhAlAmri2 AmerAlmuqati Ibrahim Allihibi ABSTRACT: Background:Follicular mucinosis is an uncommon inflammatory disorder that characteristically presents as clearly defined, erythematous plaques or papules, with follicular projections, superficial scaling, and alopecia in terminal hair bearing areas, characterized histologically by mucin accumulation in pilosebaceous units (follicular epithelium and sebaceous glands) . The condition is generally divided into primary (idiopathic) and secondary forms in association with several conditions including benign and malignant diseases. There are many local and systemic treatments. Main observations: We report a case of 15 years old male with primary follicular mucinosis treated effectively by intralesional steroid injections. Conclusions: This is a new case of Primary follicular mucinosis from Saudi Arabia was treated successfully with intralesional corticosteroids without relapse. KEYWORDS:follicular mucinosis, intralesional corticosteroids, treatment. —————————— —————————— INTRODUCTIONIJSER Follicular mucinosis is a rare condition, of unknown cause, which affects all races, ages and both sexes.1,2It is defined as the accumulation of mucin in the follicular epithelium and sebaceous glands.3,5 It was initially described in 1957 by Pinkus who named it -

Dermatology Volume 58 Issue 2 March-April 2013 Indian Journal Of
Indian Journal of ISSN: 0019-5154 Dermatology Volume 58 Issue 2 March-April 2013 Indian Journal of Highlights of the issue Dermatology • Update on cutaneous calciphylaxis • Macrophage migration inhibitory factor in • V Dermatology olume • Fixed duration therapy in leprosy 58 • Issue • Environmental dermatoses in Ladakh • Demodex folliculorum as a risk factor in 2 • Diagnosing rosacea March-April • Annular lesions in Dermatology 2013 • Pages Clinical and photomicrograph of Mycosis fungoides, PET-CT for staging and response assessment IJD® Symposium: Integrative Dermatology 87-**** Guest Editor: S R Narahari IJD® www.e-ijd.org E‑Case Report Angiolymphoid Hyperplasia with Eosinophilia with Follicular Mucinosis Rameshwar Gutte, Bhavana Doshi, Uday Khopkar From the Department of Dermatology, Seth G. S. Medical College and King Edward Memorial Hospital, Mumbai, India Abstract Follicular mucinosis occurring along with angiolymphoid hyperplasia with eosinophils (ALHE) has been described in a 49-year-old male. The patient presented with pruritic hyperpigmented papules and nodules on the vertex and right parietal scalp. There was no any other complaint. Histopathological examination from one of the papule showed prominent blood vessels in the dermis lined by plump histiocytoid endothelial cells that were surrounded by a dense lymphoid infiltrate with numerous eosinophils; these findings are typical of angiolymphoid hyperplasia with eosinophilia. Features of follicular mucinosis were observed in the same section with 3 hyperplastic follicular infundibula containing pools of mucin in the infundibular epithelium. The concurrent occurrence of these 2 distinct histopathological patterns in the same biopsy specimen has been reported rarely. Key Words: Angiolymphoid hyperplasia, eosinophilia, follicular mucinosis, scalp What was known? perivascular area and other parts of the dermis. -

This PDF Is Available for Free Download from a Site Hosted by Medknow Publications (
View Point Prurigo pigmentosa: An underdiagnosed disease? A. Böer, M. Asgari* Department of Dermatology and Dermatopathology, Dermatologikum, Hamburg, Germany, *Department of Pathology, Razi Center of Skin Lesions, Tehran University of Medical Sciences, Tehran, Iran. Address for correspondence: Dr. Almut Böer, Dermatologikum Hamburg, Stephansplatz 5, 20354, Hamburg, Germany. E-mail: [email protected] ABSTRACT Prurigo pigmentosa is a distinctive inflammatory disease first described by the Japanese dermatologist Masaji Nagashima in 1971. It is typified by recurrent, pruritic erythematous macules, papules and papulovesicles that resolve leaving behind netlike pigmentation. The disease is rarely diagnosed outside Japan, because clinicians outside Japan are not well conversant with the criteria for its diagnosis. Only one patient from India has been published previously under the diagnosis of prurigo pigmentosa, a hint that the disease may be under-recognized in India. We present an account of our observations in patients diagnosed with prurigo pigmentosa who were of five different nationalities, namely, Japanese, German, Indonesian, Turkish and Iranian. With this article we seek to increase awareness for the condition among dermatologists in India and we provide criteria for its diagnosis, both clinically and histopathologically. .com). Key Words: India, Pigmentation, Pruritic exanthema, Prurigo pigmentosa, Reticulate hyperpigmentation INTRODUCTION patient who presented with recurrent episodes of .medknowreticulate papular rash that resolved -

