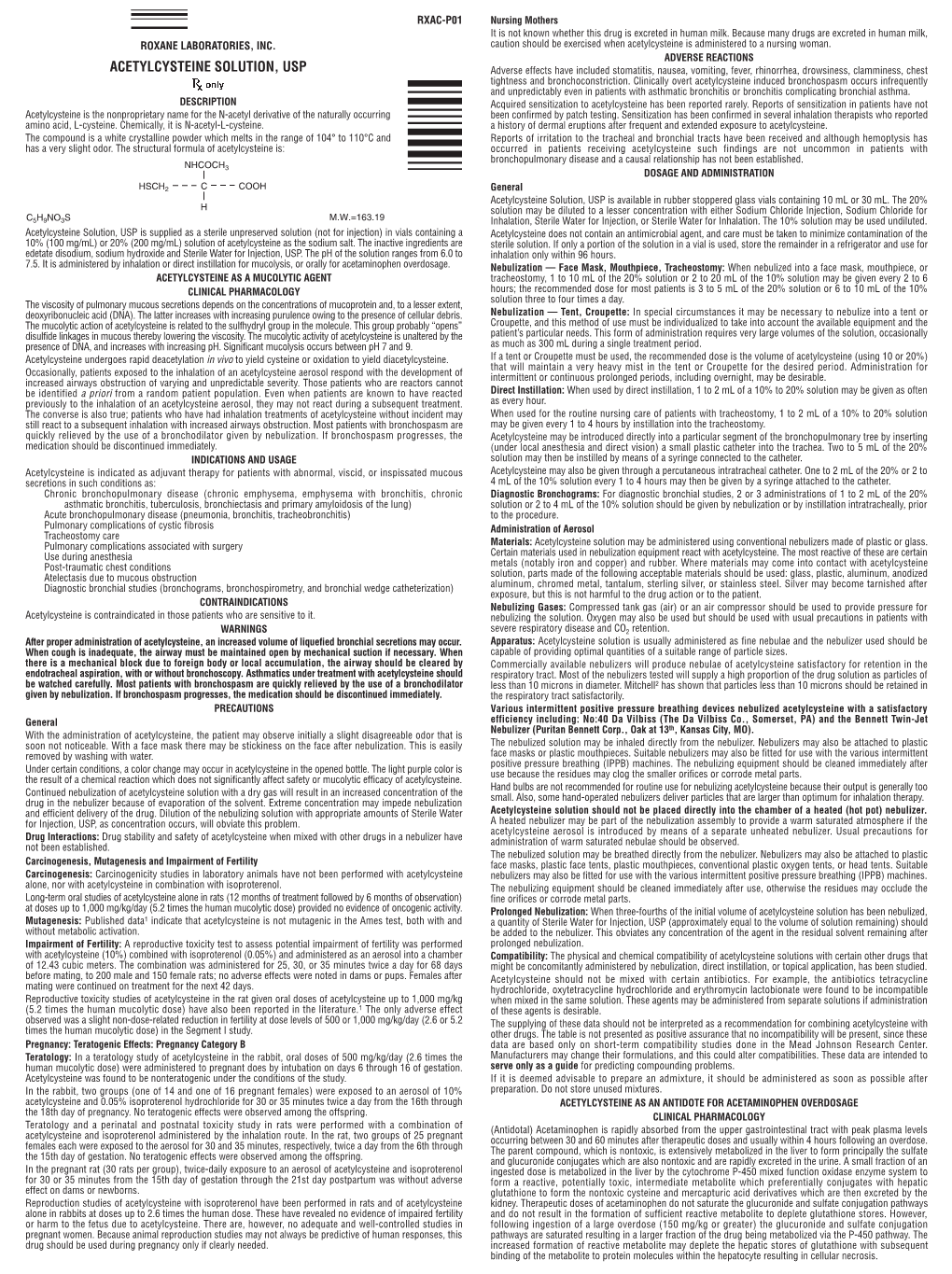
Acetylcysteine Solution
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Activated Charcoal for Acute Poisoning: One Toxicologist's Journey
J. Med. Toxicol. (2010) 6:190–198 DOI 10.1007/s13181-010-0046-1 REVIEW ARTICLE Activated Charcoal for Acute Poisoning: One Toxicologist’s Journey Kent R. Olson Published online: 20 May 2010 # The Author(s) 2010. This article is published with open access at Springerlink.com Keywords Activated charcoal . Gastrointestinal As summarized by Matthew [13], Harstad and Danish decontamination . Poisoning . Drug overdose colleagues reported in 1942 that relatively little phenobar- bital was recovered by lavage even shortly after overdose [14] and this, along with their finding of particles of When I began studying clinical toxicology in 1981, the issue charcoal in the lungs of patients who died, led them to call of gastrointestinal decontamination after acute ingestion for the abandonment of gastric lavage for poisoning.) “ ” seemed pretty well settled: universal antidote, apomor- In recent years, my colleagues and I have continued to – phine and salt wateremesiswerenolongerused[1, 2]; and I debate the value of various methods of gastric decontam- was taught that barring a specific contraindication, the awake ination and the role and risks of activated charcoal, and it is patient was given syrup of ipecac to induce emesis, and the clear to me that the issue remains muddy. Some have taken drowsy or uncooperative patient was lavaged [3]. After a firm stand that no treatment should be recommended that is gastric emptying, everyone received activated charcoal not supported by evidence from a randomized controlled trial (AC). The only controversy seemed to be over whether one (RCT). Position statements published jointly by the Amer- should add a cathartic to speed gastrointestinal transit [4]. -

Thermal Decomposition of the Amino Acids Glycine, Cysteine, Aspartic Acid, Asparagine, Glutamic Acid, Glutamine, Arginine and Histidine
bioRxiv preprint doi: https://doi.org/10.1101/119123; this version posted March 22, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Thermal decomposition of the amino acids glycine, cysteine, aspartic acid, asparagine, glutamic acid, glutamine, arginine and histidine Ingrid M. Weiss*, Christina Muth, Robert Drumm & Helmut O.K. Kirchner INM-Leibniz Institute for New Materials, Campus D2 2, D-66123 Saarbruecken Germany *Present address: Universität Stuttgart, Institut für Biomaterialien und biomolekulare Systeme, Pfaffenwaldring 57, D-70569 Stuttgart, Germany Abstract Calorimetry, thermogravimetry and mass spectrometry were used to follow the thermal decomposition of the eight amino acids G, C, D, N, E, Q, R and H between 185°C and 280°C. Endothermic heats of decomposition between 72 and 151 kJ/mol are needed to form 12 to 70 % volatile products. This process is neither melting nor sublimation. With exception of cysteine they emit mainly H2O, some NH3 and no CO2. Cysteine produces CO2 and little else. The reactions are described by polynomials, AA → a (NH3) + b (H2O) + c (CO2) + d (H2S) + e (residue), with integer or half integer coefficients. The solid monomolecular residues are rich in peptide bonds. 1. Motivation Amino acids might have been synthesized under prebiological conditions on earth or deposited on earth from interstellar space, where they have been found [Follmann and Brownson, 2009]. Robustness of amino acids against extreme conditions is required for early occurrence, but little is known about their nonbiological thermal destruction. There is hope that one might learn something about the molecules needed in synthesis from the products found in decomposition. -

