Childhood Nephrotic Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Uremic Toxins Affect Erythropoiesis During the Course of Chronic
cells Review Uremic Toxins Affect Erythropoiesis during the Course of Chronic Kidney Disease: A Review Eya Hamza 1, Laurent Metzinger 1,* and Valérie Metzinger-Le Meuth 1,2 1 HEMATIM UR 4666, C.U.R.S, Université de Picardie Jules Verne, CEDEX 1, 80025 Amiens, France; [email protected] (E.H.); [email protected] (V.M.-L.M.) 2 INSERM UMRS 1148, Laboratory for Vascular Translational Science (LVTS), UFR SMBH, Université Sorbonne Paris Nord, CEDEX, 93017 Bobigny, France * Correspondence: [email protected]; Tel.: +33-2282-5356 Received: 17 July 2020; Accepted: 4 September 2020; Published: 6 September 2020 Abstract: Chronic kidney disease (CKD) is a global health problem characterized by progressive kidney failure due to uremic toxicity and the complications that arise from it. Anemia consecutive to CKD is one of its most common complications affecting nearly all patients with end-stage renal disease. Anemia is a potential cause of cardiovascular disease, faster deterioration of renal failure and mortality. Erythropoietin (produced by the kidney) and iron (provided from recycled senescent red cells) deficiencies are the main reasons that contribute to CKD-associated anemia. Indeed, accumulation of uremic toxins in blood impairs erythropoietin synthesis, compromising the growth and differentiation of red blood cells in the bone marrow, leading to a subsequent impairment of erythropoiesis. In this review, we mainly focus on the most representative uremic toxins and their effects on the molecular mechanisms underlying anemia of CKD that have been studied so far. Understanding molecular mechanisms leading to anemia due to uremic toxins could lead to the development of new treatments that will specifically target the pathophysiologic processes of anemia consecutive to CKD, such as the newly marketed erythropoiesis-stimulating agents. -

Glomerulonephritis Management in General Practice
Renal disease • THEME Glomerulonephritis Management in general practice Nicole M Isbel MBBS, FRACP, is Consultant Nephrologist, Princess Alexandra lomerular disease remains an important cause Hospital, Brisbane, BACKGROUND Glomerulonephritis (GN) is an G and Senior Lecturer in important cause of both acute and chronic kidney of renal impairment (and is the commonest cause Medicine, University disease, however the diagnosis can be difficult of end stage kidney disease [ESKD] in Australia).1 of Queensland. nikky_ due to the variability of presenting features. Early diagnosis is essential as intervention can make [email protected] a significant impact on improving patient outcomes. OBJECTIVE This article aims to develop However, presentation can be variable – from indolent a structured approach to the investigation of patients with markers of kidney disease, and and asymptomatic to explosive with rapid loss of kidney promote the recognition of patients who need function. Pathology may be localised to the kidney or further assessment. Consideration is given to the part of a systemic illness. Therefore diagnosis involves importance of general measures required in the a systematic approach using a combination of clinical care of patients with GN. features, directed laboratory and radiological testing, DISCUSSION Glomerulonephritis is not an and in many (but not all) cases, a kidney biopsy to everyday presentation, however recognition establish the histological diagnosis. Management of and appropriate management is important to glomerulonephritis (GN) involves specific therapies prevent loss of kidney function. Disease specific directed at the underlying, often immunological cause treatment of GN may require specialist care, of the disease and more general strategies aimed at however much of the management involves delaying progression of kidney impairment. -

Pyelonephritis (Kidney Infection)
