The Rostrocaudal Axis. Part II. Posterior Clinoids to the Foramen Magnum
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MR Imaging of the Orbital Apex
J Korean Radiol Soc 2000;4 :26 9-0 6 1 6 MR Imaging of the Orbital Apex: An a to m y and Pat h o l o g y 1 Ho Kyu Lee, M.D., Chang Jin Kim, M.D.2, Hyosook Ahn, M.D.3, Ji Hoon Shin, M.D., Choong Gon Choi, M.D., Dae Chul Suh, M.D. The apex of the orbit is basically formed by the optic canal, the superior orbital fis- su r e , and their contents. Space-occupying lesions in this area can result in clinical d- eficits caused by compression of the optic nerve or extraocular muscles. Even vas c u l a r changes in the cavernous sinus can produce a direct mass effect and affect the orbit ap e x. When pathologic changes in this region is suspected, contrast-enhanced MR imaging with fat saturation is very useful. According to the anatomic regions from which the lesions arise, they can be classi- fied as belonging to one of five groups; lesions of the optic nerve-sheath complex, of the conal and intraconal spaces, of the extraconal space and bony orbit, of the cav- ernous sinus or diffuse. The characteristic MR findings of various orbital lesions will be described in this paper. Index words : Orbit, diseases Orbit, MR The apex of the orbit is a complex region which con- tains many nerves, vessels, soft tissues, and bony struc- Anatomy of the orbital apex tures such as the superior orbital fissure and the optic canal (1-3), and is likely to be involved in various dis- The orbital apex region consists of the optic nerve- eases (3). -

Anatomic Variations of the Nose and Paranasal Sinuses in Saudi Population
234 Original article Anatomic variations of the nose and paranasal sinuses in saudi population: computed tomography scan analysis Nada Alshaikha, Amirah Aldhuraisb aDepartment of Otolaryngology Head & Neck Background Surgery, Rhinology Unit, Dammam Medical Knowledge of the anatomy constitutes an integral part in the total management of Complex (DMC), bDepartment of ENT, King Fahad Specialist Hospital (KFSH), Dammam, patients with sinonasal diseases. The aim of this study was to obtain the prevalence Saudi Arabia of sinonasal anatomic variations in Saudi population and to understand their importance and impact on the disease process, as well as their influence on Correspondence to Nada Alshaikh, MD, Department of Otorhinolaryngology Head and surgical management and outcome. Neck Surgery, Dammam Medical Complex, Materials and methods Dammam - 31414, Saudi Arabia This study is prospective review of retrospectively performed normal computed e-mail: [email protected] tomography (CT) scans of the nose and paranasal sinuses in adult Saudi Received 13 November 2016 population at Dammam Medical Complex. The scans were reviewed by two Accepted 23 December 2016 independent observers. The Egyptian Journal of Otolaryngology Results 2018, 34:234–241 Of all CT scans that were reviewed, 48.4% were of female patients and 51.6% were of male patients. The mean age of the study sample was 38.5±26.5 years. The most common anatomic variation after excluding agger nasi cell was pneumatized crista galli, which was seen in 73% of the scans. However, the least common variation seen in this series was hypoplasia of the maxillary sinus, which was encountered in 5% of the cases. We did not detect a single pneumatized inferior turbinate among the studied scans. -

