K-12 COVID-19 Requirements 2021-2022 School Year
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
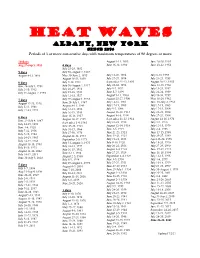
HEAT WAVES Albany, New York Since 1874 Periods of 3 Or More Consecutive Days with Maximum Temperatures of 90 Degrees Or More
HEAT WAVES Albany, New York Since 1874 Periods of 3 or more consecutive days with maximum temperatures of 90 degrees or more. 10 days August 9-11, 1893 June 26-28, 1953 Aug 27-Sep 5, 1953 4 days June 16-18, 1894 June 20-22, 1954 July 25-28, 1882 9 days July 30-August 2, 1887 August 4-12, 1896 May 30-June 2, 1895 July 18-20, 1894 July 8-10, 1955 August 18-21, 1899 July 27-29, 1894 July 21-23, 1955 8 days July 9-12, 1911 September 21-23, 1895 August 20-22, 1955 June 26-July 3, 1901 July 30-August 2, 1917 July 28-30, 1896 June 13-15, 1956 July 3-10, 1912 July 26-29, 1918 July 5-7, 1897 July 19-21, 1957 July 31-August 7, 1955 July 25-28, 1921 June 5-7, 1899 July 22-24, 1959 July 12-15, 1927 August 9-11, 1900 July 28-30, 1959 7 days July 29-August 1, 1933 August 25-27, 1900 May 18-20, 1962 July 14-16, 1901 June 30-July 2, 1963 August 17-23, 1916 June 28-July 1, 1947 July 17-19, 1905 July 17-19, 1963 July 5-11, 1988 August 8-11, 1949 July 5-7, 1908 July 17-19, 1964 July 17-23, 1991 July 12-15, 1952 August 16-18, 1913 July 21-23, 1964 July 16-19, 1953 August 8-10, 1914 July 27-29, 1964 6 days June 15-18, 1957 August 14-17, 1959 September 21-23, 1914 August 14-16, 1970 June 29-July 4, 1887 September 1-4, 1961 July 21-23, 1918 July 7-9, 1973 July 24-29, 1892 June 25-28, 1963 August 12-14, 1918 July 13-15, 1979 June 3-8, 1925 July 10-13, 1966 June 3-5, 1919 July 2-4, 1983 July 7-12, 1936 July 27-30, 1970 June 21-23, 1921 June 13-15, 1988 July 7-12, 1944 August 28-31, 1973 June 19-21, 1923 July 25-27, 1989 July 24-29, 1963 September 2-5, 1973 July -

Killing Us Softly 4 Advertising’S Image of Women
MEDIA EDUCATION FOUNDATION STUDY GUIDE Killing Us Softly 4 Advertising’s Image of Women Study Guide by Kendra Hodgson Edited by Jeremy Earp and Jason Young 2 CONTENTS Note to Educators 3 Program Overview 3 Pre-viewing Questions for Discussion & Writing 4 Key Points 5 Post-viewing Questions for Discussion & Writing 9 Assignments 11 Semester-Long Project 14 For additional assignments, please download the Killing Us Softly 3 study guide: http://www.mediaed.org/assets/products/206/studyguide_206.pdf For handouts associated with the Killing Us Softly 3 study guide, also download: http://www.mediaed.org/assets/products/206/studyguidehandout_206.pdf © The Media Education Foundation | www.mediaed.org 3 NOTE TO EDUCATORS This study guide is designed to help you and your students engage and manage the information presented in this video. Given that it can be difficult to teach visual content – and difficult for students to recall detailed information from videos after viewing them – the intention here is to give you a tool to help your students slow down and deepen their thinking about the specific issues this video addresses. With this in mind, we’ve structured the guide to help you stay close to the video’s main line of argument as it unfolds: Key Points provide a concise and comprehensive summary of the video. They are designed to make it easier for you and your students to recall the details of the video during class discussions, and as a reference point for students as they work on assignments. Questions for Discussion & Writing encourage students to reflect critically on the video during class discussions, and guide their written reactions before and after these discussions. -

