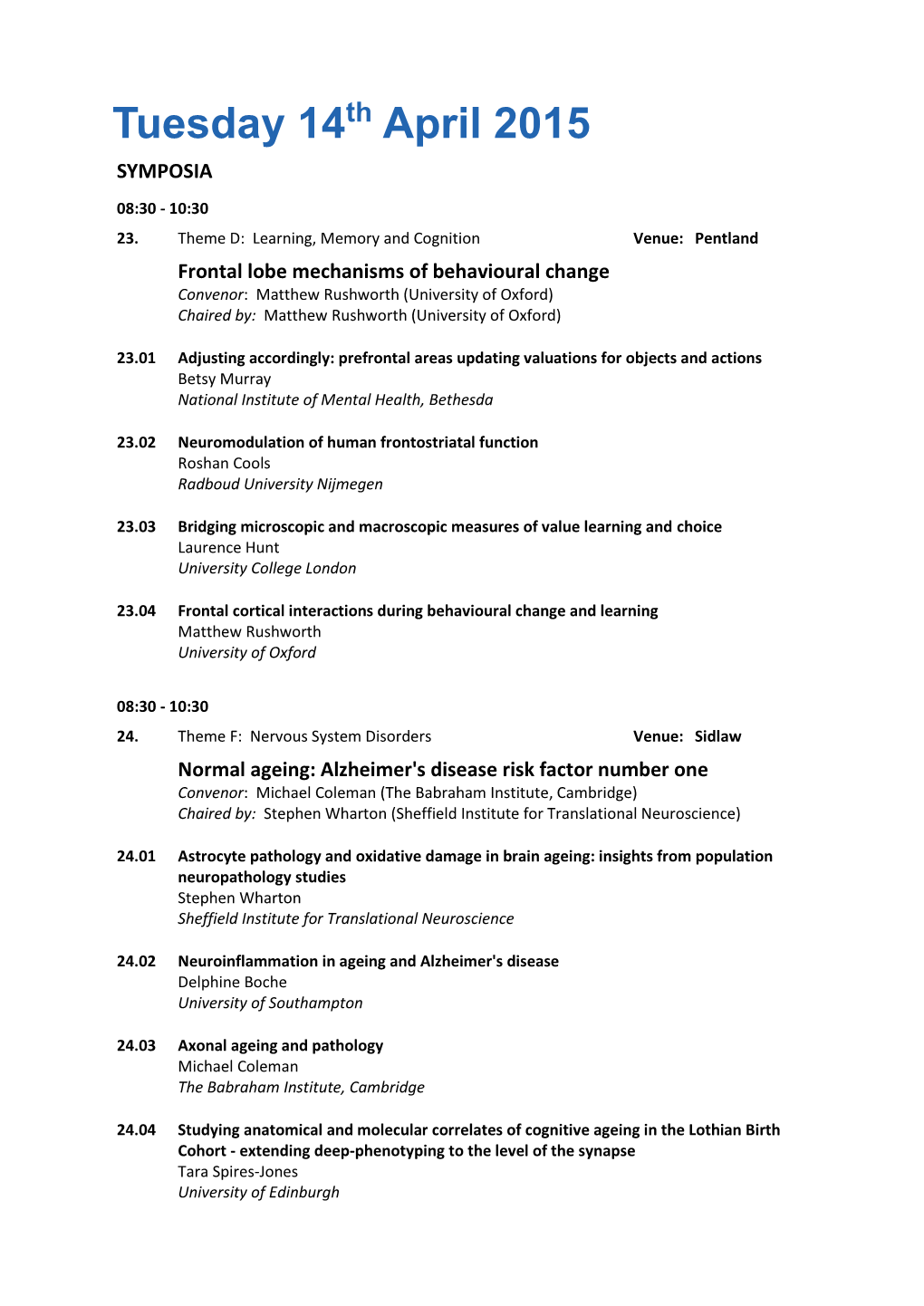
Tuesday 14Th April 2015 SYMPOSIA
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Call for Abstracts International Neuropsychological Society New York City | February 20-23, 2019 INS President: Keith Owen Yeates, Phd Program Chair: Michael W
Call for Abstracts International Neuropsychological Society New York City | February 20-23, 2019 INS President: Keith Owen Yeates, PhD Program Chair: Michael W. Kirkwood, PhD Continuing Education Chair: Melissa Lamar, PhD Submission Opens: May 7, 2018 Submission Closes: August 10, 2018 Message from Michael Kirkwood, 2019 INS Program Committee Chair: Neuropsychology is a melting pot, at the crossroads of neuroscience and behavioral health. To fully understand brain health and illness, we need to consider both neurobiological and psychological processes. We also need to consider developmental factors and the various environmental contexts within which individuals function. Drawing on these ideas, the theme for the 2019 Annual Meeting in New York City is: Embracing the Biopsychosocial Melting Pot. We welcome abstract submissions that represent the interdisciplinary nature of neuropsychology, as well as those that further our understanding of the brain-context relationships that help determine cognitive, emotional, social, and moral development and functioning. As always, we encourage submissions that offer unique insights into cognitive and affective neuroscience of healthy and disease states, innovations in behavioral measurement, and state-of-the-art treatment and rehabilitation approaches. We couldn’t be more excited to be meeting in NYC, its own melting pot of people and cultures. We hope you’ll join us for a stellar scientific program and the virtually endless arts, cultural, and social opportunities that the Big Apple has to offer. -
Download PDF Version of Issue 84
Cambridge Alumni Magazine Issue 84 – Easter 2018 What a snooze fest: why boredom could actually be good for you. Scandi flatpack buildings fit for the Ottoman Emperor. New books, old books, little known books: the summer reading list. Immersive tours of the East; from temples in Varanasi to tea gardens in Kanazawa From India’s Mughal palaces to Japan’s temple gardens, our iti neraries Illustrati on: aquati nt c. 1830 aft er a drawing by Robert Melville Grindlay. across Asia celebrate the cultural achievements of some of the world’s most extraordinary civilisati ons. Explore the Buddhist temples of Varanasi and sail Vietnam’s Perfume River. ‘Every day we got up thinking Interpret the ‘art of the fl oati ng world’ in Kyoto and the exquisite treasures it couldn’t possibly be as good of Ming and Qing Beijing. as the day before, and it was. In all fi ve countries of our Asia programme our expert lecturers enliven Diff erent and wonderful.’ ancient philosophies and dazzling landscapes with their eruditi on and enthusiasm. Expect, equally, high standards of accommodati on and Contact us: privileged access at key sites. +44 (0)20 8742 3355 Our dozen tours in Asia include Sacred India, Kingdoms of the Deccan, Bengal by River, Indian Summer, Ming & Qing Civilisati on, Essenti al China, Japanese marti nrandall.com/asia Gardens, Samarkand & Silk Road Citi es and Vietnam. ATOL 3622 | ABTA Y6050 | AITO 5085 Editor Immersive tours of the East; Mira Katbamna Commissioning editor Steve McGrath from temples in Varanasi to Design and art direction Rob Flanagan University of Cambridge tea gardens in Kanazawa Morven Knowles Cambridge Alumni Magazine Issue 84 Easter 2018 02 INBOX Publisher The University of Cambridge Development & Alumni Relations Campendium 1 Quayside, Bridge Street 30 Cambridge CB5 8AB Tel +44 (0)1223 332288 07 DON’S DIARY Dr Andrew Grant. -

Alzheimers Society Annual Research Review 2017
