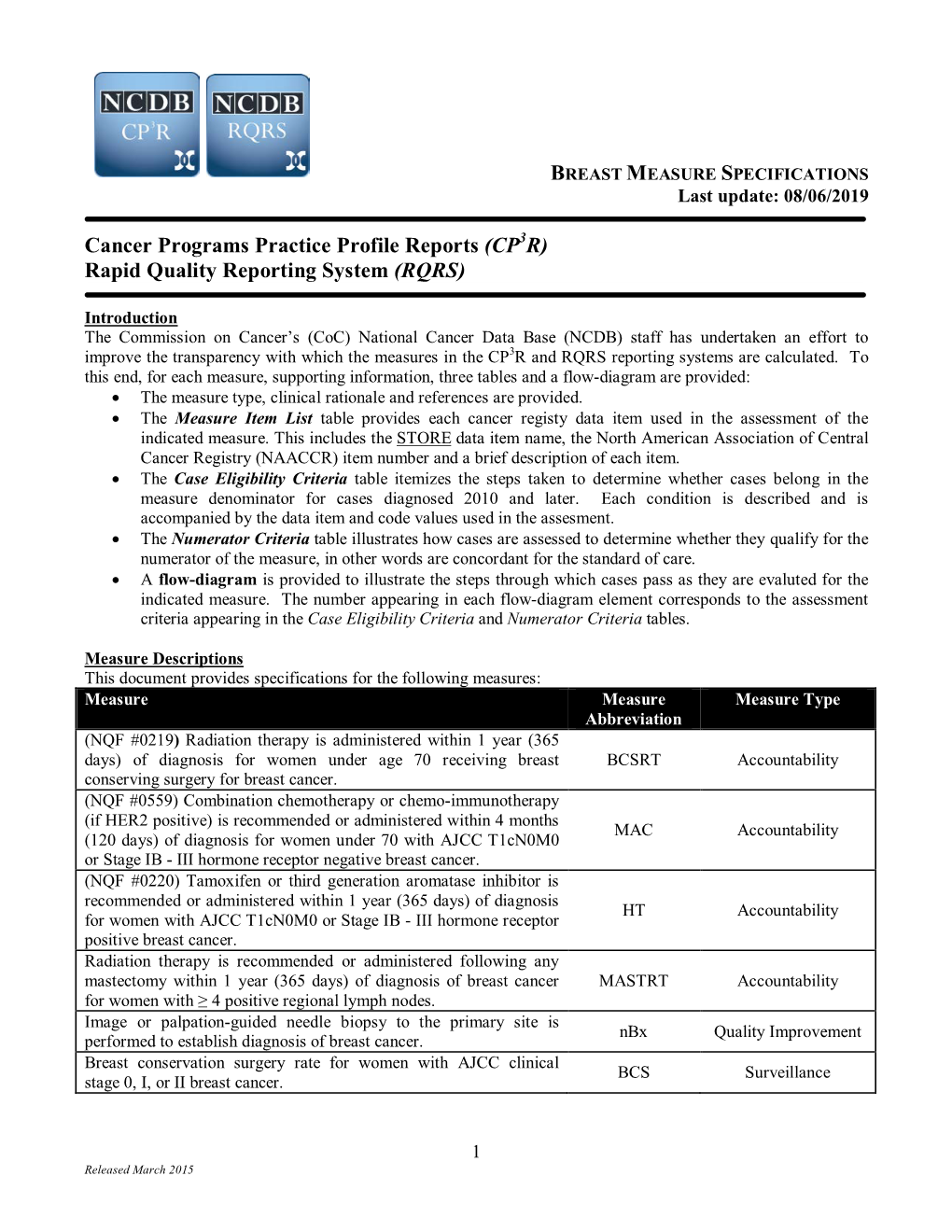
BREAST MEASURE SPECIFICATIONS Last Update: 08/06/2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Breast Cancer Screening HEDIS Tip Sheet
HEDIS® Tip Sheet Effectiveness of Care Measure Breast Cancer Screening Breast cancer is the most common type of cancer, and the second leading cause of cancer-related deaths among women in the United States. Approximately 237,000 cases of breast cancer are diagnosed in women, and about 41,000 women die each year of breast cancer.1 Mammography is an effective screening tool for early detection of breast cancer and reduction of breast cancer mortality. California Health & Wellness want to help your practice increase Healthcare Effectiveness Data and Information Set (HEDIS®) rates. This tip sheet outlines key details of the Breast Cancer Screening (BCS) measure, its codes and guidance for documentation. Measure Women ages 50–74 who had a mammogram to screen for breast cancer in the past two years.2 Exclusions: • Patients who meet the following – A unilateral mastectomy criteria anytime during the without a modifier and measurement year: a left mastectomy with – Medicare patients ages 66 and service dates 14 days or older enrolled in an institutional more apart. special needs plans (I-SNP) or – A unilateral mastectomy living long-term in an institution. without a modifier and a – Patients ages 66 and older with right mastectomy with service frailty and advanced illness. dates 14 days or more apart. – Patients in hospice. – Absence of the left breast and absence of the right breast on the • Patients with bilateral mastectomy. same or different dates of service. Any of the following meet the criteria – Both of the following (on the same for bilateral mastectomy: or different dates of service): – Bilateral mastectomy or history. -