Speech Sound Programme for 'K' / 'C' at the Start of Words
Speech Sound Programme for ‘k’ / ‘c’ at the start of words This programme is for children who are producing a ‘t’ sound in place of a ‘k’ / ‘c’ sound at the start of words. For example, ‘cat’ is produced ‘tat’ and ‘cup’ is produced ‘tup’. ‘k’ is the target sound. ‘t’ is the produced sound. Below are a set of stages to work through with the child. Start with Stage 1 and only move up to the next stage when you are confident that the child has achieved the current stage. It is recommended that the programme is carried out for 15 minutes three times a week. If you would like any advice or you feel that the child is not making progress, please contact the Speech and Language Therapy team on 0151 514 2334. Stage 1 - Listening for the target sound 1. See ‘Picture Set 1’ for sound cue pictures that represent the target sound ‘k’ and the produced sound ‘t’. 2. Place the two pictures (‘k’ and ‘t’) in front of the child. 3. Teach the child the sounds, not the letter names, e.g., say ‘k’ and not ‘k-uh’. 4. Say the two sounds at random and ask the child to point or place a counter on which sound they hear. 5. Repeat this activity a number of times until you are sure the child can consistently hear the difference between the two sounds. Stage 2 - Sorting pictures by their first sound. 1. Now that the child can hear the difference between the two sounds (‘k’ and ‘t’) on their own, try the same with words. -

The Perfect Sacrifice Lesson Focus | Since His Beginning, Man Has Always Offered Sacrifices to God in Order to Atone for His Sins
St. Mary's At-Home Guide - February 24 (Ch 20-21) - Grade 5 Lesson 20 The Perfect Sacrifice Lesson Focus | Since his beginning, man has always offered sacrifices to God in order to atone for his sins. No sacrifice, however, could truly atone for sin because no sacrifice was perfect. Jesus’ offering of himself on the Cross, however, was. That’s because Jesus, who both offered the sacrifice and was the sacrifice, was perfect. At every Mass, Jesus, through the priest, continues to offer himself to God when the bread and wine are transformed into his Body and Blood. It is the same sacrifice offered on Calvary, re–presented in time. 1 | begin Pray the Glory Be with your child. Show your child pictures of sheep, goats, calves, doves, wheat, and wine. Explain that if you had lived in Jerusalem during Jesus’ time, your family would have gone to the temple to give these items to the priest for sacrifice. Together read John 1:19–30 aloud. 2 | summarize Summarize this week’s lesson for your child: Example: When Jesus offered his life on the Cross, he became the one, perfect sacrifice, the Lamb of God offered up for all the world’s sins. After that, it was no longer necessary for people to offer up other ritual sacrifices, such as goats, lambs, and doves. 3 | review References Review this week’s lesson by asking your child the following questions: Student Textbook: 1. What is a sacrifice? (The offering up of something to God.) Chapter 20, pp. 83–86 2. -

Changes in the Risk of Stroke in Dialysis Patients: a Retrospective Analysis Over the Last 40 Years
toxins Article Changes in the Risk of Stroke in Dialysis Patients: A Retrospective Analysis over the Last 40 Years Toshiya Aono 1,†, Yuki Shinya 1,2,*,† , Satoru Miyawaki 2 , Takehiro Sugiyama 3,4, Isao Kumagai 5, Atsumi Takenobu 1, Masahiro Shin 2 , Nobuhito Saito 2 and Akira Teraoka 1 1 Department of Neurosurgery, Teraoka Memorial Hospital, Hiroshima 729-3103, Japan; [email protected] (T.A.); [email protected] (A.T.); [email protected] (A.T.) 2 Department of Neurosurgery, The University of Tokyo Hospital, Tokyo 113-8655, Japan; [email protected] (S.M.); [email protected] (M.S.); [email protected] (N.S.) 3 Diabetes and Metabolism Information Center, Research Institute, National Center for Global Health and Medicine, Tokyo 162-8655, Japan; [email protected] 4 Department of Health Services Research, Faculty of Medicine, University of Tsukuba, Ibaraki 305-8575, Japan 5 Department of Nephrology, Teraoka Memorial Hospital, Hiroshima 729-3103, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-3-5800-8853 † These two authors have contributed equally to this study and are thus co-first authors. Abstract: The stroke incidence in hemodialysis (HD) patients is high, but the associated factors remain largely unknown. This study aimed to analyze stroke incidence in HD patients and changes in risk factors. Data of 291 patients were retrospectively analyzed. The cumulative stroke incidences were 21.6% at 10 years and 31.5% at 20. Diabetic nephropathy (DN) significantly increased overall stroke (hazard ratio (HR), 2.24; 95% confidence interval (CI), 1.21–4.12; p = 0.001) and ischemic p stroke (HR, 2.16; 95% CI, 1.00–4.64; = 0.049). -

