Differential Mechanisms of Bicalutamide-Induced Apoptosis in Prostate Cell Lines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
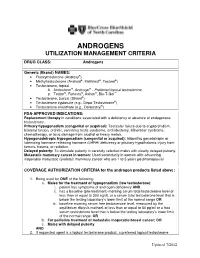
Androgens Utilization Management Criteria
ANDROGENS UTILIZATION MANAGEMENT CRITERIA DRUG CLASS: Androgens Generic (Brand) NAMES: • Fluoxymesterone (Androxy®) • Methyltestosterone (Android®, Methitest®, Testred®) • Testosterone, topical A. Androderm®, Androgel® - Preferred topical testosterone ® ® ® ™ B. Testim , Fortesta , Axiron , Bio-T-Gel • Testosterone, buccal (Striant®) • Testosterone cypionate (e.g., Depo-Testosterone®) • Testosterone enanthate (e.g., Delatestryl®) FDA-APPROVED INDICATIONS: Replacement therapy in conditions associated with a deficiency or absence of endogenous testosterone. Primary hypogonadism (congenital or acquired): Testicular failure due to cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchidectomy, Klinefelter syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. Hypogonadotropic hypogonadism (congenital or acquired): Idiopathic gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. Delayed puberty: To stimulate puberty in carefully selected males with clearly delayed puberty. Metastatic mammary cancer in women: Used secondarily in women with advancing inoperable metastatic (skeletal) mammary cancer who are 1 to 5 years postmenopausal COVERAGE AUTHORIZATION CRITERIA for the androgen products listed above: 1. Being used for ONE of the following: a. Males for the treatment of hypogonadism (low testosterone): i. patient has symptoms of androgen deficiency AND ii. has a baseline (pre-treatment) morning serum total testosterone level of less than or equal to 300 ng/dL or a serum total testosterone level that is below the testing laboratory’s lower limit of the normal range OR iii. baseline morning serum free testosterone level, measured by the equilibrium dialysis method, of less than or equal to 50 pg/ml or a free serum testosterone level that is below the testing laboratory’s lower limit of the normal range, OR b. -

CASODEX (Bicalutamide)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gynecomastia and breast pain have been reported during treatment with These highlights do not include all the information needed to use CASODEX 150 mg when used as a single agent. (5.3) CASODEX® safely and effectively. See full prescribing information for • CASODEX is used in combination with an LHRH agonist. LHRH CASODEX. agonists have been shown to cause a reduction in glucose tolerance in CASODEX® (bicalutamide) tablet, for oral use males. Consideration should be given to monitoring blood glucose in Initial U.S. Approval: 1995 patients receiving CASODEX in combination with LHRH agonists. (5.4) -------------------------- RECENT MAJOR CHANGES -------------------------- • Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate Warnings and Precautions (5.2) 10/2017 for clinical progression if PSA increases. (5.5) --------------------------- INDICATIONS AND USAGE -------------------------- ------------------------------ ADVERSE REACTIONS ----------------------------- • CASODEX 50 mg is an androgen receptor inhibitor indicated for use in Adverse reactions that occurred in more than 10% of patients receiving combination therapy with a luteinizing hormone-releasing hormone CASODEX plus an LHRH-A were: hot flashes, pain (including general, back, (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral the prostate. (1) edema, dyspnea, diarrhea, hematuria, nocturia, and anemia. (6.1) • CASODEX 150 mg daily is not approved for use alone or with other treatments. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION ---------------------- www.fda.gov/medwatch The recommended dose for CASODEX therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). -