Acetadote (Acetylcysteine) Injection Is Available As a 20% Solution in 30 Ml (200Mg/Ml) Single Dose Glass Vials
NDA 21-539/S-004 Page 3 Acetadote® (acetylcysteine) Injection Package Insert NDA 21-539/S-004 Page 4 RX ONLY PRESCRIBING INFORMATION ACETADOTE® (acetylcysteine) Injection For Intravenous Use DESCRIPTION Acetylcysteine injection is an intravenous (I.V.) medication for the treatment of acetaminophen overdose. Acetylcysteine is the nonproprietary name for the N-acetyl derivative of the naturally occurring amino acid, L-cysteine (N-acetyl-L-cysteine, NAC). The compound is a white crystalline powder, which melts in the range of 104° to 110°C and has a very slight odor. The molecular formula of the compound is C5H9NO3S, and its molecular weight is 163.2. Acetylcysteine has the following structural formula: H CH3 N SH O COOH Acetadote is supplied as a sterile solution in vials containing 20% w/v (200 mg/mL) acetylcysteine. The pH of the solution ranges from 6.0 to 7.5. Acetadote contains the following inactive ingredients: 0.5 mg/mL disodium edetate, sodium hydroxide (used for pH adjustment), and Sterile Water for Injection, USP. CLINICAL PHARMACOLOGY Acetaminophen Overdose: Acetaminophen is absorbed from the upper gastrointestinal tract with peak plasma levels occurring between 30 and 60 minutes after therapeutic doses and usually within 4 hours following an overdose. It is extensively metabolized in the liver to form principally the sulfate and glucoronide conjugates which are excreted in the urine. A small fraction of an ingested dose is metabolized in the liver by isozyme CYP2E1 of the cytochrome P-450 mixed function oxidase enzyme system to form a reactive, potentially toxic, intermediate metabolite. The toxic metabolite preferentially conjugates with hepatic glutathione to form nontoxic cysteine and mercapturic acid derivatives, which are then excreted by the kidney. -

The Promise of N-Acetylcysteine in Neuropsychiatry
Review The promise of N-acetylcysteine in neuropsychiatry 1,2,3,4 5,6 1 1,2,4 Michael Berk , Gin S. Malhi , Laura J. Gray , and Olivia M. Dean 1 School of Medicine, Deakin University, Geelong, Victoria, Australia 2 Department of Psychiatry, University of Melbourne, Parkville, Victoria, Australia 3 Orygen Research Centre, Parkville, Victoria, Australia 4 The Florey Institute of Neuroscience and Mental Health, Victoria, Australia 5 Discipline of Psychiatry, Sydney Medical School, University of Sydney, Sydney, Australia 6 CADE Clinic, Department of Psychiatry, Level 5 Building 36, Royal North Shore Hospital, St Leonards, 2065, Australia N-Acetylcysteine (NAC) targets a diverse array of factors with the pathophysiology of a diverse range of neuropsy- germane to the pathophysiology of multiple neuropsy- chiatric disorders, including autism, addiction, depression, chiatric disorders including glutamatergic transmission, schizophrenia, bipolar disorder, and Alzheimer’s and Par- the antioxidant glutathione, neurotrophins, apoptosis, kinson’s diseases [3]. Determining precisely how NAC mitochondrial function, and inflammatory pathways. works is crucial both to understanding the core biology This review summarises the areas where the mecha- of these illnesses, and to opening the door to other adjunc- nisms of action of NAC overlap with known pathophysi- tive therapies operating on these pathways. The current ological elements, and offers a pre´ cis of current literature article will initially review the possible mechanisms of regarding the use of NAC in disorders including cocaine, action of NAC, and then critically appraise the evidence cannabis, and smoking addictions, Alzheimer’s and Par- that suggests it has efficacy in the treatment of neuropsy- kinson’s diseases, autism, compulsive and grooming chiatric disorders. -