Breast Reconstruction with Expanders and Implants
Evidence-Based Clinical Practice Guideline: Breast Reconstruction with Expanders and Implants INTRODUCTION Disclaimer Evidence-based guidelines are strategies for patient management, The American Cancer Society estimates that nearly 230,000 American developed to assist physicians in clinical decision making. This women were diagnosed with invasive breast cancer in 2011.1 Many of guideline was developed through a comprehensive review of the these individuals will require mastectomy and total reconstruction of scientific literature and consideration of relevant clinical experience, the breast. The diagnosis and subsequent process can create signifi- and describes a range of generally acceptable approaches to diagnosis, cant confusion and distress for the affected persons and their families management, or prevention of specific diseases or conditions. This and, consequently, surgical treatment and reconstructive procedures guideline attempts to define principles of practice that should are of utmost importance in the breast cancer care continuum. In generally meet the needs of most patients in most circumstances. 2011, the American Society of Plastic Surgeons® (ASPS) reported an increase in the rate of breast reconstructions, citing nearly 100,000 However, this guideline should not be construed as a rule, nor procedures, of which the majority employed expanders/implants.2 should it be deemed inclusive of all proper methods of care The 3% increase in reconstructions over the course of just one year or exclusive of other methods of care reasonably directed at highlights the significance of maintaining patient safety and obtaining the appropriate results. It is anticipated that it will be optimizing surgical outcomes. necessary to approach some patients’ needs in different ways. -

Procedure: Mastectomy Instructions Surgery Information: 1
Procedure: Mastectomy Instructions Surgery Information: 1. Please stop all vitamins, supplements, and herbal medications one week before surgery, your surgeon will review any other medications that need to be stopped before surgery 2. Surgery will take about 2.5 hours 3. Surgery will be at Aspirus Wausau Hospital 4. You will have General Anesthesia 5. You will likely go home 24 hours after your surgery, but may stay longer if needed 6. If you are sensitive to tape, please tell your check-in nurse on your day of surgery 7. You will need an appointment with us about 1 week after your surgery for an incision check unless you had reconstruction (then your post-operative appt. will be with your Plastic Surgeon) Follow up appt:__________________ 8. We will call you typically within 3 business days with final pathology results 9. Please remember to wear the binder the you were given at all times (unless showering) until two weeks after your last drain is removed– the binder can be washed and hung to dry if needed. If your binder is itchy you can try wearing a T-shirt/tank top underneath or use an ACE wrap for gentle compression. AVOID more than slight pressure. Restrictions: 1. No lifting more than 15lbs. for 2 weeks after the last drain is removed 2. You will be given arm exercises by occupational therapy before you leave the hospital. It is important that you follow the instructions you are given 3. No pushing, pulling, or stretching overhead for 2 weeks after the last drain is removed. -

Breast Cancer: Management and Follow-Up
Breast Cancer: Management and Follow-Up Effective Date: October 1, 2013 Scope This guideline provides recommendations for management and follow-up of biopsy-proven breast cancer in women aged ≥ 19 years. For diagnostic recommendations, please refer to BCGuidelines.ca - Breast Disease & Cancer: Diagnosis. Refer to Appendix A for the algorithms associated with these guidelines. Key Recommendations • Immediately refer patient to the appropriate specialist by telephone, as soon as a tissue diagnosis of cancer is made. • Surveillance for an asymptomatic patient is recommended with a physical examination and annual diagnostic mammography. • A patient should report any symptoms of concern (e.g., new lumps, bone pain, chest pain, persistent headaches, dyspnea, or abdominal pain) immediately to their family physician and/or oncologist. • No routine laboratory tests are indicated in an asymptomatic patient for surveillance. Management Indications for Referral to Specialist Surgeon: As soon as a patient has a confirmed tissue diagnosis of a malignant or atypical proliferative breast lesion, immediately refer the patient to surgeon by telephone. Where possible, refer to a surgeon with experience or special interest in the breast. If a mastectomy is planned, the surgeon may refer the patient to a plastic surgeon to discuss reconstructive options pre-surgery. Oncologist*: Referral to an oncologist is typically done by the surgeon post-surgery unless the patient wants a discussion with an oncologist prior to making a decision about surgery. GP can also help facilitate this referral process if indicated. Additional Considerations for Referral Fertility Specialist: A discussion about fertility preservation with women who have invasive cancer that may require chemotherapy and would like to have children should occur soon after diagnosis. -