Annual 2017/ 2018 Research Review 2 Annual Research Review 2017/2018 Foreword Last year we launched our new strategy – the New Deal on Dementia – with a mission to transform the landscape of dementia forever by boosting research, changing society and offering support to everyone affected by dementia. It’s been brilliant to see our strategy take shape over the last 12 months. The UK Dementia Research Institute, our biggest ever single investment in research, is attracting over 400 world-leading scientists to focus their skills and energy on dementia. A partnership between Alzheimer’s Society, the Medical Research Council and Alzheimer’s Research UK, the institute is bringing new laboratories, equipment and researchers into the fight against dementia at an unprecedented scale. Meanwhile, our Centres of Excellence are transforming research into the best dementia care and support. We’ve also led in the development of a roadmap to make sure that care research is prioritised nationally, alongside finding a cure. We know that investments in research pay off. To give just one example, our research fellows made genetic discoveries this year that fundamentally advance our understanding of dementia, bringing personalised medicine ever closer. There are many individual successes to celebrate, but what excites me most is the unique ability of Alzheimer’s Society to unite people who care about dementia, working across all areas to improve people’s lives. In my new role as Chief Policy and Research Officer, I’m bringing people closer together to campaign for research funding, prepare the health and social care system for advances in treatment and diagnosis, and use research insights to improve dementia services. -

Detecting Awareness After Severe Brain Injury
PERSPECTIVES Recently, the results of some functional SCIENCE AND SOCIETY MRI (fMRI) and EEG studies have called into question the extent to which we can Detecting awareness after severe reliably consider a patient unaware simply because they exhibit no overt behavioural brain injury response to external stimulation8–11. Indeed, these studies have revealed a subset of patients who are aware but entirely physi- Davinia Fernández-Espejo and Adrian M. Owen cally unresponsive; thus, although they Abstract | Recent developments in functional neuroimaging have provided a fulfil all internationally agreed criteria for number of new tools for assessing patients who clinically appear to be in a the vegetative state, which are based on vegetative state. These techniques have been able to reveal awareness and even behavioural signs, clear signs of command- following can be demonstrated using fMRI allow rudimentary communication in some patients who remain entirely or EEG. In some cases, these developments behaviourally non-responsive. The implications of these results extend well beyond in functional neuroimaging technology have the immediate clinical and scientific findings to influencing legal proceedings, even allowed such patients to communicate raising new ethical questions about the withdrawal of nutrition and hydration and with the outside world for the first time since 10 providing new options for patients and families in that decision-making process. their brain injury . In this Perspective article, we begin by The findings have also motivated significant public discourse about the role of reviewing the ‘state‑of‑the-art’ of the two neuroscience research in society. methods — fMRI and EEG — that have been successfully used to detect covert aware- The definition and assessment of conscious- The vegetative state is a clinical condi- ness in the vegetative state, with a focus on ness is still one of the most challenging areas tion that is often described as ‘wakefulness the major developments that have emerged of contemporary neuroscience. -

Prion Pathology in the Brainstem: Clinical Target Areas in Prion Disease
PRION PATHOLOGY IN THE BRAINSTEM: CLINICAL TARGET AREAS IN PRION DISEASE A thesis submitted in partial fulfilment for the degree of Doctor of Philosophy to the University College London by Ilaria Mirabile MRC Prion Unit Institute of Neurology University College London 1 Declaration I, Ilaria Mirabile, confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I confirm that this has been indicated in the thesis 2 List of contributions All the procedures described in this thesis were performed by the candidate, with the following exceptions: In vivo procedures Mice breeding, colony maintenance, ear biopsies, prion inoculation, prion symptoms monitoring, mice culling and brain sampling were performed by designated staff at the Prion Unit animal house facility. Prion inocula were prepared by Dr Jonathan Wadsworth. Immunohistochemistry Paraffin embedding and microtome slicing were performed by designated staff in the MRC Prion Unit histology support group. Molecular biology DNA sequencing was performed by Gary Adamson. Cell culture Flow cytometry was performed by Dr Annika Alexopoulou, Dr Sara Monteiro, and Melania Tangari. 