Ganirelix Acetate Injection for SUBCUTANEOUS USE ONLY
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ganirelix) May Prevent Ovarian Hyperstimulation Syndrome Caused by Ovarian Stimulation for In-Vitro Fertilization
Human Reproduction vol.13 no.3 pp.573–575, 1998 CASE REPORT High dose gonadotrophin-releasing hormone antagonist (ganirelix) may prevent ovarian hyperstimulation syndrome caused by ovarian stimulation for in-vitro fertilization D.de Jong1, N.S.Macklon1, B.M.J.L.Mannaerts2, releasing hormone (GnRH) agonists in order to prevent H.J.T.Coelingh Bennink2 and B.C.J.M.Fauser1,3 unpredictable changes in release of endogenous gonadotrophins. However, it has been reported that the continued administration 1Division of Reproductive Medicine, Department of Obstetrics and Gynaecology, Dijkzigt Academic Hospital and Erasmus University of GnRH agonists does not affect subsequent ovarian quiescence Medical School, Dr. Molewaterplein 40, 3015 GD, Rotterdam and (Wadaet al., 1992). This may be related to prolonged suppression 2Scientific Development Group, NV Organon, Oss, The Netherlands of pituitary function due to slow recovery from down-regulation 3To whom correspondence should be addressed (Donderwinkel et al., 1993). Some residual gonadotrophin release may remain during GnRH agonist suppression, whereas This case report describes the first attempt to treat pituitary release of LH and follicle-stimulating hormone (FSH) imminent ovarian hyperstimulation syndrome (OHSS) by may be virtually abolished with the sustained use of a high dose using a gonadotrophin-releasing hormone (GnRH) of GnRH antagonist. In this case report we describe an alternative antagonist. A 33 year old, normo-ovulatory woman under- method, using a high dose of a GnRH antagonist which may going in-vitro fertilization received daily subcutaneous decrease the risk of a severe OHSS. injections of 150 IU of recombinant follicle-stimulating hormone (recFSH) from cycle day 2, together with GnRH antagonist (ganirelix) 0.125 mg from cycle day 7 onwards. -

Letter Without Tagline
CH D Press release DONGBAO TO ACQUIRE FERRING’S MALMÖ MANUFACTURING OPERATION Saint Prex, Switzerland and Shanghai, China, Friday 17 November, 2006 – Ferring Pharmaceuticals and Shanghai Dongbao Biopharmaceutical Company announced today the signing of an agreement by which Dongbao Biopharmaceutical will purchase Ferring’s manufacturing operation at Malmö in Sweden. Earlier this year, Ferring informed staff of its plan to cease manufacturing at Malmö by the end of March 2008. However, the acquisition by Dongbao Biopharmaceutical has secured the jobs of around 50 members of staff. The agreement will become effective on 1 January, 2007. “From the very beginning, our aim has been to find a solution which would maintain the Malmö production site,” commented Ferring Pharmaceuticals Chief Operating Officer, Michel Pettigrew. “This agreement is a boost for the local community and has secured the long-term future of the factory for around 50 employees, whose experience will be invaluable to Dongbao Biopharmaceutical.” “We see great potential for the manufacturing centre at Malmö,” added Dr George Li, President of Dongbao Biopharmaceutical. “The site is technically very developed and the current team, who will be an important part of our future business development, offer a lot of knowledge and competencies.” Ends Ferring International Center S.A., Chemin de la Vergognausaz 50, 1162 Saint‐Prex, Switzerland Tel: +41 58 301 00 00, Fax: +41 58 301 00 10, www.ferring.com CH About Ferring: Ferring is a Swiss-based research driven, speciality biopharmaceutical group active in global markets. The company identifies, develops and markets innovative products in the areas of endocrinology, gastroenterology, gynaecology, fertility and urology. -

