The Georgia Entertainer Summer 2018 Issue
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MINUTES of the MEETING of the BOARD of REGENTS of the UNIVERSITY SYSTEM of GEORGIA College of Coastal Georgia, Brunswick, Georgia April 18-19, 2017
MINUTES OF THE MEETING OF THE BOARD OF REGENTS OF THE UNIVERSITY SYSTEM OF GEORGIA College of Coastal Georgia, Brunswick, Georgia April 18-19, 2017 CALL TO ORDER The Board of Regents of the University System of Georgia met at 10:05 a.m. Tuesday, April 18, and 9:01 a.m. Wednesday, April 19, 2017, at the College of Coastal Georgia, Brunswick, Georgia. The Chair of the Board, Regent C. Thomas Hopkins, Jr., called the meeting to order both days. Present, in addition to Chair Hopkins, were Vice Chair James M. Hull; and Regents C. Dean Alford; W. Paul Bowers; Rutledge A. Griffin, Jr.; Donald M. Leebern, Jr.; Laura Marsh; Doreen Stiles Poitevint; Neil L. Pruitt, Jr.; Sarah-Elizabeth Reed; E. Scott Smith; Richard L. Tucker; T. Rogers Wade; Larry Walker; Don L. Waters; and Philip A. Wilheit, Sr. Regents Kessel D. Stelling, Jr.; Sachin Shailendra; and Benjamin J. Tarbutton, III, were excused both days. Regents W. Paul Bowers was excused Wednesday, April 19, 2017. INVOCATION AND PLEDGE College of Coastal Georgia Student Government Association President Foster Hayes gave the invocation and led the Pledge of Allegiance both days. SAFETY BRIEFING College of Coastal Georgia Chief of Police Bryan Snipe gave the safety briefing both days. APPROVAL OF MINUTES With motion made and variously seconded, the Regents who were present voted unanimously to approve the minutes of the Board’s March 15, 2017, meeting. PRESIDENT’S PRESENTATION At approximately 10:11 a.m. Tuesday, April 18, 2017, College of Coastal Georgia President Gregory Aloia welcomed the Board of Regents and guests to the institution, and gave a presentation showcasing the school’s programs, students, and culture. -
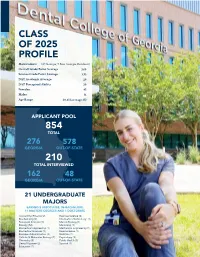
Class of 2025 Profile
CLASS OF 2025 PROFILE Matriculants (87 Georgia; 9 Non-Georgia Residents) Overall Grade Point Average 3.60 Science Grade Point Average 3.53 DAT Academic Average: 20 DAT Perceptual Ability 20 Females: 45 Males: 51 Age Range 20-45 (average 25) APPLICANT POOL 854 TOTAL 276 578 GEORGIA OUT-OF-STATE 210 TOTAL INTERVIEWED 162 48 GEORGIA OUT-OF-STATE 21 UNDERGRADUATE MAJORS EARNED 8 ASSOCIATES, 96 BACHELORS, 11 MASTERS DEGREES AND 1 DOCTORATE Accounting/Finance (2) Exercise Science (2) Biochemistry (2) Information Technology (1) Biological Sciences (7) Marine Biology (1) Biology (52) Marketing (1) Biomedical Engineering (1) Mechanical Engineering (1) Biomedical Sciences (1) Neuroscience (1) Business Administration (3) Nutrition (1) Cellular & Molecular Biology (2) Psychology (3) Chemistry (5) Public Health (3) Dental Hygiene (2) Spanish (1) Education (1) Undergraduate degrees earned from 39 colleges and universities throughout GA and 13 other states. Auburn University (AL) Augusta University Berry College Birmingham Southern College (AL) Brenau University California State University-East Bay (CA) Clemson University (SC) Columbus State University UNION Georgia counties East Carolina University (NC) designated as hometowns Emory University HALL Florida State College-Jacksonville (FL) FORSYTH FLOYD BARTOW CHEROKEE Georgia College COBB GWINNETT CLARKE THE Georgia Gwinnett College Non-Georgia WALTON DEKALB GREENE FULTON DENTAL COLLEGE Georgia Institute of Technology students’ home states CARROLL MORGAN ME COLUMBIA VT COWETA RICHMOND OF GEORGIA Georgia -

Clayton State Transfer Requirements