Analysis of the Effects of Three Commercially Available Supplements on Performance, Exercise Induced Changes and Bio-Markers in Recreationally Trained Young Males
Analysis of the effects of three commercially available supplements on performance, exercise induced changes and bio-markers in recreationally trained young males Robert Cooper A thesis is submitted in partial fulfilment of the requirements of the University of Greenwich for the Degree of Doctor of Philosophy This research programme was carried out in collaboration with GlaxoSmithKline Maxinutrition division December 2013 School of Science University of Greenwich, Medway Campus Chatham Maritime, Kent ME4 4TB, UK i DECLARATION “I certify that this work has not been accepted in substance for any degree, and is not concurrently being submitted for any degree other than that of Doctor of Philosophy being studied at the University of Greenwich. I also declare that this work is the result of my own investigations except where otherwise identified by references and that I have not plagiarised the work of others”. Signed Date Mr Robert Cooper (Candidate) …………………………………………………………………………………………………………………………… PhD Supervisors Signed Date Dr Fernando Naclerio (1st supervisor) Signed Date Dr Mark Goss-Sampson (2nd supervisor) ii ACKNOWLEDGEMENTS Thank you to my supervisory team, Dr Fernando Naclerio, Dr Mark Goss Sampson and Dr Judith Allgrove for their support and guidance throughout my PhD. Particular thanks to Dr Fernando Naclerio for his tireless efforts, guidance and support in developing the research and my own research and communication skills. Thank you to Dr Eneko Larumbe Zabala for the statistics support. I would like to take this opportunity to thank my wonderful mother and sister who continue to give me the support and drive to succeed. Also on a personal level thank you to my amazing fiancée, Jennie Swift. -

(Acetylcysteine) Effervescent Tablets for Oral Solution Intratracheal Instillation Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION • See the Full Prescribing Information for instructions on how to use the These highlights do not include all the information needed to use nomogram to determine the need for loading and maintenance dosing. CETYLEV® safely and effectively. See full prescribing information for CETYLEV. Recommended Adult and Pediatric Dosage (2.3): • CETYLEV is for oral administration only; not for nebulization or CETYLEV (acetylcysteine) effervescent tablets for oral solution intratracheal instillation Initial U.S. Approval: 1963 • Loading dose: 140 mg/kg • Maintenance doses: 70 mg/kg repeated every 4 hours for a total of 17 ----------------------------INDICATIONS AND USAGE--------------------------- doses. CETYLEV is an antidote for acetaminophen overdose indicated to prevent or • lessen hepatic injury after ingestion of a potentially hepatotoxic quantity of See Full Prescribing Information for weight-based dosage and preparation acetaminophen in patients with acute ingestion or from repeated and administration instructions. supratherapeutic ingestion. (1) Repeated Supratherapeutic Acetaminophen Ingestion (2.4): -----------------------DOSAGE AND ADMINISTRATION----------------------- • Obtain acetaminophen concentration and other laboratory tests to guide Pre-Treatment Assessment Following Acute Ingestion (2.1): treatment; Rumack-Matthew nomogram does not apply. Obtain a plasma or serum sample to assay for acetaminophen concentration at least 4 hours after ingestion. ----------------------DOSAGE FORMS AND STRENGTHS--------------------- -