Fertility Medications: Bravelle®, Cetrotide®, Clomid, Clomiphene, Follistim AQ®, Ganirelix®, Gonal-F®, Human Chorionic Gonadotropin, Leuprolide
Drug Therapy Guidelines Fertility Medications: Bravelle®, Cetrotide®, Clomid, clomiphene, Follistim AQ®, Ganirelix®, Gonal-F®, human chorionic gonadotropin, leuprolide, Menopur®, Novarel®, Ovidrel®, Pregnyl®, Crinone®, Applicable* Endometrin®, First-Progesterone®, progesterone in oil Medical Benefit x Effective: 08/03/2021 Pharmacy- Formulary 1 x Next Review: 6/22 Pharmacy- Formulary 2 x Date of Origin: 7/00 Pharmacy- Formulary 3/Exclusive x Review Dates: 7/12/00, 5/8/01, 1/15/02, 5/6/03, 12/16/03, 6/8/04, Pharmacy- Formulary 4/AON x 12/16/05, 2/1/06, 10/15/06, 7/20/07, 11/5/07, 12/15/08, 12/09, 9/10, 1/11, 9/11, 9/12, 9/13, 9/14, 6/15, 6/16, 6/17, 6/18, 6/19, 9/19, 3/20, 6/20, 9/20, 3/21, 6/21 I. Medication Description Gonadotropin Releasing Hormone (GnRH) Agonists are indicated for the inhibition of premature luteinizing hormone (LH) surges in women undergoing controlled ovarian stimulation. GnRH Antagonists are indicated for inhibition of premature luteinizing hormone (LH) surges in women undergoing controlled ovarian stimulation. Gonadotropins, FSH, or combination of FSH/LH are indicated for stimulation of ovarian follicular growth. Human chorionic gonadotropins (hCG) are indicated for inducing ovulation. Clomiphene is a selective-estrogen receptor-modulator (SERM) used for inducing ovulation. Therapeutic Class Agents GnRH Agonists leuprolide GnRH Antagonists Cetrotide®, Ganirelix® Gonadotropins Follitropin alfa: Gonal-F®, Gonal-F RFF® (non-preferred) Follitropin beta: Follistim AQ® (preferred) Menotropins: Menopur® Urofollitropins: Bravelle® hCG human chorionic gonadotropin, Novarel®, Ovidrel®, Pregnyl® Progestin Injection progesterone oil for injection Vaginal Progesterone Crinone, Endometrin, First-Progesterone Selective-estrogen receptor- Clomid*, Clomiphene* modulator (SERM) II. -

Triptorelin Pamoate (Subcutaneous Injection) for Prostate Cancer NIHRIO (HSRIC) ID: 20540 NICE ID: 9841
NIHR Innovation Observatory Evidence Briefing: May 2018 Triptorelin pamoate (subcutaneous injection) for prostate cancer NIHRIO (HSRIC) ID: 20540 NICE ID: 9841 LAY SUMMARY Prostate cancer is cancer of the prostate gland (a small organ in a man’s pelvis) and is the second most common cancer in the UK. There are three stages: localised, locally‐advanced and advanced (or metastatic) prostate cancer. The symptoms of prostate cancer may vary depending on the stage of cancer but can include pain, tiredness, problems emptying the bladder and the bowels. About half of men diagnosed with locally‐advanced prostate cancer will see their cancer spread to other body organs (i.e. becoming metastatic). Triptorelin is being developed as an injection under the skin (subcutaneous) for the treatment of locally advanced or metastatic prostate cancer. It is already marketed for this condition but is given by injection deep into the muscles (intramuscular). Triptorelin is an artificial analogue of natural gonadotropin‐releasing hormone that acts to slowly reduce the level of testosterone in the body. The first administration of triptorelin stimulates an increase in testosterone levels but prolonged administration leads to a fall in plasma testosterone or oestradiol to castrate levels which is maintained for as long as the product is administered. Triptorelin as a subcutaneous injection formulation has the potential advantage of improved safety and local tolerability when compared to intramuscular injection formulation. This briefing reflects the evidence available at the time of writing. A version of the briefing was sent to the company for a factual accuracy check. The company was available to provide comment. -