Clinical Guidelines for the Management of Breast Cancer West Midlands Expert Advisory Group for Breast Cancer West Midlands Clinical Networks and Clinical Senate
Clinical Guidelines for the Management of Breast Cancer West Midlands Expert Advisory Group for Breast Cancer West Midlands Clinical Networks and Clinical Senate Coversheet for Network Expert Advisory Group Agreed Documentation This sheet is to accompany all documentation agreed by the West Midlands Strategic Clinical Network Expert Advisory Groups. This will assist the Clinical Network to endorse the documentation and request implementation. EAG name Breast Cancer Expert Advisory Group Document Clinical guidelines for the management of breast cancer Title Published December 2016 date Document Clinical guidance for the management of Breast cancer to all practitioners, Purpose clinicians and health care professionals providing a service to all patients across the West Midlands Clinical Network. Authors Original Author: Mr Stephen Parker Modified By: Mrs Abigail Tomlins Consultant Breast Surgeon University Hospitals Coventry & Warwickshire NHS Trust References Consultation These guidelines were originally authored by Stephen Parker and Process subsequently modified by Abigail Tomlins for the Coventry, Warwickshire and Worcestershire Breast Group. The West Midlands EAG agreed to adopt these guidelines as the regional network guidelines. The version history reflects changes made by the Coventry, Warwickshire and Worcestershire Breast Group. As the Coventry, Warwickshire and Worcestershire Breast Group update their guidelines, the EAG will discuss whether to adopt the updated version. Review Date December 2019 (must be within three years) Approval Network Clinical Director Signatures: Date: 25/10/2017 \\ims.gov.uk\data\Users\GBEXPVD\EXPHOME25\PGoulding\Data\Desktop\guidelines- 2 for-the-management-of-breast-cancer-v1.doc Version History - Coventry, Warwickshire and Worcestershire Breast Group Version Date Brief Summary of Change 2010v1.0D 12 March 2010 Immediate breast reconstruction criteria Young adult survivors Updated follow-up guidelines. -

Lumpectomy/Mastectomy Patient/Family Education
LUMPECTOMY/MASTECTOMY PATIENT/FAMILY EDUCATION Being diagnosed with breast cancer can be emotionally challenging. It is important to learn as much as possible about your cancer and the available treatments. More than one type of treatment is commonly recommended for breast cancer. Each woman’s situation is unique and which treatment or treatments that will be recommended is based on tumor characteristics, stage of disease and patient preference. Surgery to remove the cancer is an effective way to control breast cancer. The purpose of this educational material is to: increase the patient’s and loved ones’ knowledge about lumpectomy and mastectomy to treat breast cancer; reduce anxiety about the surgery; prevent post-operative complications; and to facilitate physical and emotional adjustment after breast surgery. THE BASICS There are three primary goals of breast cancer surgery: 1. To remove a cancerous tumor or other abnormal area from the breast and enough surrounding breast tissue to leave a “margin of safety” around the tumor or affected area. 2. To remove lymph nodes from the armpit area (axilla) to check for possible spread of cancer (metastasis) or remove lymph nodes that are already known to contain cancer. 3. Sometimes one or both breasts are removed to prevent breast cancer if a woman is at especially high risk for the disease. Breast cancer surgery can be done before or after chemotherapy (if chemotherapy is recommended). Radiation therapy and hormonal therapy (if recommended) are typically done after surgery. There are several types of breast surgery. The type of surgery best suited for a specific woman depends on the type of breast disease, the size and location of the breast disease/tumor(s) in the breast, and the personal preference of the patient. -