A Randomized Placebo-Controlled Trial of N-Acetylcysteine for Cannabis Use Disorder in Adults
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Drug Alcohol Manuscript Author Depend. Author Manuscript Author manuscript; available in PMC 2018 August 01. Published in final edited form as: Drug Alcohol Depend. 2017 August 01; 177: 249–257. doi:10.1016/j.drugalcdep.2017.04.020. A randomized placebo-controlled trial of N-acetylcysteine for cannabis use disorder in adults Kevin M. Graya, Susan C. Sonnea, Erin A. McClurea, Udi E. Ghitzab, Abigail G. Matthewsc, Aimee L. McRae-Clarka, Kathleen M. Carrolld, Jennifer S. Pottere, Katharina Wiestf, Larissa J. Mooneyg, Albert Hassong, Sharon L. Walshh, Michelle R. Lofwallh, Shanna Babalonish, Robert W. Lindbladc, Steven Sparenborgb,†, Aimee Wahlec, Jacqueline S. Kingc, Nathaniel L. Bakera, Rachel L. Tomkoa, Louise F. Haynesa, Ryan G. Vandreyi, and Frances R. Levinj aMedical University of South Carolina, Charleston SC bNational Institute on Drug Abuse Center for the Clinical Trials Network, Rockville MD cThe Emmes Corporation, Rockville MD dYale University, New Haven CT Correspondence: Kevin M. Gray, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, 67 President Street, MSC861, Charleston, SC USA 29425, Phone: (843) 792-6330, Fax: (843) 792-8206, [email protected]. †Retired Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. -

Treatment of Self-Poisoned Adults G
Archives of Emergency Medicine, 1985, 2, 203-208 Ipecacuanha induced emesis in the treatment of self-poisoned adults G. GORDON Accident and Emergency Department, Manor Hospital, Nuneaton, Warwickshire, England SUMMARY One hundred consecutive adult patients presenting to an Accident and Emergency Department following intentional self-poisoning were given 50 to 80 ml Paediatric Ipecacuanha Emetic Mixture BP as an emetic, together with two or three glasses of strong orange juice. A satisfactory emetic result was obtained in 99 patients. No toxic effects were noted in these patients, or in the one patient in whom emesis did not occur, and who subsequently refused gastric lavage. The potential toxicity of Ipecacuanha Syrup itself is discussed, and attention drawn to the lower Emetine content of Paediatric Ipecacuanha Emetic Mixture (BP), rather than that of the formulations used in previously published reports. The use of Paediatric Ipecacuanha Emetic Mixture B.P. in adults is effective and safe in this dosage. INTRODUCTION The methods available for retrieval of poisoning agents from the stomach are gastric lavage and emesis. In the United Kingdom at the present time, gastric lavage is the method most commonly used in the treatment of adults. It is an unpleasant and time consuming procedure for both patient and staff, and it is not without risk (Matthew et al., 1966), even in the hands of the experienced nursing staff who usually carry it out. Doubt still remains about its effectiveness (Goulding & Volans, 1977), and the basis for its use rests more on the occasional recovery of large quantities of drug, rather than verification of its routine efficiency by studies in man (Melman & Morelli, 1978). -

1 Isolation and Characterization of Cyclotides from Brazilian Psychotria