Acne Keloidalis Nuchae
Dermatologic Therapy, Vol. 20, 2007, 128–132 Copyright © Blackwell Publishing, Inc., 2007 Printed in the United States · All rights reserved DERMATOLOGIC THERAPY ISSN 1396-0296 Blackwell Publishing Inc Acne keloidalis nuchae Acne keloidalis nuchae, also known as folliculitis its antimicrobial and antiinflammatory effect), nuchae, is a chronic scarring folliculitis charac- and a series of intralesional steroids (40 mg/cc of terized by fibrotic papules and nodules of the existing keloids). Education is the key to preven- nape of the neck and the occiput. It particularly tion. I discourage high-collared shirts, short hair- affects young men of African descent and rarely cuts, and close shaving or cutting the hair along occurs in women; in either case its occurrence the posterior hairline. In the long-term, patients has a significant impact on the patient’s quality benefit from laser hair removal using diode or of life. We’ve asked our experts to share their expe- Nd:YAG, which helps avoid disease progression. rience in helping patients with this cosmetically Early treatment decreases the morbidity that can disfiguring disorder. be associated with late-stage disease. Question Dr. Vause: I treat early acne keloidalis nuchae by instructing patients to wash the skin frequently Please describe your approach to the treatment of with a mild keratolytic like tar or an alpha hydroxy patients with early (less than 20 papules, pustules acid cleanser. Patients are instructed to apply and 1–2 < 2 cm nuchae keloids) acne keloidalis topical clindamycin with steroid in the morning nuchae. (1–3) and retinoid at bedtime. Dr. Brauner: An option is to treat all patients with Response chlorhexadine cleanser as a daily shampoo and minocycline 100 mg daily b.i.d. -

Alopecia, Particularly: Alopecia Areata Androgenetic Alopecia Telogen Effluvium Anagen Effluvium
432 Teams Dermatology Hair disorders Color Code: Original, Team’s note, Important, Doctor’s note, Not important, Old teamwork Done by: Shaikha Aldossari Reviewer: Lama AlTawil 8 Team Leader: Basil Al Suwaine&Lama Al Tawil 432 Dermatology Team Lecture 8: Hair Disorders Objectives 1- Normal anatomy of hair follicle and hair cycle. 2- Causes, features and management of non scarring alopecia, particularly: Alopecia areata Androgenetic alopecia Telogen effluvium Anagen effluvium 3- Causes and features of scarring alopecia. 4- Causes and features of Excessive hair growth. hair disorder Excessive hair Alopecia growth non scarring Hirsutism Hypertrichosis scarring Anagen Telogen Androgenetic Alopecia effluvium effluvium Alopecia Areata P a g e | 1 432 Dermatology Team Lecture 8: Hair Disorders Anatomy of hair follicle: The Arrector piliResponsible for piloerection (goose bumps ) that happens when one is cold (produces energy and therefor warmth) . hair follicle becomes vertical instead of oblique Cuticle is the last layer here . what we can see outside . it has 7 layers of keratinocytes How many hairs in the body? 5 millions hairs in the body, 100,000 in the scalp. Growth rate: 0.3mm/day for scalp hair i.e.1cm/month Hair follicle bulge: -Very important part since it has stem cells .its the inertion of the arrector pili Hair follicle on vertical section: -So any pathological process affecting any part other Initially the shaft and the follicle are one than this, hair would still be able to regrow. organ then when you reach 1/3 the follicle -If we want to destroy a hair follicle, we’d target the bulge. -

The Tamilnadu Dr. M.G.R. Medical University Chennai, Tamil Nadu
CLINICO-PATHOLOGICAL STUDY OF SKIN SURFACE EPIDERMAL AND APPENDAGEAL TUMOURS Dissertation Submitted in partial fulfillment of university regulations for M.D. DEGREE IN DERMATOLOGY, VENEREOLOGY AND LEPROSY BRANCH XII – A THE TAMILNADU DR. M.G.R. MEDICAL UNIVERSITY CHENNAI, TAMIL NADU SEPTEMBER 2006 CERTIFICATE This is to certify that this Dissertation entitled “CLINICO-PATHOLOGICAL STUDY OF SKIN SURFACE EPIDERMAL AND APPENDAGEAL TUMOURS” is a bonafide work done by DR.G.BALAJI, Postgraduate student of Department of Dermatology, Leprosy and Institute of STD, Madras Medical College and Government General Hospital, Chennai – 3 for the award of Degree of M.D.( Dermatology, Venereology and Leprosy ) Branch XII – A during the academic year of 2003-2006. This work has not previously formed in the basis for the award of any degree or diploma. Prof. Dr. B. Parveen, MD., DD., Professor & Head, Dept. of Dermatology and Leprosy, Madras Medical College & Govt. General Hospital, Chennai – 3. Prof. Dr. Kalavathy Ponniraivan, MD., The Dean Madras Medical College & Govt. General Hospital, Chennai – 3. SPECIAL ACKNOWLEDGEMENT I sincerely thank Prof. Dr. Kalavathy Ponniraivan, MD., Dean, Madras Medical College & Govt. General Hospital, Chennai – 3, for granting me permission to use the resources of this institution for my study. ACKNOWLEDGEMENT I sincerely thank Prof. B.Parveen MD.,DD, Professor and Head of Department of Dermatology for her invaluable guidance and encouragement for the successful completion of this study. I express my heart felt gratitude to Dr.N.Gomathy MD.,DD, former Head of department of Dermatology who was instrumental in the initiation of this project, giving constant guidance throughout my work.