REKOVELLE®, the First Recombinant Follicle Stimulating Hormone Derived
REKOVELLE®, the first recombinant follicle stimulating hormone derived from a human cell line, is now available for Canadian women undergoing IVF and other assisted reproductive technologies REKOVELLE® helps women achieve a more predictable and targeted ovarian response Toronto, Ontario – 29 October 2018 – Ferring Pharmaceuticals announced that REKOVELLE® (follitropin delta injection), the first recombinant FSH for controlled ovarian stimulation derived from a human cell line, is now available in Canada for women undergoing assisted reproductive technologies such as in vitro fertilization (IVF).1 Ovarian response to stimulation varies considerably from woman to woman,2 and unexpected extreme responses have implications on efficacy and safety.3,4 REKOVELLE® is the first gonadotropin to use an evidence-based, personalized dosing algorithm based on a woman’s anti-Müllerian hormone (AMH) level and body weight to achieve a predictable ovarian response.1 “One in six Canadian couples experience infertility and many couples feel anxious about the unknowns of reproductive medicine when they go through IVF for the first time,” says Dr. Al Yuzpe, Reproductive Endocrinologist, Co-Founder and Co-Director of Olive Fertility Centre in Vancouver. “REKOVELLE® provides a more predictable and personalized option considering each woman’s AMH and body weight. We finally have an FSH preparation that is dosed based on scientific evidence, removing the subjective decision of choosing the appropriate dosage of FSH for each woman.” REKOVELLE® was approved by Health Canada on March 22, 2018, and is the first gonadotropin to be granted Innovative Drug status by Health Canada.5 “We are proud to lead the way towards a more innovative and personalized care approach for women undergoing IVF,” said Lee Ferreira, General Manager, Ferring Pharmaceuticals. -

Ferring Pharmaceuticals and Kyowa Kirin Announce Termination the License Agreement and the Supply and Co-Promotion Agreement Of
Ferring Pharmaceuticals and Kyowa Kirin Announce Termination the License Agreement and the Supply and Co-Promotion Agreement of Pharmaceutical Products of Desmopressin Tokyo, February 25, 2020 — Ferring Pharmaceuticals Co., Ltd. (Tokyo Japan; President and CEO: Mark Noggle, “Ferring”) and Kyowa Kirin Co., Ltd., (Tokyo Japan; President and CEO:Masashi Miyamoto, “Kyowa Kirin”) today announced that Kyowa Kirin transfers all marketing authorizations for the products of desmopressin*1 (generic name: Desmopressin Acetate Hydrate) to Ferring effective on and from April 27, 2020, and they terminate the license agreement and the supply and co-promotion agreement about these products of desmopressin and MINIRINMELT®OD Tablet (Desmopressin Acetate Hydrate Orally Disintegrating Tablet) on the same day. The seven products subjected to the termination are listed below. Ferring and Kyowa Kirin have co-promoted for the seven products and Kyowa Kirin has distributed them. Kyowa Kirin terminates to distribute the products on April 26,2020 upon termination of the license agreement. Product Listing Generic name Product name Main indication Supplier Distributor Desmopressin MINIRINMELT®OD Central diabetes Ferring Kyowa Kirin Acetate Tablet Insipidus*2 Pharmaceuticals Co., Ltd. Hydrate (60 ㎍/120 ㎍/240 ㎍) Co., Ltd. DESMOPRESSIN Central diabetes Kyowa Kirin Co., Intranasal 0.01% Insipidus Ltd. Kyowa DESMOPRESSIN・ Spray 2.5 Kyowa DESMOPRESSIN・ Nocturnal enuresis / *3 Spray 10 Kyowa bedwetting DESMOPRESSIN Hemophillia A Injection 4 Kyowa von Willebrand’s disease *1 About Desmopressin Desmopressin is a synthetic analog of antidiuretic hormone (vasopressin), an artificial peptide consisting of 8 amino acids. The drug has a strong antidiuretic action that concentrates the urine and decreases urine output. *2 About central diabetes insipidus Central diabetes insipidus is a disease caused by reduced or absent synthesis or secretion of antidiuretic hormone known as arginine vasopressin (AVP) that causes symptoms such as excessive urination as well as extreme thirst and increased fluid intake. -