Pyelonephritis (Kidney Infection) Cathy E. Langston, DVM, DACVIM (Small Animal) BASIC INFORMATION urine collected from the bladder to be negative despite infection in the Description kidney. Abdominal x-rays and an ultrasound may be recommended. Bacterial infection of the kidney is termed pyelonephritis . Infection Although culture of a piece of kidney tissue obtained by biopsy may occur within kidney tissue or in the renal pelvis, the area of increases the chance of finding the infection, the invasiveness of the kidney where urine collects before being transported to the the procedure makes it too risky for general use (the biopsy would bladder. need to be taken from deeper within the kidney than the average Causes kidney biopsy). Contrast x-ray studies, such as an excretory uro- In most cases, a urinary tract infection starts in the bladder and gram (intravenous pyelogram), are sometimes helpful. An excre- the bacteria travel upstream to the kidney. Anything that decreases tory urogram involves taking a series of x-rays after a dye (that the free flow of urine, such as obstruction of the urethra (tube shows up white on x-rays) is given intravenously. Other tests may that carries urine from the bladder to the outside), bladder, ureter be recommended to rule out diseases that cause similar clinical (tube that carries urine from the kidney to the bladder), or kid- signs and other causes of kidney disease. ney, increases the risk that the infection will spread to the kid- ney. The presence of stones and growths in the bladder and kidney TREATMENT AND FOLLOW-UP also increases the risk. -
Urinalysis and Kidney Disease: What You Need to Know
URINALYSIS AND KIDNEY DISEASE What You Need To Know www.kidney.org About the Information in this Booklet Did you know that the National Kidney Foundation (NKF) offers guidelines and commentaries that help your healthcare provider make decisions about your medical treatment? The information in this booklet is based on those recommended guidelines. Stages of Kidney Disease There are five stages of kidney disease. They are shown in the table below. Your healthcare provider determines your stage of kidney disease based on the presence of kidney damage and your glomerular filtration rate (GFR), which is a measure of your kidney function. Your treatment is based on your stage of kidney disease. Speak to your healthcare provider if you have any questions about your stage of kidney disease or your treatment. STAGES OF KIDNEY DISEASE Glomerular Stage Description Filtration Rate (GFR)* Kidney damage (e.g., protein 1 90 or above in the urine) with normal GFR Kidney damage with mild 2 60 to 89 decrease in GFR 3 Moderate decrease in GFR 30 to 59 4 Severe reduction in GFR 15 to 29 5 Kidney failure Less than 15 *Your GFR number tells your healthcare provider how much kidney function you have. As chronic kidney disease progresses, your GFR number decreases. What is a urinalysis (also called a “urine test”)? A urinalysis is a simple test that looks at a small sample of your urine. It can help find conditions that may need treatment, including infections or kidney problems. It can also help find serious diseases in the early stages, like chronic kidney disease, diabetes, or liver disease. -

High Blood Pressure and Chronic Kidney Disease: for People
HIGH BLOOD PRESSURE AND CHRONIC KIDNEY DISEASE For People with CKD Stages 1–4 www.kidney.org National Kidney Foundation's Kidney Disease Outcomes Quality Initiative Did you know that the National Kidney Foundation's Kidney Disease Outcomes Quality Initiative (NKF-KDOQI™) has guidelines and commentaries that help your doctor and healthcare team make important decisions about your medical treatment? The information in this booklet is based on the NKF- KDOQI recommended guidelines and commentaries. What is your stage of kidney disease? There are five stages of kidney disease. They are shown in the table below. Your doctor determines your stage of kidney disease based on the presence of kidney damage and your glomerular filtration rate (GFR), which is a measure of your level of kidney function. Your treatment is based on your stage of kidney disease. Speak to your doctor if you have any questions about your stage of kidney disease or your treatment. STAGES of KidNEY DISEASE AGES of KidNEY DISEASE STAGES OF KIDNEY DISEASE Stage Description Glomerular Filtration Rate (GFR)* Kidney damage (e.g., protein 1 90 or above in the urine) with normal GFR Kidney damage with mild 2 60 to 89 decrease in GFR 3 Moderate decrease in GFR 30 to 59 4 Severe reduction in GFR 15 to 29 5 Kidney failure Less than 15 *Your GFR number tells your doctor how much kidney function you have. As chronic kidney disease progresses, your GFR number decreases. 