Health Risks Associated with Long-Term Finasteride and Dutasteride Use: It’S Time to Sound the Alarm
Review Article Health promotion, disease prevention, and lifestyle pISSN: 2287-4208 / eISSN: 2287-4690 World J Mens Health 2020 Jul 38(3): 323-337 https://doi.org/10.5534/wjmh.200012 Health Risks Associated with Long-Term Finasteride and Dutasteride Use: It’s Time to Sound the Alarm Abdulmaged M. Traish Department of Urology, Boston University School of Medicine, Boston, MA, USA 5α-dihydrotestosterone (5α-DHT) is the most potent natural androgen. 5α-DHT elicits a multitude of physiological actions, in a host of tissues, including prostate, seminal vesicles, hair follicles, skin, kidney, and lacrimal and meibomian glands. How- ever, the physiological role of 5α-DHT in human physiology, remains questionable and, at best, poorly appreciated. Recent emerging literature supports a role for 5α-DHT in the physiological function of liver, pancreatic β-cell function and survival, ocular function and prevention of dry eye disease and kidney physiological function. Thus, inhibition of 5α-reductases with finasteride or dutasteride to reduce 5α-DHT biosynthesis in the course of treatment of benign prostatic hyperplasia (BPH) or male pattern hair loss, known as androgenetic alopecia (AGA) my induces a novel form of tissue specific androgen deficien- cy and contributes to a host of pathophysiological conditions, that are yet to be fully recognized. Here, we advance the con- cept that blockade of 5α-reductases by finasteride or dutasteride in a mechanism-based, irreversible, inhabitation of 5α-DHT biosynthesis results in a novel state of androgen deficiency, independent of circulating testosterone levels. Finasteride and dutasteride are frequently prescribed for long-term treatment of lower urinary tract symptoms in men with BPH and in men with AGA. -

COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone During SARS-Cov-2 Infection
pharmaceuticals Review COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone during SARS-CoV-2 Infection Katarzyna Kotfis 1,* , Kacper Lechowicz 1 , Sylwester Drozd˙ zal˙ 2 , Paulina Nied´zwiedzka-Rystwej 3 , Tomasz K. Wojdacz 4, Ewelina Grywalska 5 , Jowita Biernawska 6, Magda Wi´sniewska 7 and Miłosz Parczewski 8 1 Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University in Szczecin, 70-111 Szczecin, Poland; [email protected] 2 Department of Pharmacokinetics and Monitored Therapy, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 3 Institute of Biology, University of Szczecin, 71-412 Szczecin, Poland; [email protected] 4 Independent Clinical Epigenetics Laboratory, Pomeranian Medical University, 71-252 Szczecin, Poland; [email protected] 5 Department of Clinical Immunology and Immunotherapy, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 6 Department of Anesthesiology and Intensive Therapy, Pomeranian Medical University in Szczecin, 71-252 Szczecin, Poland; [email protected] 7 Clinical Department of Nephrology, Transplantology and Internal Medicine, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 8 Department of Infectious, Tropical Diseases and Immune Deficiency, Pomeranian Medical University in Szczecin, 71-455 Szczecin, Poland; [email protected] * Correspondence: katarzyna.kotfi[email protected]; Tel.: +48-91-466-11-44 Abstract: In March 2020, coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2 was declared Citation: Kotfis, K.; Lechowicz, K.; a global pandemic by the World Health Organization (WHO). The clinical course of the disease is Drozd˙ zal,˙ S.; Nied´zwiedzka-Rystwej, unpredictable but may lead to severe acute respiratory infection (SARI) and pneumonia leading to P.; Wojdacz, T.K.; Grywalska, E.; acute respiratory distress syndrome (ARDS). -

Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals
Journal of Clinical Medicine Review Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals Carlotta Cocchetti 1, Jiska Ristori 1, Alessia Romani 1, Mario Maggi 2 and Alessandra Daphne Fisher 1,* 1 Andrology, Women’s Endocrinology and Gender Incongruence Unit, Florence University Hospital, 50139 Florence, Italy; [email protected] (C.C); jiska.ristori@unifi.it (J.R.); [email protected] (A.R.) 2 Department of Experimental, Clinical and Biomedical Sciences, Careggi University Hospital, 50139 Florence, Italy; [email protected]fi.it * Correspondence: fi[email protected] Received: 16 April 2020; Accepted: 18 May 2020; Published: 26 May 2020 Abstract: Introduction: To date no standardized hormonal treatment protocols for non-binary transgender individuals have been described in the literature and there is a lack of data regarding their efficacy and safety. Objectives: To suggest possible treatment strategies for non-binary transgender individuals with non-standardized requests and to emphasize the importance of a personalized clinical approach. Methods: A narrative review of pertinent literature on gender-affirming hormonal treatment in transgender persons was performed using PubMed. Results: New hormonal treatment regimens outside those reported in current guidelines should be considered for non-binary transgender individuals, in order to improve psychological well-being and quality of life. In the present review we suggested the use of hormonal and non-hormonal compounds, which—based on their mechanism of action—could be used in these cases depending on clients’ requests. Conclusion: Requests for an individualized hormonal treatment in non-binary transgender individuals represent a future challenge for professionals managing transgender health care. For each case, clinicians should balance the benefits and risks of a personalized non-standardized treatment, actively involving the person in decisions regarding hormonal treatment. -