3 Acknowledgments I am extremely grateful to all the members of the MRC Prion Unit for their intellectual, practical and moral support. Firstly, I would like to thank my supervisors, Prof. Parmjit Jat, Prof. John Collinge and Prof. Sebastian Brandner for their guidance. I am particularly grateful to Jackie Linehan, Catherine O‘Malley, Caroline Powell and Lorrain Spence in the Histology Core Facility, and to the Prion Unit Animal Facility, for their tremendous hard work. A big thank goes to the members of Prof Parmjit Jat‘s laboratory who welcome me as a second family, to Prof. -
How Neuroscience Technology Is Changing Our Understanding of Brain Injury, Vegetative States and the Law
NORTH CAROLINA JOURNAL OF LAW & TECHNOLOGY Volume 20 Issue 3 Article 2 3-1-2019 How Neuroscience Technology is Changing Our Understanding of Brain Injury, Vegetative States and the Law Glenn R. Butterton Follow this and additional works at: https://scholarship.law.unc.edu/ncjolt Part of the Law Commons Recommended Citation Glenn R. Butterton, How Neuroscience Technology is Changing Our Understanding of Brain Injury, Vegetative States and the Law, 20 N.C. J.L. & TECH. 331 (2019). Available at: https://scholarship.law.unc.edu/ncjolt/vol20/iss3/2 This Article is brought to you for free and open access by Carolina Law Scholarship Repository. It has been accepted for inclusion in North Carolina Journal of Law & Technology by an authorized editor of Carolina Law Scholarship Repository. For more information, please contact [email protected]. NORTH CAROLINA JOURNAL OF LAW & TECHNOLOGY VOLUME 20, ISSUE 3: MARCH 2019 HOW NEUROSCIENCE TECHNOLOGY IS CHANGING OUR UNDERSTANDING OF BRAIN INJURY, VEGETATIVE STATES AND THE LAW Glenn R. Butterton* The author examines clinical studies that use neuroscience technology to study patients in Vegetative States. The studies indicate that some of the patients are, in fact, conscious. The author suggests that this finding is a matter of considerable practical importance for the drafting and execution of end-of-life protocols such as Advance Directives and Living Wills. He recommends that statutes, and other guidance used by patients, caregivers, medical institutions, family members and others to draft and interpret such Directives and Wills, be revised or amended to take account of these results. I. INTRODUCTION ........................................................................332 II. -

Anesthesia and Neuroimaging: Investigating the Neural Correlates
Review Anesthesia and neuroimaging: investigating the neural correlates of unconsciousness 1 1 2 2 Alex A. MacDonald , Lorina Naci , Penny A. MacDonald , and Adrian M. Owen 1 Undergraduate Medical Program, Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada 2 The Brain and Mind Institute, The Natural Sciences Centre, University of Western Ontario, London, Ontario, Canada In the past 15 years, rapid technological development in agents both complement and extend results from tradi- the field of neuroimaging has led to a resurgence of tional psychophysical studies. interest in the study of consciousness. However, the In the following we summarize findings from functional neural bases of consciousness and the boundaries of neuroimaging studies that have used anesthetic agents to unconscious processing remain poorly understood. An- study changes in brain activation at reduced levels of esthesia combined with functional neuroimaging pre- awareness, both with sensory stimulation and at rest. sents a unique approach for studying neural responses We then relate these results to those obtained with brain as a function of consciousness. In this review we sum- imaging (i) using traditional psychophysical manipula- marize findings from functional neuroimaging studies tions of awareness, and (ii) in behaviorally non-responsive that have used anesthetic drugs to study cognition at patients. In the latter case, we discuss how studies that different levels of conscious awareness. We relate the have used anesthetic drugs to modulate the level of aware- results to those of psychophysical studies of cognition ness might inform diagnoses in disorders of consciousness. and explore their potential usefulness in interpreting We focus on cognitive systems that have been studied clinical findings from studies of non-responsive patients. -