2 NATIONAL KIDNEY FOUNDATION TABLE of ConTEntS Did you know? ...............................4 What is chronic kidney disease? ................5 What is high blood pressure? ...................6 How are high blood pressure and kidney disease related? ..............................6 How do I know if my blood pressure is too high? ..................................7 How is blood pressure measured? How often should it be checked? ...............8 I have high blood pressure but am not sure if I have CKD. -
What Is Lupus Nephritis
What is lupus nephritis (LN)? Lupus nephritis (LN) is inflammation of the kidney that occurs as a common symptom of systemic lupus erythematosus (SLE), also known as lupus. Proteins in the immune system called antibodies damage important structures in the kidney. ⅱ Why are the kidneys important? To understand how lupus nephritis damages the kidney, it is important to understand how the kidneys work. The kidneys’ main function is to filter out excess waste and water from the blood through the urine. Kidneys also balance the salts and minerals circulating in the blood, help control blood pressure and make red blood cells. So, when the kidneys are damaged or fail, they can’t do their job as well. As a result, the kidneys are not able to filter out waste and water into the urine causing it to stay in the blood. What are the signs and symptoms of LN? Signs to ask the doctor about include blood in the urine or foamy urine which can mean that there is excess protein. Other signs to notice are swelling of legs, ankles, hands or tissue around the eyes as well as weight gain that can be caused by fluid the body isn’t getting rid of. ⅲ Symptoms of lupus nephritis also include high blood pressure, joint/muscle pain, high levels of waste (creatinine) in the blood, or impaired/failing kidney. ⅳ How common is LN? Lupus nephritis is the most common complication of lupus. Five out of 10 adults with lupus will have lupus nephritis, while eight out of 10 children with lupus will have kidney damage, which usually stems from lupus nephritis. -

Chronic Kidney Disease (Ckd)
CHRONIC KIDNEY DISEASE ISSUE BRIEF prevent and control progressiveawareness obesity untreated end-stage renal disease kidney failure heart disease high blood pressure lifestyle changes stages complications family history damage to kidneys diabetes CKD few signs or symptoms PROGRESSION OF CHRONIC KIDNEY DISEASE (CKD) RISK FACTORS FOR CKD MAY INCLUDE ■ Heart Disease ■ Lupus ■ Diabetes ■ Family History of CKD ■ High Blood Pressure ■ Age ■ Obesity ■ High Cholesterol REDUCED INCREASED KIDNEY KIDNEY NORMAL KIDNEY RISK DAMAGE FUNCTION FAILURE Preventing CKD and its complications is possible by managing risk factors and treating the disease to slow its progression and reduce the risk of complications PROGRESSION OF CHRONIC KIDNEY DISEASE (CKD) What Is Chronic Kidney Disease? Fast Fact: Kidney diseases are the 9th leading cause of death in the United States. ■ Chronic kidney disease (CKD) is a condition in which a person has damaged kidneys or reduced kidney function for more than 3 months. During this time, the kidneys cannot properly filter waste out of the blood. If not detected and treated early, CKD can cause many health problems and even lead to kidney failure and early death. ■ CKD can start at any age, but the chances of developing it increase as people get older. It is most common among adults aged 70 years or older. ■ Once a person has CKD, it usually gets worse over time and lasts for the rest of the person’s life. Kidney failure—also called end-stage renal disease—is the final stage of CKD, when the kidneys stop working completely. How Big Is the CKD Problem and Who Is at Risk? Fast Fact: CDC estimates that more 6% than 20 million US adults aged 20 Unknown years or older have CKD—or more than 10% of the US adult population. -
2012 CKD Guideline