Isolation and Characterization of Cyclotides from Brazilian Psychotria: Significance in Plant Defense and Co-occurrence with Antioxidant Alkaloids Hélio N. Matsuura,† Aaron G. Poth,‡ Anna C. A. Yendo,† Arthur G. Fett-Neto,† and David J. Craik‡,* †Center for Biotechnology and Department of Botany, Federal University of Rio Grande do Sul, Porto Alegre, RS, Brazil ‡Institute for Molecular Bioscience, The University of Queensland, Brisbane, QLD, Australia. 1 ABSTRACT Plants from the genus Psychotria include species bearing cyclotides and/or alkaloids. The elucidation of factors affecting the metabolism of these molecules as well as their activities may help to understand their ecological function. In the present study, high concentrations of antioxidant indole alkaloids were found to co-occur with cyclotides in Psychotria leiocarpa and P. brachyceras. The concentrations of the major cyclotides and alkaloids in P. leiocarpa and P. brachyceras were monitored following herbivore- and pathogen-associated challenges, revealing a constitutive, phytoanticipin-like accumulation pattern. Psyleio A, the most abundant cyclotide found in the leaves of P. leiocarpa, and also found in P. brachyceras leaves, exhibited insecticidal activity against Helicoverpa armigera larvae. Addition of ethanol in the vehicle for peptide solubilization in larval feeding trials proved deleterious to insecticidal activity, and resulted in increased rates of larval survival in treatments containing indole alkaloids. This suggests that plant alkaloids ingested by larvae might contribute to herbivore oxidative stress detoxification, corroborating, in a heterologous system with artificial oxidative stress stimulation, the antioxidant efficiency of Psychotria alkaloids previously observed in planta. Overall, the present study reports data for eight novel cyclotides, the identification of P. -

Delayed Dosing of Minocycline Plus N-Acetylcysteine Reduces Neurodegeneration in Distal Brain Regions and Restores Spatial Memor
Manuscript bioRxiv preprint doi: https://doi.org/10.1101/2021.03.28.437090; this version posted March 29, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Delayed dosing of minocycline plus N-acetylcysteine reduces neurodegeneration in distal brain regions and restores spatial memory after experimental traumatic brain injury Kristen Whitney 1,2, Elena Nikulina1, Syed N. Rahman1, Alisia Alexis1 and Peter J. Bergold1,2 1Department of Physiology and Pharmacology 2Program in Neural and Behavioral Science, School of Graduate Studies State University of New York-Downstate Health Sciences University, Brooklyn NY 11215 Corresponding Author: [email protected] Department of Physiology and Pharmacology, Box 29 State University of New York – Downstate Health Sciences University 450 Clarkson Avenue Brooklyn, NY 11215 Declarations of interest: none Abbreviations: CHI- closed head injury Contra- contralateral Ipsi- ipsilateral MAP2 -microtubule associated protein 2 MINO- minocycline MN12- MINO plus NAC first dosed 12 hours after injury MN72- MINO plus NAC first dosed 72 hours after injury NAC- N-acetylcysteine TBI- Traumatic brain injury 1 bioRxiv preprint doi: https://doi.org/10.1101/2021.03.28.437090; this version posted March 29, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Abstract Multiple drugs to treat traumatic brain injury (TBI) have failed clinical trials. Most drugs lose efficacy as the time interval increases between injury and treatment onset. Insufficient therapeutic time window is a major reason underlying failure in clinical trials. -

The Alkaloid Emetine As a Promising Agent for the Induction and Enhancement of Drug-Induced Apoptosis in Leukemia Cells