42Db806284f0469eb175c7556318039c Aalves
http://www.skymem.com/xdoc/document-2015-3-3t05-02-02-3131z- 42db806284f0469eb175c7556318039c [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] -

Joern R Steinert, Tatyana Chernova, Ian D Forsythe Hans H
ISSN 1473-9348 VOLUME 9 ISSUE 5 NOVEMBER/DECEMBER 2009 ACNRwww.acnr.co.uk ADVANCES IN CLINICAL NEUROSCIENCE & REHABILITATION In this issue Joern R Steinert, Tatyana Chernova, Ian D Forsythe Nitric Oxide In Brain Function and Dysfunction Hans H Jung, Adrian Danek, Ruth H Walker Neuroacanthocytosis Heather Angus-Leppan, Charles Warlow Health Records: out of the frying pan? Justin Cross, HK Cheow Nuclear Medicine in Neurology NEWS REVIEW > CONFERENCE REPORTS > BOOK REVIEWS > EVENTS DIARY Azilect® 1mg tablets Prescribing information (Please refer to the Summary of Product in patients with moderate hepatic impairment. Use caution in patients with mild hepatic Characteristics (SmPC) before prescribing) Presentation: Tablets containing 1mg rasagiline (as impairment. Use with caution in pregnancy or lactation. There is an increased risk of skin cancer the mesilate). Indication: Treatment of idiopathic Parkinson’s disease as monotherapy or as in Parkinson’s disease, not associated with any particular drug. Suspicious skin lesions require adjunct to levodopa in patients with end of dose fluctuations. Dosage and administration: specialist evaluation. Undesirable effects in clinical trials: Monotherapy: >1%: headache, flu Oral, 1mg once daily taken with or without food. Elderly: No change in dosage required. syndrome, malaise, neck pain, dyspepsia, arthralgia, depression, conjunctivitis, allergic reaction, Children and adolescents (<18 years): Not recommended. Patients with renal impairment: No fever, angina pectoris, anorexia, leucopenia, arthritis, vertigo, rhinitis, contact dermatitis, change in dosage required. Patients with hepatic impairment: Predominant hepatic metabolism. vesiculobullous rash, skin carcinoma, hallucinations, urinary urgency. <1%: cerebrovascular Do not use in patients with severe impairment. Avoid use in patients with moderate impairment. accident, myocardial infarct. -
Update on the Pathophysiology of Prion Diseases
ACNRSO14_Layout 1 04/09/2014 22:13 Page 6 REVIEW ARTICLE Update on the Pathophysiology of Prion Diseases extensive neuronal cell loss. Whilst PrP Sc is asso - Summary ciated with infectivity (prion diseases are trans - • Prion diseases are characterised by the missible), there is extensive evidence that it is not accumulation of misfolded prion protein in itself neurotoxic. Sub-clinical states of prion (PrP) and widespread neuronal loss disease have been identified in which extensive throughout the brain. Recent work has accumulation of PrP Sc is dissociated from neuro - elucidated a major mechanism by which toxicity. 3 PrP Sc is harmless to cells devoid of PrP C, misfolded PrP induces neurodegeneration and therapeutic agents targeting PrP Sc have very in prion disease. limited efficacy and do not prevent neuronal • Rising levels of misfolded PrP lead to C Giovanna Mallucci loss. PrP is absolutely required for susceptibility sustained dysregulation of an endogenous to prion neurotoxicity: PrP-null mice are resistant is Professor of Neuroscience and cellular pathway, the unfolded protein Programme Leader at the MRC to prion disease 4 and depleting PrP C in neurons response (UPR), which regulates protein Toxicology Unit and Honorary of prion infected mice cures disease, as conver - Consultant Neurologist at synthesis at the level of translation sion can no longer occur. 5 Thus, the process of Addenbrooke's Hospital, with a initiation. prion protein misfolding is central to neurotoxi - specialist interest in dementia. She • This results in the sustained reduction in city. Recent work has shown that neuronal death gained her PhD in 2001 from Imperial global protein synthesis rates in neurons, College, London, developing a new leading to loss of critical proteins, results from dysregulation of the cellular transgenic model of 'reversible’ prion response to unfolded proteins triggered by the disease, after which she combined resulting in synaptic failure and neuronal 6 scientific and clinical careers focused death. -