OFFICIAL JOURNAL OF THE INTERNATIONAL SOCIETY OF NEPHROLOGY KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease VOLUME 3 | ISSUE 1 | JANUARY 2013 http://www.kidney-international.org KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease KDIGO gratefully acknowledges the following consortium of sponsors that make our initiatives possible: Abbott, Amgen, Bayer Schering Pharma, Belo Foundation, Bristol-Myers Squibb, Chugai Pharmaceutical, Coca-Cola Company, Dole Food Company, Fresenius Medical Care, Genzyme, Hoffmann-LaRoche, JC Penney, Kyowa Hakko Kirin, NATCO—The Organization for Transplant Professionals, NKF-Board of Directors, Novartis, Pharmacosmos, PUMC Pharmaceutical, Robert and Jane Cizik Foundation, Shire, Takeda Pharmaceutical, Transwestern Commercial Services, Vifor Pharma, and Wyeth. Sponsorship Statement: KDIGO is supported by a consortium of sponsors and no funding is accepted for the development of specific guidelines. http://www.kidney-international.org contents & 2013 KDIGO VOL 3 | ISSUE 1 | JANUARY (1) 2013 KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease v Tables and Figures vii KDIGO Board Members viii Reference Keys x CKD Nomenclature xi Conversion Factors & HbA1c Conversion xii Abbreviations and Acronyms 1 Notice 2 Foreword 3 Work Group Membership 4 Abstract 5 Summary of Recommendation Statements 15 Introduction: The case for updating and context 19 Chapter 1: Definition, and classification -

National Kidney and Urologic Diseases Information Clearinghouse 05/13/14 U.S
Proteinuria - National Kidney and Urologic Diseases Information Clearinghouse 05/13/14 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Site Map | FAQS | Contact NIDDK | National Kidney and Urologic Diseases Information Clearinghouse (NKUDIC) A service of the National Institute of Diabetes and Digestive and Kidney SEARCH Advanced Search Diseases (NIDDK), National Institutes of Health (NIH) HOME KIDNEY INFO STATISTICS RESEARCH RESOURCES ORDER ABOUT US ESPAÑOL National Kidney and Health Information Urologic Diseases Services Information Clearinghouse National Diabetes Information Clearinghouse Publications National Digestive Diseases Home : Kidney and Urologic Diseases A-Z List of Topics and Titles : Proteinuria Information Clearinghouse Tools and Resources Proteinuria National Kidney and Urologic E-News Diseases Information Clearinghouse Alternate Version On this page: National Endocrine and Print PDF Version (487 KB) * Metabolic Diseases Information What is proteinuria? Service Also see: Who is at risk for proteinuria? National Hematologic Diseases Information Service Kidney Disease of Diabetes What are the signs and symptoms of proteinuria? Weight-control Information High Blood Pressure and What are the tests for proteinuria? Kidney Disease Network What additional tests for kidney disease may be needed? The Kidneys and How They Work What should a person with proteinuria do? Education Programs Points to Remember National Diabetes Education Subscribe to E-news Program Go Hope through Research National Kidney Disease For More Information Education Program Acknowledgments Awareness Campaigns Let’s Talk about Bowel Control What is proteinuria? Celiac Disease Awareness Proteinuria—also called albuminuria or urine albumin—is a condition in which Campaign urine contains an abnormal amount of protein. Albumin is the main protein in Bladder Control for Women the blood. -

Hematuria: Blood in the Urine
Hematuria: Blood in the Urine National Kidney and Urologic Diseases Information Clearinghouse What is hematuria? Hematuria is blood in the urine. Two types of blood in the urine exist. Blood that can be seen in the urine is called gross hematu- U.S. Department of Health and ria. Blood that cannot be seen in the urine, Human Services except when examined with a microscope, is called microscopic hematuria. NATIONAL INSTITUTES OF HEALTH What are the symptoms of Kidneys hematuria? Most people with microscopic hematuria do not have symptoms. People with gross hematuria have urine that is pink, red, or cola-colored due to the presence of red blood cells (RBCs). Even a small amount of Bladder blood in the urine can cause urine to change Ureters color. In most cases, people with gross hematuria do not have other symptoms. However, people with gross hematuria that Urethra includes blood clots in the urine