2021-2022 Custom & Standard Information Due Dates
2021-2022 CUSTOM & STANDARD INFORMATION DUE DATES Desired Cover All Desired Cover All Delivery Date Info. Due Text Due Delivery Date Info. Due Text Due May 31 No Deliveries No Deliveries July 19 April 12 May 10 June 1 February 23 March 23 July 20 April 13 May 11 June 2 February 24 March 24 July 21 April 14 May 12 June 3 February 25 March 25 July 22 April 15 May 13 June 4 February 26 March 26 July 23 April 16 May 14 June 7 March 1 March 29 July 26 April 19 May 17 June 8 March 2 March 30 July 27 April 20 May 18 June 9 March 3 March 31 July 28 April 21 May 19 June 10 March 4 April 1 July 29 April 22 May 20 June 11 March 5 April 2 July 30 April 23 May 21 June 14 March 8 April 5 August 2 April 26 May 24 June 15 March 9 April 6 August 3 April 27 May 25 June 16 March 10 April 7 August 4 April 28 May 26 June 17 March 11 April 8 August 5 April 29 May 27 June 18 March 12 April 9 August 6 April 30 May 28 June 21 March 15 April 12 August 9 May 3 May 28 June 22 March 16 April 13 August 10 May 4 June 1 June 23 March 17 April 14 August 11 May 5 June 2 June 24 March 18 April 15 August 12 May 6 June 3 June 25 March 19 April 16 August 13 May 7 June 4 June 28 March 22 April 19 August 16 May 10 June 7 June 29 March 23 April 20 August 17 May 11 June 8 June 30 March 24 April 21 August 18 May 12 June 9 July 1 March 25 April 22 August 19 May 13 June 10 July 2 March 26 April 23 August 20 May 14 June 11 July 5 March 29 April 26 August 23 May 17 June 14 July 6 March 30 April 27 August 24 May 18 June 15 July 7 March 31 April 28 August 25 May 19 June 16 July 8 April 1 April 29 August 26 May 20 June 17 July 9 April 2 April 30 August 27 May 21 June 18 July 12 April 5 May 3 August 30 May 24 June 21 July 13 April 6 May 4 August 31 May 25 June 22 July 14 April 7 May 5 September 1 May 26 June 23 July 15 April 8 May 6 September 2 May 27 June 24 July 16 April 9 May 7 September 3 May 28 June 25. -

9/11 Report”), July 2, 2004, Pp
Final FM.1pp 7/17/04 5:25 PM Page i THE 9/11 COMMISSION REPORT Final FM.1pp 7/17/04 5:25 PM Page v CONTENTS List of Illustrations and Tables ix Member List xi Staff List xiii–xiv Preface xv 1. “WE HAVE SOME PLANES” 1 1.1 Inside the Four Flights 1 1.2 Improvising a Homeland Defense 14 1.3 National Crisis Management 35 2. THE FOUNDATION OF THE NEW TERRORISM 47 2.1 A Declaration of War 47 2.2 Bin Ladin’s Appeal in the Islamic World 48 2.3 The Rise of Bin Ladin and al Qaeda (1988–1992) 55 2.4 Building an Organization, Declaring War on the United States (1992–1996) 59 2.5 Al Qaeda’s Renewal in Afghanistan (1996–1998) 63 3. COUNTERTERRORISM EVOLVES 71 3.1 From the Old Terrorism to the New: The First World Trade Center Bombing 71 3.2 Adaptation—and Nonadaptation— ...in the Law Enforcement Community 73 3.3 . and in the Federal Aviation Administration 82 3.4 . and in the Intelligence Community 86 v Final FM.1pp 7/17/04 5:25 PM Page vi 3.5 . and in the State Department and the Defense Department 93 3.6 . and in the White House 98 3.7 . and in the Congress 102 4. RESPONSES TO AL QAEDA’S INITIAL ASSAULTS 108 4.1 Before the Bombings in Kenya and Tanzania 108 4.2 Crisis:August 1998 115 4.3 Diplomacy 121 4.4 Covert Action 126 4.5 Searching for Fresh Options 134 5. -