Canadian Perspectives on the Clinical Actionability of Neuroimaging in Disorders of Consciousness
ORIGINAL ARTICLE COPYRIGHT © 2015 THE CANADIAN JOURNAL OF NEUROLOGICAL SCIENCES INC. Canadian Perspectives on the Clinical Actionability of Neuroimaging in Disorders of Consciousness Grace Lee, Adrian C. Byram, Adrian M. Owen, Urs Ribary, A. Jon Stoessl, Andrea Townson, Christine Stables, Judy Illes ABSTRACT: Background: Acquired brain injury is a critical public health and socioeconomic problem in Canada, leaving many patients in vegetative, minimally conscious, or locked-in states, unresponsive and unable to communicate. Recent advances in neuroimaging research have demonstrated residual consciousness in a few exemplary patients with acquired brain injury, suggesting potential misdiagnosis and changes in prognosis. Such progress, in parallel with research using multimodal brain imaging technologies in recent years, has promising implications for clinical translation, notwithstanding the many challenges that impact health care and policy development. This study explored the perspectives of Canadian professionals with expertise either in neuroimaging research, disorders of consciousness, or both, on the potential clinical applications and implications of imaging technology. Methods: Twenty-two professionals from designated communities of neuroimaging researchers, ethicists, lawyers, and practitioners participated in semistructured interviews. Data were analyzed for emergent themes. Results: The five most dominant themes were: (1) validation and calibration of the methods; (2) informed consent; (3) burdens on the health care system; (4) implications for the Canadian health care system; and (5) possibilities for improved prognosis. Conclusions: Movement of neuroimaging from research into clinical care for acquired brain injury will require careful consideration of legal and ethical issues alongside research reliability, responsible distribution of health care resources, and the interaction of technological capabilities with patient outcome. -

Anesthesia and Neuroimaging: Investigating the Neural
Review Anesthesia and neuroimaging: investigating the neural correlates of unconsciousness 1 1 2 2 Alex A. MacDonald , Lorina Naci , Penny A. MacDonald , and Adrian M. Owen 1 Undergraduate Medical Program, Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada 2 The Brain and Mind Institute, The Natural Sciences Centre, University of Western Ontario, London, Ontario, Canada In the past 15 years, rapid technological development in agents both complement and extend results from tradi- the field of neuroimaging has led to a resurgence of tional psychophysical studies. interest in the study of consciousness. However, the In the following we summarize findings from functional neural bases of consciousness and the boundaries of neuroimaging studies that have used anesthetic agents to unconscious processing remain poorly understood. An- study changes in brain activation at reduced levels of esthesia combined with functional neuroimaging pre- awareness, both with sensory stimulation and at rest. sents a unique approach for studying neural responses We then relate these results to those obtained with brain as a function of consciousness. In this review we sum- imaging (i) using traditional psychophysical manipula- marize findings from functional neuroimaging studies tions of awareness, and (ii) in behaviorally non-responsive that have used anesthetic drugs to study cognition at patients. In the latter case, we discuss how studies that different levels of conscious awareness. We relate the have used anesthetic drugs to modulate the level of aware- results to those of psychophysical studies of cognition ness might inform diagnoses in disorders of consciousness. and explore their potential usefulness in interpreting We focus on cognitive systems that have been studied clinical findings from studies of non-responsive patients.