may have pain. The urinary tract What is the urinary tract? the two kidneys process about 200 quarts The urinary tract is the body’s drainage of blood to produce about 1 to 2 quarts of system for removing wastes and extra water. urine, composed of wastes and extra water. The urinary tract includes two kidneys, two The urine flows from the kidneys to the ureters, a bladder, and a urethra. The kid- bladder through tubes called ureters. The neys are two bean-shaped organs, each about bladder stores urine until releasing it through the size of a fist. They are located near the urination. When the bladder empties, urine middle of the back, just below the rib cage, flows out of the body through a tube called one on each side of the spine. -

People with Lupus Are Much More Likely to Have Kidney Disease Than People Who Don't Have Lupus
Lupus and kidney disease What does kidney disease have to do with lupus? People with lupus are much more likely to have kidney disease than people who don't have lupus. The kidneys are the organs that make urine. Kidneys filter the blood by putting the waste products into the urine where they can leave the body. Kidney disease can cause blood and protein in the urine, swelling of the body, high blood pressure, and other symptoms. "Lupus nephritis" is the medical name for a type of kidney disease in people with lupus. People who have lupus can also get kidney disease caused by other problems. For example, if someone with lupus also has diabetes, the diabetes might be the cause of kidney problems. The way we find out is by doing a kidney biopsy. Types of Lupus Nephritis: There are several types or “classes” of lupus nephritis. They range from Class I to Class 6: Class 1 disease is mild, Classes 2 and 5 are moderate Classes 3 and 4 are aggressive, Class 6 indicates severe non-reversible disease. What are the symptoms of lupus nephritis? Foamy Urine- This is often one of the first signs of lupus nephritis Blood in the Urine- This is also often one of the first signs of lupus nephritis Swelling- Usually in the legs, feet, or ankles and less often in the hands or face. This tends to worsen as the day progresses or after sitting (this is called edema) High Blood Pressure Changes in Frequency of Urination– Either much more or much less Vomiting- Toxins that build up because the kidney is unable to remove them from the body can result in abnormal function of the liver and the process of digestion. -
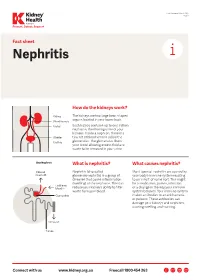
Nephritis Fact Sheet
Last Reviewed March 2017 Page 1 Prevent, Detect, Support. Fact sheet Nephritis How do the kidneys work? The kidneys are two large bean-shaped organs located in your lower back. Each kidney contains up to one million nephrons, the filtering units of your kidneys. Inside a nephron, there is a tiny set of blood vessels called the glomerulus. The glomerulus filters your blood allowing excess fluid and waste to be removed in your urine. What is nephritis? What causes nephritis? Nephritis (also called Most types of nephritis are caused by glomerulonephritis) is a group of your body’s immune system reacting diseases that cause inflammation to an ‘insult’ of some sort. This might (swelling) of the nephrons. This can be a medication, poison, infection reduce your kidney’s ability to filter or a change in the way your immune waste from your blood. system behaves. Your immune system makes antibodies to attack bacteria or poisons. These antibodies can damage your kidneys and nephrons, causing swelling and scarring. Connect with us www.kidney.org.au Freecall 1800 454 363 Kidney Health Australia Nephritis Last Reviewed March 2017 Prevent, Detect, Support. Page 2 What are the different types of nephritis? There are many different types of Different types of nephritis include: Nephrotic syndrome: Damage to the nephritis. It can vary from a mild, nephrons causes them to leak large Focal nephritis: Less than a half of non-damaging condition to a serious amounts of protein into your urine your nephrons have scarring, and problem causing kidney failure. Some but little blood. Losing this protein blood and a small amount of protein types of nephritis appear mild at means your body does not have are found in your urine.