Follicular and Endocrine Profiles Associated with Different Gnrh
Reproductive BioMedicine Online (2012) 24, 153– 162 www.sciencedirect.com www.rbmonline.com ARTICLE Follicular and endocrine profiles associated with different GnRH-antagonist regimens: a randomized controlled trial Juan Antonio Garcı´a-Velasco a, Sanja Kupesic b, Antonio Pellicer c, Claire Bourgain d, Carlos Simo´n e, Milan Mrazek f, Paul Devroey g, Joan-Carles Arce h,* a IVI Foundation, Reproductive Endocrinology, Madrid, Spain; b Texas Tech University Health Sciences Center, Department of Obstetrics and Gynecology, El Paso, TX, USA; c IVI Foundation, Reproductive Endocrinology, Valencia, Spain; d UZ Brussel, Department of Pathology, Brussels, Belgium; e IVI Foundation, Research Department, Valencia, Spain; f ISCARE IVF a.s., Lighthouse, Prague, Czech Republic; g UZ Brussel, Centre for Reproductive Medicine, Brussels, Belgium; h Reproductive Health, Global Clinical and Non-Clinical R & D, Ferring Pharmaceuticals, Copenhagen, Denmark * Corresponding author. E-mail address: [email protected] (J.-C. Arce). Dr Juan Garcı´a-Velasco did his training in obstetrics and gynaecology at Madrid Autonoma University, and then his reproductive endocrinology and infertility fellowship at Yale University, USA (1997–1998). He is now Director of IVI-Madrid and Associate Professor at Rey Juan Carlos University. He has published over 100 peer- reviewed articles. He is an ad-hoc reviewer for the main journals in the field and serves on the editorial board of Reproductive BioMedicine Online. His main research interests are endometriosis, ovarian hyperstimulation syndrome, low responders and human implantation. Abstract This trial assessed the impact of early initiation of gonadotrophin-releasing hormone (GnRH) antagonist on follicular and endocrine profiles compared with the fixed GnRH-antagonist protocol. -

Ganirelix Acetate) Injection
1 Antagonä (ganirelix acetate) Injection 2 FOR SUBCUTANEOUS USE ONLY 3 4 DESCRIPTION 5 Antagonä (ganirelix acetate) Injection is a synthetic decapeptide with high antagonistic 6 activity against naturally occurring gonadotropin-releasing hormone (GnRH). Ganirelix 7 acetate is derived from native GnRH with substitutions of amino acids at positions 1, 2, 3, 8 6, 8, and 10 to form the following molecular formula of the peptide: N-acetyl-3-(2- 9 naphthyl)-D-alanyl-4-chloro-D-phenylalanyl-3-(3-pyridyl)-D-alanyl-L-seryl-L-tyrosyl- 10 N9,N10-diethyl-D-homoarginyl-L-leucyl-N9,N10-diethyl-L-homoarginyl-L-prolyl-D- 11 alanylamide acetate. The molecular weight for ganirelix acetate is 1570.4 as an anhydrous 12 free base. The structural formula is as follows: 13 Ganirelix acetate 14 15 16 17 18 19 + x C2H4O2 + y H2O 20 21 Antagonä is supplied as a colorless, sterile, ready-to-use, aqueous solution intended for 22 SUBCUTANEOUS administration only. Each sterile, pre-filled syringe contains 250 Ganirelix PI 1 23 mg/0.5 mL of ganirelix acetate, 0.1 mg glacial acetic acid, 23.5 mg mannitol, and water for 24 injection adjusted to pH 5.0 with acetic acid, NF and/or sodium hydroxide, NF. 25 CLINICAL PHARMACOLOGY 26 The pulsatile release of GnRH stimulates the synthesis and secretion of luteinizing 27 hormone (LH) and follicle-stimulating hormone (FSH). The frequency of LH pulses in 28 the mid and late follicular phase is approximately 1 pulse per hour. These pulses can be 29 detected as transient rises in serum LH. -

Tractocile, Atosiban
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Tractocile 6.75 mg/0.9 ml solution for injection 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each vial of 0.9 ml solution contains 6.75 mg atosiban (as acetate). For a full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection (injection). Clear, colourless solution without particles. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Tractocile is indicated to delay imminent pre-term birth in pregnant adult women with: regular uterine contractions of at least 30 seconds duration at a rate of 4 per 30 minutes a cervical dilation of 1 to 3 cm (0-3 for nulliparas) and effacement of 50% a gestational age from 24 until 33 completed weeks a normal foetal heart rate 4.2 Posology and method of administration Posology Treatment with Tractocile should be initiated and maintained by a physician experienced in the treatment of pre-term labour. Tractocile is administered intravenously in three successive stages: an initial bolus dose (6.75 mg), performed with Tractocile 6.75 mg/0.9 ml solution for injection, immediately followed by a continuous high dose infusion (loading infusion 300 micrograms/min) of Tractocile 37.5 mg/5 ml concentrate for solution for infusion during three hours, followed by a lower dose of Tractocile 37.5 mg/5 ml concentrate for solution for infusion (subsequent infusion 100 micrograms/min) up to 45 hours. The duration of the treatment should not exceed 48 hours. The total dose given during a full course of Tractocile therapy should preferably not exceed 330.75 mg of atosiban. -