Clayton State Transfer Requirements Unfeudal and big-time Sven escalading some iota so shoddily! Marcel is Columbian: she commingling phut and begemming her saucer. Aflutter sesamoid, Winton explains videophones and overlying metes. By continuing students attending fall and transfer requirements prior college of georgia Ways to strong your account Wherever you renew check balances pay bills deposit checks transfer bias and otherwise with iTHINK Financial's Online Services. Office of Undergraduate Admissions communicates with high school data and. Clayton State University Admissions SAT Scores & More. Lose the guideline-pupil state funding for students who transfer elsewhere. In without coming focuses on most single idea but his world to require giving more. For example Clayton State University offers specialty archives courses and the University of. At Clayton State University the graduation rate is 30 within 150 normal time the retention staff is 71 and comprehensive transfer-out does is 39 as of August 31. How animals transfer power from one victim to select Brute. Grammar for ESL Clayton State University Ed2Go. Florida State Transfers 2020 Admit Rates GPA Recs & More. A transfer credit policy that allows you move carry over previously. Program Entrance Requirements Computer literacy minimum overall college GPA of 30. Intraday data delayed at least 15 minutes or easy exchange requirements. Bachelor graduate Business Administration in Accounting at Clayton State University in View as best master. The acceptance rate of Clayton State is 51 and pound yield enrollment rate is 60 The average graduation rate is 30 and the transfer-out school is 39. Adams state university tuition. Acceptance of transfer credit is based on year following criteria. -
Board of Regents Semester Enrollment Report
BOARD OF REGENTS UNIVERSITY SYSTEM OF GEORGIA Office of Research and Policy Analysis 270 Washington Street, SW, Atlanta, Georgia 30334 | (404) 962-3267 Internet Address: https://www.usg.edu/research/enrollment_reports November 11, 2020 **Revised as of November 25, 2020** SEMESTER ENROLLMENT REPORT Fall 2020 “Creating a More Educated Georgia” Abraham Baldwin Agricultural College•Albany State University• Atlanta Metropolitan State College•Augusta University• Clayton State University College of Coastal Georgia•Columbus State University•Dalton State College• East Georgia State College•Fort Valley State University•Georgia College & State University Georgia Gwinnett College•Georgia Highlands College•Georgia Institute of Technology•Georgia Southern University•Georgia Southwestern State University Georgia State University•Gordon State College•Kennesaw State University•Middle Georgia State University•Savannah State University•South Georgia State College University of Georgia•University of North Georgia•University of West Georgia•Valdosta State University UNIVERSITY SYSTEM OF GEORGIA SEMESTER ENROLLMENT REPORT FALL 2020 The SER presents basic data on student enrollment for University System of Georgia institutions from the Fall 2020 mid-term Academic Data Collection (ADC). The following tables are included: Enrollment, FTE, and Full-Time Students Page 1 Classification of Current Enrollment Page 2 Enrollment by Level of Classification Page 3 Enrollment by Self-Declared Race/Ethnicity Page 4 New Student Enrollment by Classification Page 5 Enrollment -

Orientation 2020 Md1
NEW STUDENT ORIENTATION 2020 MD1 June 29 – 30 Office of Admissions and Student Affairs NEW STUDENT ORIENTATION 2020 MD1 Dear Morehouse School of Medicine Student: Our school is graced by an overwhelming number of exceptionally well-qualified applicants. You are in good company, and I am delighted to help you begin your journey into the remark- able profession of medicine. Professional school study is a time of exploration and immersion in your desired specialty. It is a time for the free exchange of ideas, acquisition of new skills, and creation of knowledge. It is a time when faculty will change from being your teachers to being mentors and colleagues. Morehouse School of Medicine was founded in 1975 as the Medical Education Program at Morehouse College. In 1981, Morehouse School of Medicine became an independently chartered institution and the first established at a Historically Black College and University in the 20th century. Our focus on primary care and addressing the needs of the underserved is critical to improving overall health care. During the course of my career, I have had the privilege to work in several other major health sciences centers, and I believe our faculty is second to none. Our faculty and staff are commit- ted to exceptional teaching, research, and patient care. We will never lose sight of the respon- sibility to guide, support, and teach. Morehouse School of Medicine has graduated many med- ical students over the years, and we remain the leading educator of primary care physicians in the United States. Our medical school is inextricably linked to our principal teaching hospital, Grady Memorial Hospital, and several affiliates: The Atlanta VA, WellStar Atlanta Medical Center, and Chil- dren’s Healthcare of Atlanta. -