Finasteride Adverse Effects and Post-Finasteride Syndrome
Journal of Mind and Medical Sciences Volume 3 | Issue 1 Article 9 2016 Finasteride adverse effects and post-finasteride syndrome; implications for dentists Stana Paunica Carol Davila University, Faculty of Dental Medicine, Department of Periodontology, [email protected] Marina Giurgiu Carol Davila University, Faculty of Dental Medicine, Department of Periodontology Andrei Vasilache Carol Davila University, Faculty of Dental Medicine, Department of Periodontology Ioana Paunica Carol Davila University, Faculty of General Medicine Ion Motofei Carol Davila University, Faculty of General Medicine See next page for additional authors Follow this and additional works at: http://scholar.valpo.edu/jmms Part of the Oral Biology and Oral Pathology Commons, and the Periodontics and Periodontology Commons Recommended Citation Paunica, Stana; Giurgiu, Marina; Vasilache, Andrei; Paunica, Ioana; Motofei, Ion; Vasilache, Adriana; Dumitriu, Horia Traian; and Dumitriu, Anca Silvia (2016) "Finasteride adverse effects and post-finasteride syndrome; implications for dentists," Journal of Mind and Medical Sciences: Vol. 3 : Iss. 1 , Article 9. Available at: http://scholar.valpo.edu/jmms/vol3/iss1/9 This Research Article is brought to you for free and open access by ValpoScholar. It has been accepted for inclusion in Journal of Mind and Medical Sciences by an authorized administrator of ValpoScholar. For more information, please contact a ValpoScholar staff member at [email protected]. Finasteride adverse effects and post-finasteride syndrome; implications for dentists Authors Stana Paunica, Marina Giurgiu, Andrei Vasilache, Ioana Paunica, Ion Motofei, Adriana Vasilache, Horia Traian Dumitriu, and Anca Silvia Dumitriu This research article is available in Journal of Mind and Medical Sciences: http://scholar.valpo.edu/jmms/vol3/iss1/9 J Mind Med Sci. -

Gender-Affirming Hormone Therapy
GENDER-AFFIRMING HORMONE THERAPY Julie Thompson, PA-C Medical Director of Trans Health, Fenway Health March 2020 fenwayhealth.org GOALS AND OBJECTIVES 1. Review process of initiating hormone therapy through the informed consent model 2. Provide an overview of masculinizing and feminizing hormone therapy 3. Review realistic expectations and benefits of hormone therapy vs their associated risks 4. Discuss recommendations for monitoring fenwayhealth.org PROTOCOLS AND STANDARDS OF CARE fenwayhealth.org WPATH STANDARDS OF CARE, 2011 The criteria for hormone therapy are as follows: 1. Well-documented, persistent (at least 6mo) gender dysphoria 2. Capacity to make a fully informed decision and to consent for treatment 3. Age of majority in a given country 4. If significant medical or mental health concerns are present, they must be reasonably well controlled fenwayhealth.org INFORMED CONSENT MODEL ▪ Requires healthcare provider to ▪ Effectively communicate benefits, risks and alternatives of treatment to patient ▪ Assess that the patient is able to understand and consent to the treatment ▪ Informed consent model does not preclude mental health care! ▪ Recognizes that prescribing decision ultimately rests with clinical judgment of provider working together with the patient ▪ Recognizes patient autonomy and empowers self-agency ▪ Decreases barriers to medically necessary care fenwayhealth.org INITIAL VISITS ▪ Review history of gender experience and patient’s goals ▪ Document prior hormone use ▪ Assess appropriateness for gender affirming medical -