Septation of the Sphenoid Sinus and Its Clinical Significance
1793 International Journal of Collaborative Research on Internal Medicine & Public Health Septation of the Sphenoid Sinus and its Clinical Significance Eldan Kapur 1* , Adnan Kapidžić 2, Amela Kulenović 1, Lana Sarajlić 2, Adis Šahinović 2, Maida Šahinović 3 1 Department of anatomy, Medical faculty, University of Sarajevo, Čekaluša 90, 71000 Sarajevo, Bosnia and Herzegovina 2 Clinic for otorhinolaryngology, Clinical centre University of Sarajevo, Bolnička 25, 71000 Sarajevo, Bosnia and Herzegovina 3 Department of histology and embriology, Medical faculty, University of Sarajevo, Čekaluša 90, 71000 Sarajevo, Bosnia and Herzegovina * Corresponding Author: Eldan Kapur, MD, PhD Department of anatomy, Medical faculty, University of Sarajevo, Bosnia and Herzegovina Email: [email protected] Phone: 033 66 55 49; 033 22 64 78 (ext. 136) Abstract Introduction: Sphenoid sinus is located in the body of sphenoid, closed with a thin plate of bone tissue that separates it from the important structures such as the optic nerve, optic chiasm, cavernous sinus, pituitary gland, and internal carotid artery. It is divided by one or more vertical septa that are often asymmetric. Because of its location and the relationships with important neurovascular and glandular structures, sphenoid sinus represents a great diagnostic and therapeutic challenge. Aim: The aim of this study was to assess the septation of the sphenoid sinus and relationship between the number and position of septa and internal carotid artery in the adult BH population. Participants and Methods: A retrospective study of the CT analysis of the paranasal sinuses in 200 patients (104 male, 96 female) were performed using Siemens Somatom Art with the following parameters: 130 mAs: 120 kV, Slice: 3 mm. -

Investigating the Various Shapes of Sella Turcica in Nigerian Children Using Lateral Skull Radiographs
International Journal of Health Sciences and Research www.ijhsr.org ISSN: 2249-9571 Original Research Article Investigating the Various Shapes of Sella Turcica in Nigerian Children Using Lateral Skull Radiographs Bello A., Usman J.D. Department of Anatomy, Faculty of Basic Medical Sciences, College of Health Sciences, Usmanu Danfodiyo University, Sokoto, Nigeria. Corresponding Author: Bello A ABSTRACT The knowledge of the normal radiographic anatomy of the sella turcica and sella point is of great importance to clinicians in enabling them quickly recognize, investigate or evaluate any deviation from normal as well as any pathological situation related to the pituitary gland. This study investigated the various shapes of the sella turcica in children. A total of 250 lateral skull radiographs taken in the Department of Radiology, Usmanu Danfodiyo University Teaching Hospital (UDUTH), Sokoto from January 2013 to December 2014 were retrieved for the purpose of this study. Radiographs were mounted on the viewing box and variants of the anatomical shapes of the sella turcica were studied and classified. Of the 162 radiographs used in this study, 114 (70.4%) sella turcica were round shaped while 48 (29.6%) oval in shaped. This observed difference was statistically significant (p<0.001). Meanwhile, the floor of the sella turcica of the study participants showed a concave outline in 130 (80%) of the children and flat outline in 32 (20%) of the children. Sexual dimorphism was seen in this study with respect to shape of sella turcica. Round shaped sella turcica was predominant in Nigerian children used in this study. The prevalence and the relative frequencies of the normal variants of the anatomical shapes of the sella turcica of male Nigerian children differ significantly from those of their female counterparts. -

Macroscopic Anatomy of the Nasal Cavity and Paranasal Sinuses of the Domestic Pig (Sus Scrofa Domestica) Daniel John Hillmann Iowa State University
Iowa State University Capstones, Theses and Retrospective Theses and Dissertations Dissertations 1971 Macroscopic anatomy of the nasal cavity and paranasal sinuses of the domestic pig (Sus scrofa domestica) Daniel John Hillmann Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/rtd Part of the Animal Structures Commons, and the Veterinary Anatomy Commons Recommended Citation Hillmann, Daniel John, "Macroscopic anatomy of the nasal cavity and paranasal sinuses of the domestic pig (Sus scrofa domestica)" (1971). Retrospective Theses and Dissertations. 4460. https://lib.dr.iastate.edu/rtd/4460 This Dissertation is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Retrospective Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. 72-5208 HILLMANN, Daniel John, 1938- MACROSCOPIC ANATOMY OF THE NASAL CAVITY AND PARANASAL SINUSES OF THE DOMESTIC PIG (SUS SCROFA DOMESTICA). Iowa State University, Ph.D., 1971 Anatomy I University Microfilms, A XEROX Company, Ann Arbor. Michigan I , THIS DISSERTATION HAS BEEN MICROFILMED EXACTLY AS RECEIVED Macroscopic anatomy of the nasal cavity and paranasal sinuses of the domestic pig (Sus scrofa domestica) by Daniel John Hillmann A Dissertation Submitted to the Graduate Faculty in Partial Fulfillment of The Requirements for the Degree of DOCTOR OF PHILOSOPHY Major Subject: Veterinary Anatomy Approved: Signature was redacted for privacy. h Charge of -^lajoï^ Wor Signature was redacted for privacy. For/the Major Department For the Graduate College Iowa State University Ames/ Iowa 19 71 PLEASE NOTE: Some Pages have indistinct print. -