737-744 26/7/07 08:26 Page 737 ONCOLOGY REPORTS 18: 737-744, 2007 737 The alkaloid emetine as a promising agent for the induction and enhancement of drug-induced apoptosis in leukemia cells MAREN MÖLLER1, KERSTIN HERZER3, TILL WENGER2,4, INGRID HERR2 and MICHAEL WINK1 1Institute of Pharmacy and Molecular Biotechnology, University of Heidelberg, Im Neuenheimer Feld 364; 2Molecular OncoSurgery, Department of Surgery, University and German Cancer Research Center, Im Neuenheimer Feld 365, 69120 Heidelberg; 31st Department of Internal Medicine, University of Mainz, Langenbeckstrasse 1, 55131 Mainz, Germany; 4Centre d'Immunologie de Marseille-Luminy, Marseille, France Received January 8, 2007; Accepted February 20, 2007 Abstract. Emetine, a natural alkaloid from Psychotria caused mainly by two isoquinoline alkaloids, emetine and ipecacuanha, has been used in phytomedicine to induce cephaeline, having identical effects regarding the irritation of vomiting, and to treat cough and severe amoebiasis. Certain the respiratory tract (1). Nowadays, ipecac syrup is no longer data suggest the induction of apoptosis by emetine in recommended for the routine use in the management of leukemia cells. Therefore, we examined the suitability of poisoned patients (2) and recently a guideline on the use of emetine for the sensitisation of leukemia cells to apoptosis ipecac syrup was published, stating that ‘the circumstances in induced by cisplatin. In response to emetine, we found a which ipecac-induced emesis is the appropriate or desired strong reduction in viability, an induction of apoptosis and method of gastric decontamination are rare’ (3). Moreover, at caspase activity comparable to the cytotoxic effect of present there is a demand to remove ipecac from the over- cisplatin. -
Minocycline Synergizes with N-Acetylcysteine and Improves Cognition and Memory Following Traumatic Brain Injury in Rats
Minocycline Synergizes with N-Acetylcysteine and Improves Cognition and Memory Following Traumatic Brain Injury in Rats Samah G. Abdel Baki, Ben Schwab, Margalit Haber, Andre´ A. Fenton, Peter J. Bergold* Departments of Physiology and Pharmacology, State University of New York-Downstate Medical Center, Brooklyn, New York, United States of America Abstract Background: There are no drugs presently available to treat traumatic brain injury (TBI). A variety of single drugs have failed clinical trials suggesting a role for drug combinations. Drug combinations acting synergistically often provide the greatest combination of potency and safety. The drugs examined (minocycline (MINO), N-acetylcysteine (NAC), simvastatin, cyclosporine A, and progesterone) had FDA-approval for uses other than TBI and limited brain injury in experimental TBI models. Methodology/Principal Findings: Drugs were dosed one hour after injury using the controlled cortical impact (CCI) TBI model in adult rats. One week later, drugs were tested for efficacy and drug combinations tested for synergy on a hierarchy of behavioral tests that included active place avoidance testing. As monotherapy, only MINO improved acquisition of the massed version of active place avoidance that required memory lasting less than two hours. MINO-treated animals, however, were impaired during the spaced version of the same avoidance task that required 24-hour memory retention. Co- administration of NAC with MINO synergistically improved spaced learning. Examination of brain histology 2 weeks after injury suggested that MINO plus NAC preserved white, but not grey matter, since lesion volume was unaffected, yet myelin loss was attenuated. When dosed 3 hours before injury, MINO plus NAC as single drugs had no effect on interleukin-1 formation; together they synergistically lowered interleukin-1 levels.