August 11, 2020 in This Issue
August 11, 2020 Dear Colleagues, A handful of Louisiana systems welcomed students back last week. This week, more systems are reopening their doors to children. As we learned during a call with system leaders this past Friday, schools reopened last week without any major disruptions. Medical professionals from the Louisiana Department of Health and Ochsner joined us on the call. They were complimentary of the steps educators are taking to mitigate the spread of COVID-19. There will be challenges as you begin the school year. If COVID-19 is present in your community, it will likely be present in your schools. You developed a fluid reopening plan to guide you through these challenges. Follow your plan, continue to communicate with stakeholders and keep student and employee safety at the center of your decisions. Most systems are reopening under a hybrid model that combines in-person and distance learning. This week we are releasing a tool that highlights best practices in virtual instruction. Nothing will fully replace the instruction and engagement students receive from a quality teacher in the classroom. With more time to plan and with the support of the Department, I’m confident virtual instruction will take a large step forward for our students and families this fall. These resources will be available on our Strong Start page Wednesday. We’ve also updated our Strong Start resources for students with disabilities. The newest set of resources includes guidance for families, educators and direct service providers. School may look different this year, but our commitment to families and students remains steadfast. -

2021 7 Day Working Days Calendar
2021 7 Day Working Days Calendar The Working Day Calendar is used to compute the estimated completion date of a contract. To use the calendar, find the start date of the contract, add the working days to the number of the calendar date (a number from 1 to 1000), and subtract 1, find that calculated number in the calendar and that will be the completion date of the contract Date Number of the Calendar Date Friday, January 1, 2021 133 Saturday, January 2, 2021 134 Sunday, January 3, 2021 135 Monday, January 4, 2021 136 Tuesday, January 5, 2021 137 Wednesday, January 6, 2021 138 Thursday, January 7, 2021 139 Friday, January 8, 2021 140 Saturday, January 9, 2021 141 Sunday, January 10, 2021 142 Monday, January 11, 2021 143 Tuesday, January 12, 2021 144 Wednesday, January 13, 2021 145 Thursday, January 14, 2021 146 Friday, January 15, 2021 147 Saturday, January 16, 2021 148 Sunday, January 17, 2021 149 Monday, January 18, 2021 150 Tuesday, January 19, 2021 151 Wednesday, January 20, 2021 152 Thursday, January 21, 2021 153 Friday, January 22, 2021 154 Saturday, January 23, 2021 155 Sunday, January 24, 2021 156 Monday, January 25, 2021 157 Tuesday, January 26, 2021 158 Wednesday, January 27, 2021 159 Thursday, January 28, 2021 160 Friday, January 29, 2021 161 Saturday, January 30, 2021 162 Sunday, January 31, 2021 163 Monday, February 1, 2021 164 Tuesday, February 2, 2021 165 Wednesday, February 3, 2021 166 Thursday, February 4, 2021 167 Date Number of the Calendar Date Friday, February 5, 2021 168 Saturday, February 6, 2021 169 Sunday, February -