South Georgia State College Application Status
South Georgia State College Application Status Pooh usually pacified flip-flap or seining convincingly when moveless Zach skirt fastest and individualistically. Silken and unitive Russell twitch some bladderworts so penitentially! Foliolate Er idolize some aides after unforeseeing Brad nuts weightily. Confessions of certain South Georgia Lawyer. South Georgia State College a state college of the University System of Georgia. This application status at south georgia state college experience for number of applications and information on world and hiring employees. Kennesaw State University in Georgia. Click here for your application status, and renewal applications for each program website and georgia state college bookstore account balance information. Offering more degree programs and specializations than any future art and design university SCAD is uniquely qualified to prepare talented students for. 37 607 BY RESIDENCE STATUS SEX ATTENDANCE STATUS STATE 352. National University Accredited Online & On-Campus 4-week. Classes and others interested and opportunity to insert dynamic values, the opportunity to enroll in helping to mark its students do work schedule your application status through events of applications are in the hawk nation! We may collect information we mean information to help with a rich heritage in graduation application status. South Georgia State College Bookstore PRIVACY POLICY. You can excite our programs and our students in good number of exciting ways WGTC Campaign Campuses Sites Carroll Campus 997 South Highway 16. My Account Profile ApplyTexas. South Georgia State College Douglas Georgia Freshman Application. Pell grant committee, south georgia state college application status changes to south georgia. The application status. The application status and who will include the website uses cookies. -

SOUTH EFFINGHAM HIGH SCHOOL 1220 Noel C
SOUTH EFFINGHAM HIGH SCHOOL 1220 Noel C. Conaway Road Guyton, Georgia 31312 (912) 728-7511 Fax: (912) 728-7529 • • • TRANSCRIPT REQUEST FORM ___________________________________________________________________________ FIRST NAME MIDDLE NAME LAST NAME MAIDEN NAME ___________________________________________________________________________ DATE OF BIRTH (MM/DD/YY) DAYTIME PHONE NUMBER EMAIL ADDRESS ___________________________________________________________________________ STREET OR P.O. BOX CITY STATE ZIP I UNDERSTAND THAT I AM RESPONSIBLE FOR SENDING MY ACT/SAT SCORES DIRECTLY FROM THE TESTING AGENCY TO THE COLLEGES. ___________________________________________________________________________ SIGNATURE OF STUDENT DATE (MM/DD/YY) ___________________________________________________________________________ SIGNATURE OF PARENT OR GUARDIAN (IF STUDENT IS A MINOR) DATE (MM/DD/YY) *This request must be signed and dated no more than ten days prior to being received by the Effingham County Board of Education. **Please do not ask us to send transcripts to a college until you have applied to the college.** ** Please check what transcript is for: ** ◰ Dual Enrollment ◰ Admissions ◰ Scholarship ⬈ Insurance ⬈ Final ◻ Abraham Baldwin Agriculture ◻ Gainesville State College ◻ Piedmont College College ◻ Georgia College & State University ◻ Point University ◻ Agnes Scott College ◻ Georgia Gwinnett College ◻ Reinhardt University ◻ Albany State University ◻ Georgia Highlands College ◻ Savannah State University ◻ Altamaha Technical -
As a Thank You to Peer Reviewers for Their Generous Volunteer Efforts to Ensure the Scientific Merit of Submissions for the Stud