MBB: Head & Neck Anatomy
MBB: Head & Neck Anatomy Skull Osteology • This is a comprehensive guide of all the skull features you must know by the practical exam. • Many of these structures will be presented multiple times during upcoming labs. • This PowerPoint Handout is the resource you will use during lab when you have access to skulls. Mind, Brain & Behavior 2021 Osteology of the Skull Slide Title Slide Number Slide Title Slide Number Ethmoid Slide 3 Paranasal Sinuses Slide 19 Vomer, Nasal Bone, and Inferior Turbinate (Concha) Slide4 Paranasal Sinus Imaging Slide 20 Lacrimal and Palatine Bones Slide 5 Paranasal Sinus Imaging (Sagittal Section) Slide 21 Zygomatic Bone Slide 6 Skull Sutures Slide 22 Frontal Bone Slide 7 Foramen RevieW Slide 23 Mandible Slide 8 Skull Subdivisions Slide 24 Maxilla Slide 9 Sphenoid Bone Slide 10 Skull Subdivisions: Viscerocranium Slide 25 Temporal Bone Slide 11 Skull Subdivisions: Neurocranium Slide 26 Temporal Bone (Continued) Slide 12 Cranial Base: Cranial Fossae Slide 27 Temporal Bone (Middle Ear Cavity and Facial Canal) Slide 13 Skull Development: Intramembranous vs Endochondral Slide 28 Occipital Bone Slide 14 Ossification Structures/Spaces Formed by More Than One Bone Slide 15 Intramembranous Ossification: Fontanelles Slide 29 Structures/Apertures Formed by More Than One Bone Slide 16 Intramembranous Ossification: Craniosynostosis Slide 30 Nasal Septum Slide 17 Endochondral Ossification Slide 31 Infratemporal Fossa & Pterygopalatine Fossa Slide 18 Achondroplasia and Skull Growth Slide 32 Ethmoid • Cribriform plate/foramina -

Anatomic Variations of Sphenoid Sinus Pneumatization in a Sample of Turkish Population: MRI Study
Int. J. Morphol., 32(4):1140-1143, 2014. Anatomic Variations of Sphenoid Sinus Pneumatization in a Sample of Turkish Population: MRI Study Variaciones Anatómicas de la Neumatización del Seno Esfenoidal en una Muestra de Población Turca: Estudio por Resonancia Magnética Ozdemir Sevinc*; Merih Is**; Cagatay Barut*** & Aliriza Erdogan**** SEVINC, O.; IS, M.; BARUT, C. & ERDOGAN, A. Anatomic Variations of Sphenoid Sinus Pneumatization in a Sample of Turkish Population: MRI Study. Int. J. Morphol., 32(4):1140-1143, 2014. SUMMARY: There are a number of variations regarding morphometric anatomy and degree of pneumatization of the sphenoid sinus. In our study, we planned to examine and show the differences of pneumatization of the sphenoid sinus particularly to guide the neurosurgeon during transsphenoidal surgery. Sagittal T1-weighed spin-echo Magnetic Resonance Images (MRIs) of 616 adult individuals (406 women and 210 men) were analyzed, retrospectively. According to the collected data from our study, the most common type of the sphenoid sinus was the sellar type (83%; n=511) for the whole study group. Of the 616 individuals 16.6% (n=102) had presellar type and 0.5% (n=3) had conchal type of sphenoid sinus. Preoperative detailed detection of the anatomical characteristics of sphenoid sinus is essential. A thorough information obtained from studies of the regional anatomy and awareness of its variability can provide a safe and accurate transsphenoidal and extended endoscopic skull base approaches. KEY WORDS: Paranasal sinus; Pneumatization; Sphenoid sinus; Transsphenoidal approach. INTRODUCTION The sphenoid sinus is the most hidden and first years of life, it extends backward into the presellar area inaccessible of the paranasal sinuses which is approached and gradually expands into the area below and behind the by neurosurgeons via many surgical routes through basis sella turcica, and reaches its full size during adolescence cranii (Hewaidi & Omami, 2008). -