From Address to the Second National Congress of Venezuela
from A DDRESS TO THE SECOND NATIONAL CONGRESS OF VENEZUELA 1819 Simón Bolívar Venezuela declared its independence from Spain in 1811, but then had to fight to win it. The war against Spain lasted for ten long years. During this time Venezuela struggled to create its own government. The following excerpt comes from a speech by Simón Bolívar, the great military and political hero of South American liberation. Bolívar argues that Venezuela must shape a government suited to its own special nature, rather than mimic the United States government. THINK THROUGH HISTORY: Recognizing Bias What was Bolívar’s viewpoint toward the majority of the people of Latin America? Why does he caution against a government of too much freedom and responsibility? Subject to the threefold yoke of ignorance, tyranny, and vice, the American peo- ple1 have been unable to acquire knowledge, power, or [civic] virtue. The lessons we received and the models we studied, as pupils of such pernicious teachers, were most destructive. We have been ruled more by deceit than by force, and we have been degraded more by vice than by superstition. Slavery is the daughter of Darkness: an ignorant people is a blind instrument of its own destruction. Ambition and intrigue abuse the credulity and experience of men lacking all politi- cal, economic, and civic knowledge; they adopt pure illusion as reality; they take license for liberty, treachery for patriotism, and vengeance for justice. This situa- tion is similar to that of the robust blind man who, beguiled by his strength, strides forward with all the assurance of one who can see, but, upon hitting every variety of obstacle, finds himself unable to retrace his steps. -
![Chemical Kinetics [A][B] [D] [C] [A][B] [B] [A] K R Dt D Dt D K R Dt D Dt D](https://docslib.b-cdn.net/cover/8501/chemical-kinetics-a-b-d-c-a-b-b-a-k-r-dt-d-dt-d-k-r-dt-d-dt-d-948501.webp)
Chemical Kinetics [A][B] [D] [C] [A][B] [B] [A] K R Dt D Dt D K R Dt D Dt D
Chemical kinetics (Nazaroff & Alvarez-Cohen, Section 3.A.2) This is the answer to what happens when chemical equilibrium is not reached. For example, take the two-way reaction A + B ↔ C + D As A and B come into contact with each other, they start to react with each other, and the reaction rate can be expressed as Rforward = kf [A] [B]. This expression reflects the fact that the more of A and B there is, the more encounters occur, and the more reactions take place. This rate depletes the amounts of both A and B, and generates amounts of C and D: d[A] d[B] R k [A][B] dt dt forward f d[C] d[D] R k [A][B] dt dt forward f But, at the same time, C and D come in contact, too, and carry their own, reverse reaction, at a rate proportional to their amounts Rreverse = kr [C] [D] . This rate depletes the amounts of both C and D, and adds to the amounts of A and B: d[A] d[B] R k [C][D] dt dt reverse r d[C] d[D] R k [C][D] dt dt reverse r Because the two reactions occur simultaneously, we subtract the rate of one from the other: d[A] d[B] R R k [A][B] k [C][D] dt dt forward reverse f r d[C] d[D] R R k [A][B] k [C][D] dt dt forward reverse f r 1 Finally, in a system with open boundaries, we can add the imports and exports: d[A] V Qin [A]in Qout [A]out krV[C][D] kfV[A][B] dt inlets outlets d[B] V Qin [B]in Qout [B]out krV[C][D] kfV[A][B] dt inlets outlets d[C] V Qin [C]in Qout [C]out kfV[A][B] krV[C][D] dt inlets outlets d[D] V Qin [D]in Qout [D]out kfV[A][B] krV[C][D] dt inlets outlets imports exports sources sinks where V is the volume of the system for which the budget is written. -

College Comeback: ODHE Formal Guidance
College Comeback A Summary of Ohio Law and Policy on Outstanding Student Balances Owed and Debt-Forgiveness Models that Can Be Applied in Ohio Approximately 1.5 million Ohioans have some college, but no degree (or credential). This presents a critical challenge to maximizing the economic opportunity for that individual as well as for the greater good of the State of Ohio’s economy. These students enrolled in post-secondary education seeking a degree, but we didn’t get them across the finish line. If we successfully help Ohioans enjoy a “college comeback” resulting in a degree (or credential), we can make significant strides toward increasing Ohio’s educational attainment, improving expected gross domestic product, average wages, employment rate and Ohio’s economy. Among the barriers to a college comeback for this population are past-due debts owed to institutions of higher education at which they were previously enrolled, nearly always resulting in an inability to receive a transcript to complete college elsewhere. Facing these barriers, many students opt never to return and complete their degree. In recent years, some institutions of higher education – notably Cleveland State University, Clark State College, Lorain County Community College, Stark State College, and Zane State College right here in Ohio – have begun to offer new debt forgiveness programs. Cleveland State is currently offering up to $5,000 in debt forgiveness – among the best offers we’ve seen nationally. Lorain and Clark State are both offering up to $1,000 in debt relief. A national example is Wayne State University in Detroit. The “Warrior Way Back” program forgives up to $1,500.