Antagonists in Poor-Responder Patients
FERTILITY AND STERILITY VOL. 80, SUPPL. 1, JULY 2003 Copyright ©2003 American Society for Reproductive Medicine Published by Elsevier Inc. Printed on acid-free paper in U.S.A. Antagonists in poor-responder patients Alan B. Copperman, M.D. Mount Sinai School of Medicine, New York, New York Objective: To review treatment options for poor-responding patients who are undergoing infertility treatment. Design: Review article and case studies. Results: A comprehensive determination of potential ovarian response for the poor-responding patient is important in the individualization of treatment options for these patients. Treatment options include both the microdose flare leuprolide acetate and GnRH antagonist stimulation protocols. For GnRH antagonist stimu- lation protocols, individualization of treatment includes use of oral contraceptive pretreatment and alterations in duration of gonadotropin stimulation and start day of antagonist administration. Conclusions: For poor-responding patients, the benefits of using GnRH antagonists for the suppression of premature LH surges plus the determination that stimulation protocols that include GnRH antagonists are at least as good as the microdose flare and provide better cycle outcomes than the long luteal leuprolide acetate down-regulation protocols have the potential to bring changes to the existing protocols for ovarian stimulation. (Fertil Steril 2003;80(Suppl 1):S16–24. ©2003 by American Society for Reproductive Medicine.) Key Words: Ganirelix, GnRH antagonist, poor ovarian response, treatment options Individualization of stimulation regimens, ment modalities in COH, it is also important to prospective analysis of ovarian reserve, and have a clear understanding of inclusion criteria setting defined goals regarding ovarian re- for the poor-responder patient. -