Adverse Effects of Anabolic-Androgenic Steroids: a Literature Review
healthcare Review Adverse Effects of Anabolic-Androgenic Steroids: A Literature Review Giuseppe Davide Albano 1,†, Francesco Amico 1,†, Giuseppe Cocimano 1, Aldo Liberto 1, Francesca Maglietta 2, Massimiliano Esposito 1, Giuseppe Li Rosi 3, Nunzio Di Nunno 4, Monica Salerno 1,‡ and Angelo Montana 1,*,‡ 1 Legal Medicine, Department of Medical, Surgical and Advanced Technologies, “G.F. Ingrassia”, University of Catania, 95123 Catania, Italy; [email protected] (G.D.A.); [email protected] (F.A.); [email protected] (G.C.); [email protected] (A.L.); [email protected] (M.E.); [email protected] (M.S.) 2 Department of Clinical and Experimental Medicine, University of Foggia, 71122 Foggia, Italy; [email protected] 3 Department of Law, Criminology, Magna Graecia University of Catanzaro, 88100 Catanzaro, Italy; [email protected] 4 Department of History, Society and Studies on Humanity, University of Salento, 73100 Lecce, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-095-3782153 † These authors contributed equally to this work. ‡ These authors share last authorship. Abstract: Anabolic-androgenic steroids (AASs) are a large group of molecules including endoge- nously produced androgens, such as testosterone, as well as synthetically manufactured derivatives. AAS use is widespread due to their ability to improve muscle growth for aesthetic purposes and athletes’ performance, minimizing androgenic effects. AAS use is very popular and 1–3% of US inhabitants have been estimated to be AAS users. However, AASs have side effects, involving all organs, tissues and body functions, especially long-term toxicity involving the cardiovascular system Citation: Albano, G.D.; Amico, F.; and the reproductive system, thereby, their abuse is considered a public health issue. -

Steroid Sulfatase Stimulates Intracrine Androgen Synthesis and Is a Therapeutic Target for Advanced Prostate Cancer
Author Manuscript Published OnlineFirst on September 14, 2020; DOI: 10.1158/1078-0432.CCR-20-1682 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Steroid sulfatase stimulates intracrine androgen synthesis and is a therapeutic target for advanced prostate cancer Cameron M. Armstrong1*, Chengfei Liu1*, Liangren Liu1,2*, Joy C. Yang1, Wei Lou1, Ruining Zhao1,3, Shu Ning1, Alan P. Lombard1, Jinge Zhao1, Leandro S D'Abronzo1, Christopher P. Evans1,4, Pui-Kai Li5, Allen C. Gao1, 4, 6,7 Running title: Targeting steroid sulfatase for advanced prostate cancer Key words: Prostate cancer, steroid sulfatase, resistance, intracrine androgen synthesis, adrenal androgens 1Department of Urologic Surgery, University of California Davis, CA, USA 2Present address: Department of Urology, West China Hospital, Sichuan University, China 3Present address: Department of Urology, General Hospital of Ningxia Medical University, China 4UC Davis Comprehensive Cancer Center, University of California Davis, CA, USA 5Division of Medicinal Chemistry and Pharmacognosy, College of Pharmacy, The Ohio State University, Columbus, OH, USA 6VA Northern California Health Care System, Sacramento, CA, USA 7Corresponding author: Allen Gao, University of California Davis, 4645 2nd Avenue, Sacramento, CA 95817, USA. Phone: 916-734-8718, email: [email protected] *These authors contributed equally to the work. Conflict of interest: PKL and ACG are co-inventors of a patent application of the selected small molecule inhibitors of steroid sulfatase. 1 Downloaded from clincancerres.aacrjournals.org on October 1, 2021. © 2020 American Association for Cancer Research. Author Manuscript Published OnlineFirst on September 14, 2020; DOI: 10.1158/1078-0432.CCR-20-1682 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. -

Steroids and Other Appearance and Performance Enhancing Drugs (Apeds) Research Report
Research Report Revised Febrero 2018 Steroids and Other Appearance and Performance Enhancing Drugs (APEDs) Research Report Table of Contents Steroids and Other Appearance and Performance Enhancing Drugs (APEDs) Research Report Introduction What are the different types of APEDs? What is the history of anabolic steroid use? Who uses anabolic steroids? Why are anabolic steroids misused? How are anabolic steroids used? What are the side effects of anabolic steroid misuse? How does anabolic steroid misuse affect behavior? What are the risks of anabolic steroid use in teens? How do anabolic steroids work in the brain? Are anabolic steroids addictive? How are anabolic steroids tested in athletes? What can be done to prevent steroid misuse? What treatments are effective for anabolic steroid misuse? Where can I get further information about steroids? References Page 1 Steroids and Other Appearance and Performance Enhancing Drugs (APEDs) Research Report Esta publicación está disponible para su uso y puede ser reproducida, en su totalidad, sin pedir autorización al NIDA. Se agradece la citación de la fuente, de la siguiente manera: Fuente: Instituto Nacional sobre el Abuso de Drogas; Institutos Nacionales de la Salud; Departamento de Salud y Servicios Humanos de los Estados Unidos. Introduction Appearance and performance enhancing drugs (APEDs) are most often used by males to improve appearance by building muscle mass or to enhance athletic performance. Although they may directly and indirectly have effects on a user’s mood, they do not produce a euphoric high, which makes APEDs distinct from other drugs such as cocaine, heroin, and marijuana. However, users may develop a substance use disorder, defined as continued use despite adverse consequences. -