Breast Self-Examination Practices in Women Who
Breast self-examination practices in women who have had a mastectomy by Carole H Crowell A thesis submitted in partial fulfillment of the requirement for the degree of Master of Nursing Montana State University © Copyright by Carole H Crowell (1990) Abstract: Research findings indicate that breast cancer mortality has not decreased significantly in the past decade. While research continues on the development of more effective therapies, techniques for early detection are presently receiving greater attention. The use of breast self-examination (BSE) has been emphasized in the media and professional literature but little emphasis has been placed on BSE for women who have had a mastectomy. The purposes of this study were to determine if women who have had breast surgery do breast self-examination and to describe barriers that block this behavior. An assumption was made that women who have had surgery for breast cancer do not examine their remaining breast tissue and scar site. A qualitative study was conducted using a grounded theory approach to explore and describe behavior of women who have had a mastectomy. Analytic strategies used for data analysis were the constant comparative method, theoretical sampling, open coding, memo writing, and recoding. A convenience sample of twelve informants was selected from a mastectomy support group located in a rural community in Montana. BSE was viewed as a health-promoting behavior and was found to relate to certain variables of Penders (1987) Health Promotion Model. Findings of this study indicate a majority of women perform BSE after their mastectomy but most do not examine their scar site. -

Lumpectomy and Mastectomy Surgery Comparison
Lumpectomy and Mastectomy Surgery Comparison Surgery to remove cancer from the breast can be done with either lumpectomy or mastectomy. Your surgeon will tell you if one option is better for you than the other. Or, you may be eligible for both and must decide which procedure to have. Survival rate (chance of being alive at a certain time point) is the same with both surgeries. For this reason, both surgical options are considered equal in the treatment of breast cancer. Lumpectomy Lumpectomy is the removal of the part of the breast that has cancer. Other names for this surgery are segmental and partial mastectomy. This surgery is for patients who have a small area of disease in relation to breast size. Lumpectomy must be followed by radiation to be considered appropriate treatment. Radiation usually begins four to six weeks after surgery. For patients receiving partial breast radiation, treatment will begin about one week after surgery. There are several possible courses of radiation. Your radiation doctor will discuss the best course for you. Sometimes the cancer cannot be felt during a physical exam. When this happens, a wire or locator device will be placed in your breast the morning of surgery. Medicine to numb the involved area of the breast is given before this device is inserted. This wire or locator device will guide your surgeon to the area of the breast to be removed. Lumpectomy Pros and Cons Pros Cons Outpatient surgery. Greater possibility of re-excision (additional surgery). Shorter recovery. Usually requires radiation. No drain. Possible cosmetic change. -

Consensus Guideline on the Management of the Axilla in Patients with Invasive/In-Situ Breast Cancer
- Official Statement - Consensus Guideline on the Management of the Axilla in Patients With Invasive/In-Situ Breast Cancer Purpose To outline the management of the axilla for patients with invasive and in-situ breast cancer. Associated ASBrS Guidelines or Quality Measures 1. Performance and Practice Guidelines for Sentinel Lymph Node Biopsy in Breast Cancer Patients – Revised November 25, 2014 2. Performance and Practice Guidelines for Axillary Lymph Node Dissection in Breast Cancer Patients – Approved November 25, 2014 3. Quality Measure: Sentinel Lymph Node Biopsy for Invasive Breast Cancer – Approved November 4, 2010 4. Prior Position Statement: Management of the Axilla in Patients With Invasive Breast Cancer – Approved August 31, 2011 Methods A literature review inclusive of recent randomized controlled trials evaluating the use of sentinel lymph node surgery and axillary lymph node dissection for invasive and in-situ breast cancer as well as the pathologic review of sentinel lymph nodes and indications for axillary radiation was performed. This is not a complete systematic review but rather, a comprehensive review of recent relevant literature. A focused review of non-randomized controlled trials was then performed to develop consensus guidance on management of the axilla in scenarios where randomized controlled trials data is lacking. The ASBrS Research Committee developed a consensus document, which was reviewed and approved by the ASBrS Board of Directors. Summary of Data Reviewed Recommendations Based on Randomized Controlled -

Breast Reduction Surgery (Policy OCA 3.44), Effective 08/01/21
bmchp.org | 888-566-0008 wellsense.org | 877-957-1300 Medical Policy Breast Reduction Surgery Policy Number: OCA 3.44 Version Number: 22 Version Effective Date: 08/01/21 + Product Applicability All Plan Products Well Sense Health Plan Boston Medical Center HealthNet Plan Well Sense Health Plan MassHealth ACO MassHealth MCO Qualified Health Plans/ConnectorCare/Employer Choice Direct Senior Care Options ◊ Notes: + Disclaimer and audit information is located at the end of this document. ◊ The guidelines included in this Plan policy are applicable to members enrolled in Senior Care Options only if there are no criteria established for the specified service in a Centers for Medicare & Medicaid Services (CMS) national coverage determination (NCD) or local coverage determination (LCD) on the date of the prior authorization request. Review the member’s product-specific benefit documents at www.SeniorsGetMore.org to determine coverage guidelines for Senior Care Options. Policy Summary Breast reduction surgery (reduction mammoplasty) is considered medically necessary for symptomatic macromastia when Plan criteria are met for a female member (or a member born with female reproductive organs and/or with typical female karyotype with two [2] X chromosomes). The Plan complies with coverage guidelines for all applicable state-mandated benefits and federally-mandated benefits that are medically necessary for the member’s condition. Plan prior authorization is required for reduction mammoplasty. If applicable medical criteria are NOT met, the surgery is considered cosmetic. Breast Reduction Surgery + Plan refers to Boston Medical Center Health Plan, Inc. and its affiliates and subsidiaries offering health coverage plans to enrolled members. The Plan operates in Massachusetts under the trade name Boston Medical Center HealthNet Plan and in other states under the trade name Well Sense Health Plan. -