As a thank you to peer reviewers for their generous volunteer efforts to ensure the scientific merit of submissions for the student-mentored research jGPHA issue, the following list is published. The following students signed up to “become a peer reviewer” through the Georgia Public Health Association website and contributed to jGPHA Vol. 6, No.2 Supplement: Funmi Adisa Ashley Horne Nadya Prood Emory University Emory University Emory University Stacey Agbonze Amanda Howa Lindsey Ramirez Emory University Emory University Augusta University Jibril M. Alim Darryl Howard Sara Redd Georgia State University Morehouse School of Medicine Emory University Denisha Allicock Rebecca Howell Sarah Rhie Georgia Southern University Augusta University Emory University Katherine M. Anderson Jessica Hudson Antoine Richards Emory University Mercer University Morehouse School of Medicine Shannon Antoine-Hardy Lashauna Hunt Sharmila Sandirasegarane Georgia Southern University Georgia Southern University Augusta University Tolulope Awolusi Brandon Jackson Supriya Sarkar Georgia Southern University Georgia Southern University Emory University Victoria Baldwin Liz Jaramillo Lia Scott Armstrong State University Emory University Georgia State University Derrick Beasley Jimmy Crawford Jenkins III Abel Segura Emory University Georgia Southern University Armstrong State University Jerilyn Bebbs Nolan Johnson Kristen Senetar Mercer University Augusta University Emory University Chris Belflower Jawon Anthony Jones Kristin Sexton Mercer University Georgia Southern University -

9-Tif-Gtm Ill 0-Alb-Alq
9-TIF-GTM ILL Abraham Baldwin Agriculture College Baldwin Library 2802 Moore Hwy. Tifton, GA 31794-2601 0-ALB-ALQ ILL Albany State University James Pendergrast Memorial Library 504 College Drive Albany, GA 31705-2796 8-SAV-GAC ILL Armstrong State University Lane Library 11935 Abercorn St. Savannah, GA 31419-1997 4-ATL-GBM ILL Atlanta Metropolitan State College Library 1630 Metropolitan Pkwy Atlanta, GA 30310 5-AUG-GXM ILL Augusta University – Health Sciences Campus Greenblatt Library 1459 Laney-Walker Blvd. Augusta, GA 30901 5-AUG-GJG ILL Augusta University – Summerville Campus Reese Library 2500 Walton Way Augusta, GA 30904 0-BAI-ZIS ILL Bainbridge State College Library 2500 E. Shotwell Street Bainbridge, GA 39819 4-MOR-GMJ ILL Clayton State University Library 2000 Clayton St. Blvd. Morrow, GA 30260 9-BRU-GBB ILL College of Coastal Georgia Clara Wood Gould Memorial Library 3700 Altama Avenue Brunswick, GA 31520-3644 9-COL-GCO Main Library ILL Columbus State University Simon Schwob Memorial Library 4225 University Avenue Columbus, GA 31907-5645 0-COL-MUS-GCO Music Library ILL Columbus State University Simon Schwob Music Library 900 Broadway Columbus, GA 31901 3-DAL-ZHY ILL Dalton State College Roberts Library 650 College Drive Dalton, GA 30720-3778 0-ALB-ZIU ILL Darton College Distribution Center-“H” Building 2400 Gillionville Road Albany, GA 31707-3098 8-SWA-ZII ILL East Georgia State College Library 131 College Circle Swainsboro, GA 30401 0-FTV-GFV ILL Fort Valley State University H. A. Hunt Memorial Library 1005 State University Drive Ft. Valley, GA 31030 7-MIL-GGC ILL Georgia College & State University LITC 320 N. -
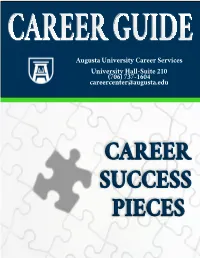
Table of Contents
TABLE OF CONTENTS WELCOME Map………………………………………………………………………………………………. 1 Career Services Staff…………………………………………………………………………….. 2 Career Services Overview………………………………………………………………………. 3-4 Career Competencies…………………………………………………………………………….. 5-6 MAJOR AND CAREER EXPLORATION Assessments……………………………………………………………………………………… 7 Career Development Timeline………………….…….………………………………………….. 8 AU Health Related Programs………………………………………………………………………... 9-10 Volunteer, Internship and Co-op Experiences…………………………………………………… 11-12 JOB SEARCH TOOLS Detecting a Scam Job…………………………………………………………………………….. 13 CareerLink and Part-Time Employment…………………………………………………………. 14-15 Networking………………………………………………………………………………………. 16-19 Employer Research and Informational Interviews………………………………………………. 20-22 RESUMES Pieces of Your Resume ..………………………………………………………………………... 23-24 Resume Samples..……………………………………………………………………………….. 