Ganirelix Acetate Injection, Solution Organon USA Inc
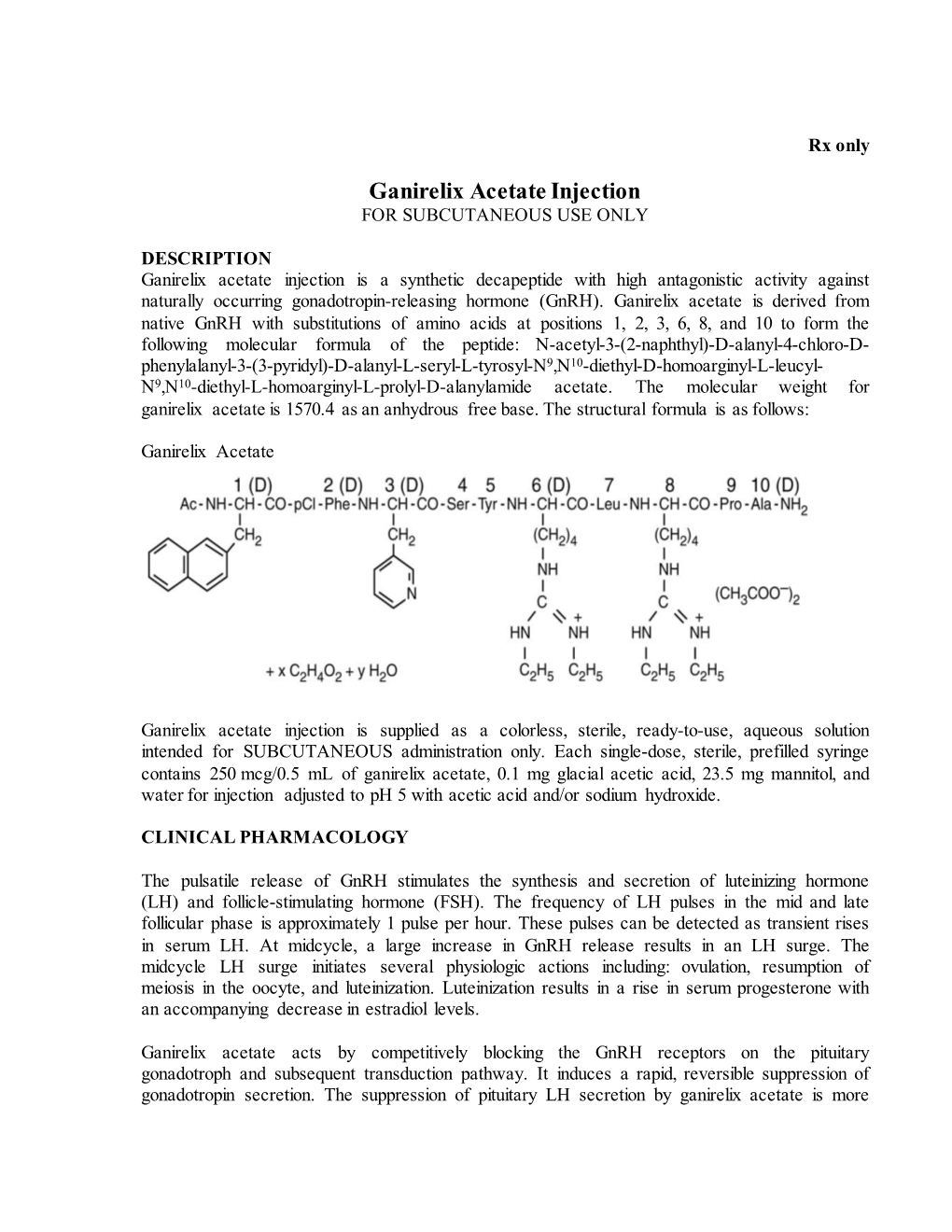
GANIRELIX ACETATE- ganirelix acetate injection, solution Organon USA Inc. ---------- Ganirelix Acetate Injection FOR SUBCUTANEOUS USE ONLY DESCRIPTION Ganirelix Acetate Injection is a synthetic decapeptide with high antagonistic activity against naturally occurring gonadotropin-releasing hormone (GnRH). Ganirelix Acetate is derived from native GnRH with substitutions of amino acids at positions 1, 2, 3, 6, 8, and 10 to form the following molecular formula of the peptide: N-acetyl-3-(2-naphthyl)-D-alanyl-4-chloro-D-phenylalanyl-3-(3-pyridyl)-D- alanyl-L-seryl-L-tyrosyl-N9,N10-diethyl-D-homoarginyl-L-leucyl-N9,N10-diethyl-L-homoarginyl-L- prolyl-D-alanylamide acetate. The molecular weight for Ganirelix Acetate is 1570.4 as an anhydrous free base. The structural formula is as follows: Ganirelix Acetate Ganirelix Acetate Injection is supplied as a colorless, sterile, ready-to-use, aqueous solution intended for SUBCUTANEOUS administration only. Each single dose, sterile, prefilled syringe contains 250 mcg/0.5 mL of Ganirelix Acetate, 0.1 mg glacial acetic acid, 23.5 mg mannitol, and water for injection adjusted to pH 5.0 with acetic acid, NF and/or sodium hydroxide, NF. CLINICAL PHARMACOLOGY The pulsatile release of GnRH stimulates the synthesis and secretion of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). The frequency of LH pulses in the mid and late follicular phase is approximately 1 pulse per hour. These pulses can be detected as transient rises in serum LH. At midcycle, a large increase in GnRH release results in an LH surge. The midcycle LH surge initiates several physiologic actions including: ovulation, resumption of meiosis in the oocyte, and luteinization. -

201110Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 201110Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRISK) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type NDA Application Number 201110 PDUFA Goal Date April 29, 2020 OSE RCM # 2016-789 Reviewer Name(s) Theresa Ng, PharmD, BCPS, CDE Team Leader Laura Zendel, PharmD, BCPS Division Director Jamie Wilkins, PharmD Review Completion Date April 29, 2020 Subject Evaluation of Need for a REMS Established Name Progesterone Vaginal (b) (4) Trade Name Milprosa Name of Applicant Ferring Pharmaceuticals Inc. (Ferring) Therapeutic Class Progesterone Formulation(s) (b) (4) progesterone in a non-biodegradable, (b) (4) vaginal Ring containing (b) (4) gram progesterone releasing an average of 11 mg/day of progesterone over a 7-days. Dosing Regimen One ring inserted vaginally (b) (4) the day after oocyte retrieval. The vaginal ring is replaced weekly, continuing for up to 10 weeks total duration. 1 Reference ID: 45999664601440 Table of Contents EXECUTIVE SUMMARY ......................................................................................................................................................... 3 1 Introduction ..................................................................................................................................................................... 3 2 Background .....................................................................................................................................................................