Breast Imaging Faqs
Breast Imaging Frequently Asked Questions Update 2021 The following Q&As address Medicare guidelines on the reporting of breast imaging procedures. Private payer guidelines may vary from Medicare guidelines and from payer to payer; therefore, please be sure to check with your private payers on their specific breast imaging guidelines. Q: What differentiates a diagnostic from a screening mammography procedure? Medicare’s definitions of screening and diagnostic mammography, as noted in the Centers for Medicare and Medicaid’s (CMS’) National Coverage Determination database, and the American College of Radiology’s (ACR’s) definitions, as stated in the ACR Practice Parameter of Screening and Diagnostic Mammography, are provided as a means of differentiating diagnostic from screening mammography procedures. Although Medicare’s definitions are consistent with those from the ACR, the ACR's definitions of screening and diagnostic mammography offer additional insight into what may be included in these procedures. Please go to the CMS and ACR Web site links noted below for more in- depth information about these studies. Medicare Definitions (per the CMS National Coverage Determination for Mammograms 220.4) “A diagnostic mammogram is a radiologic procedure furnished to a man or woman with signs and symptoms of breast disease, or a personal history of breast cancer, or a personal history of biopsy - proven benign breast disease, and includes a physician's interpretation of the results of the procedure.” “A screening mammogram is a radiologic procedure furnished to a woman without signs or symptoms of breast disease, for the purpose of early detection of breast cancer, and includes a physician’s interpretation of the results of the procedure. -

(NCCN Guidelines®) Breast Cancer
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Breast Cancer Version 4.2017 — February 7, 2018 NCCN.org NCCN Guidelines for Patients® available at www.nccn.org/patients Continue Version 4.2017, 02/07/18 National Comprehensive Cancer Network, Inc. 2018, All rights reserved. The NCCN Guidelines® and this illustration may not be reproduced in any form without the express written permission of NCCN®. Printed by Anton Kabakov on 3/5/2018 6:44:49 AM. For personal use only. Not approved for distribution. Copyright © 2018 National Comprehensive Cancer Network, Inc., All Rights Reserved. NCCN Guidelines Version 4.2017 Panel Members NCCN Guidelines Index Table of Contents Breast Cancer Discussion * William J. Gradishar, MD/Chair ‡ † Sharon H. Giordano, MD, MPH † Lori J. Pierce, MD § Robert H. Lurie Comprehensive Cancer The University of Texas University of Michigan Center of Northwestern University MD Anderson Cancer Center Comprehensive Cancer Center * Benjamin O. Anderson, MD/Vice-Chair ¶ Matthew P. Goetz, MD ‡ † Elizabeth C. Reed, MD † ξ Fred Hutchinson Cancer Research Mayo Clinic Cancer Center Fred & Pamela Buffett Cancer Center Center/Seattle Cancer Care Alliance Lori J. Goldstein, MD † Kilian E. Salerno, MD § Ron Balassanian, MD ≠ Fox Chase Cancer Center Roswell Park Cancer Institute UCSF Helen Diller Family Comprehensive Cancer Center Steven J. Isakoff, MD, PhD † Lee S. Schwartzberg, MD ‡ † Massachusetts General Hospital St. Jude Children’s Research Hospital/ Sarah L. Blair, MD ¶ Cancer Center The University of Tennessee UC San Diego Moores Cancer Center Health Science Center Janice Lyons, MD § Harold J. Burstein, MD, PhD † Case Comprehensive Cancer Center/ Amy Sitapati, MD Þ Dana-Farber/Brigham and Women’s University Hospitals Seidman Cancer Center and UC San Diego Moores Cancer Center Cancer Center Cleveland Clinic Taussig Cancer Institute Karen Lisa Smith, MD, MPH † Amy Cyr, MD ¶ P.