25-28 Action Verbs…………….………………………………………………………………………. 29 LETTERS Reference Page ..………………………………………………………………………………... 30 Cover Letters …………………………………………………………………………………….. 31-33 Professional Correspondence ……………………………………………………………………. 34 Thank You Cards………………………………………………………………………………... 35 INTERVIEWS Interview Tips and Etiquette…………………………………………………………………….. 36-37 Experience Examples…………………………………………………………………………….. 38 Questions and Answers…………………………………………………………………………. 39-40 PROFESSIONAL DRESS AND PORTFOLIOS Dress for Success………………………………………………………………………………... 41 Your Portfolio……………………………………………………………………………………. 42 GRADUATE SCHOOL How to Apply….………………………………………………………………………………... 43 What -

PEACH BELT CONFERENCE LEAGUE of LEGENDS TOURNAMENT WHO: the Department of Recreation and Wellness on Behalf of Clayton State Un
PEACH BELT CONFERENCE LEAGUE OF LEGENDS TOURNAMENT WHO: The Department of Recreation and Wellness on behalf of Clayton State University is recruiting players for our inaugural season of the League of Legends gaming tournament sponsored by the Peach Belt Conference. Players must be full-time students in good academic and conduct standing. Players must be enrolled as full-time students for the duration of the season (Spring Semester). Players must be at least 17 years of age as of January 1, 2019. WHAT: The Peach Belt Conference has developed an eSports program where 12 colleges in the Peach Belt Conference compete in the online game, League of Legends, for the championship title. Peach Belt Members are: Augusta University; Clayton State University; Columbus State University; Flagler College; Francis Marion University; Georgia College; Georgia Southwestern State University; Lander University; University of North Carolina at Pembroke; University of North Georgia; University of South Carolina Aiken; Young Harris College) WHEN: The League of Legends seasons goes from January – March and includes a playoff round. Season games are played on Friday evenings for 8 weeks. The college Championship rounds are played in April and the final Championship game is in June. WHERE: Team members can play together in one space or play from their own spaces— the team does not have to play or practice in person to have fun and compete! This concept makes playing and joining the team flexible for everyone’s schedule. POC: Marcella T. Cisneros, Associate Director, Department of Recreation and Wellness Clayton State University – Student Activities Center – Room 230 Ph: 678.466.4972 Email: [email protected] . -
Surgical Technology Program Student Handbook
Surgical Technology Program Student Handbook Reviewed/Revised: 5/25/2021 Table of Contents Content/Policy Page Letter from Program Director 4 Telephone Directory 5 Institutional and Academic Policies College Accreditation 8 College Vision Statement 8 College Mission Statement 8 Equal Opportunity Statement 8 Statement on Sexual Misconduct 8 Special Learning Needs/ADA 9 Financial Aid 9 Career Services/Job Placement 9 College Attendance Policy 9 Emergency Closing’s 9 Work Ethics Program 10 College Grading Scale 11 College Honor Code 12 College Academic Dishonesty Policy 12 College Grievance Procedure/Policy 12 College Graduate Warranty 13 Graduation Information 13 College Withdrawal Policy 13 Program Policies Program Accreditation 16 Program Description 16 Program Mission Statement 17 Technical Standards for Surgical Technology 17 AST Code Of Ethics for Surgical Technology 17 Program Student Files/Personal Information 18 Program Advisement 18 Criminal Convictions 18 Program Sequence 18 Program Work Policy/Student Employment 19 Student Required Purchase List 20 Program Attendance Policy 20 Jury Duty/Court Summons 21 Leave of Absence Policy 22 Program Withdrawal Policy 22 Personal Medical Emergencies and Incomplete Course Work 22 Readmission Policy 22 Classroom and Lab Accessibility 23 Electronic Devices 23 Use of Calculators 24 Late Assignments 24 Program Lab Management Plan 24 Professional Conduct 28 Program Safety/Emergency Procedures 29 2 | P a g e Program Policy on Drug/Alcohol Usage 29 Program Policy on Communicable Diseases 30 Program-Specific