Androgenic Alopecia; the Risk–Benefit Ar Tio of Finasteride David L
Journal of Mind and Medical Sciences Volume 5 | Issue 1 Article 2 2018 Androgenic alopecia; the risk–benefit ar tio of Finasteride David L. Rowland Valparaiso University, Department of Psychology, Valparaiso, [email protected] Ion G. Motofei Carol Davila University of Medicine and Pharmacy, Faculty of General Medicine, [email protected] Ioana Păunică Carol Davila University of Medicine and Pharmacy, Faculty of General Medicine Petrișor Banu Carol Davila University of Medicine and Pharmacy, Faculty of General Medicine Mihaela F. Nistor Carol Davila University of Medicine and Pharmacy, Faculty of General Medicine See next page for additional authors Follow this and additional works at: https://scholar.valpo.edu/jmms Part of the Dermatology Commons, Endocrine System Diseases Commons, Integrative Medicine Commons, and the Skin and Connective Tissue Diseases Commons Recommended Citation Rowland, David L.; Motofei, Ion G.; Păunică, Ioana; Banu, Petrișor; Nistor, Mihaela F.; Păunică, Stana; and Constantin, Vlad D. (2018) "Androgenic alopecia; the risk–benefit ar tio of Finasteride," Journal of Mind and Medical Sciences: Vol. 5 : Iss. 1 , Article 2. DOI: 10.22543/7674.51.P16 Available at: https://scholar.valpo.edu/jmms/vol5/iss1/2 This Review Article is brought to you for free and open access by ValpoScholar. It has been accepted for inclusion in Journal of Mind and Medical Sciences by an authorized administrator of ValpoScholar. For more information, please contact a ValpoScholar staff member at [email protected]. Androgenic alopecia; the risk–benefit ar tio of Finasteride Authors David L. Rowland, Ion G. Motofei, Ioana Păunică, Petrișor Banu, Mihaela F. Nistor, Stana Păunică, and Vlad D. -

Risk of Depression After 5 Alpha Reductase Inhibitor Medication: Meta-Analysis
Original Article Prostate and male voiding dysfunctions pISSN: 2287-4208 / eISSN: 2287-4690 World J Mens Health Published online May 23, 2019 https://doi.org/10.5534/wjmh.190046 Risk of Depression after 5 Alpha Reductase Inhibitor Medication: Meta-Analysis Jae Heon Kim1,2 , Sung Ryul Shim3,4 , Yash Khandwala1 , Francesco Del Giudice5 , Simon Sorensen6 , Benjamin I. Chung1 1Department of Urology, Stanford University Medical Center, Stanford, CA, USA, 2Department of Urology and 3Urological Biomedicine Research Institute, Soonchunhyang University Seoul Hospital, Soon Chun Hyang University College of Medicine, Seoul, 4Department of Preventive Medicine, Korea University College of Medicine, Seoul, Korea, 5Department of Urology, Sapienza University of Rome, Rome, Italy, 6Department of Urology, Aarhus University Hospital, Aarhus, Denmark Purpose: Although five-alpha reductase inhibitor (5-ARI) is one of standard treatment for benign prostatic hyperplasia (BPH) or alopecia, potential complications after 5-ARI have been issues recently. This study aimed to investigate the risk of depres- sion after taking 5-ARI and to quantify the risk using meta-analysis. Materials and Methods: A total of 209,940 patients including 207,798 in 5-ARI treatment groups and 110,118 in control groups from five studies were included for final analysis. Inclusion criteria for finial analysis incudes clinical outcomes re- garding depression risk in BPH or alopecia patients. Overall hazard ratio (HR) and odds ratio (OR) for depression were ana- lyzed. Moderator analysis and sensitivity analysis were performed to determine whether HR or OR could be affected by any variables, including number of patients, age, study type, and control type. Results: The pooled overall HRs for the 5-ARI medication was 1.23 (95% confidence interval [CI], 0.99–1.54) in a random effects model.