Sella Turcica Morphology on Cephalometric Radiographs and Dental Abnormalities—Is There Any Association? —Systematic Review
International Journal of Environmental Research and Public Health Review Sella Turcica Morphology on Cephalometric Radiographs and Dental Abnormalities—Is There Any Association? —Systematic Review Tomasz Jankowski 1, Maciej Jedli ´nski 2 , Katarzyna Grocholewicz 2 and Joanna Janiszewska-Olszowska 2,* 1 Private Practice Dental Clinic Jankowscy, 68-200 Zary,˙ Poland; [email protected] 2 Department of Interdisciplinary Dentistry, Pomeranian Medical University in Szczecin, 70-204 Szczecin, Poland; [email protected] (M.J.); [email protected] (K.G.) * Correspondence: [email protected]; Tel.: +48-91-466-1690 Abstract: Background: The sella turcica is a saddle-like structure in the middle cranial fossa on the intracranial surface of the sphenoid bone, visible on lateral cephalograms routinely conducted for orthodontic diagnosis. The development of facial structures follows similar traits to the sella turcica: glandular anomalies may be associated with functional disorders, e.g., altered hormonal levels, thus influencing dental development. The aim of this study is to find out if there is any association between the morphology of the sella turcica on cephalometric radiographs and the presence of dental abnormalities. (2) Methods: The search was conducted on 27 January 2021 in four search engines: Medline (PubMed Central), Scopus, Web of Science, Embase. The keywords used in the search strategy were as follows: “sella turcica” AND (“dental abnormalities” OR “dental anomalies” OR Citation: Jankowski, T.; Jedli´nski,M.; “malocclusion”). Since all the studies finally included were retrospective case–control studies, the Grocholewicz, K.; Janiszewska- Newcastle–Ottawa Quality Assessment Form for Case–Control Studies was applied. (3) Results: The Olszowska, J. Sella Turcica search strategy identified 465 articles: 289 from PubMed, 121 from Scopus, 32 from Web of Science and Morphology on Cephalometric 23 from Embase. -

Level I to III Craniofacial Approaches Based on Barrow Classification For
Neurosurg Focus 30 (5):E5, 2011 Level I to III craniofacial approaches based on Barrow classification for treatment of skull base meningiomas: surgical technique, microsurgical anatomy, and case illustrations EMEL AVCı, M.D.,1 ERINÇ AKTÜRE, M.D.,1 HAKAN SEÇKIN, M.D., PH.D.,1 KUTLUAY ULUÇ, M.D.,1 ANDREW M. BAUER, M.D.,1 YUSUF IZCI, M.D.,1 JACQUes J. MORCOS, M.D.,2 AND MUSTAFA K. BAşKAYA, M.D.1 1Department of Neurological Surgery, University of Wisconsin–Madison, Wisconsin; and 2Department of Neurological Surgery, University of Miami, Florida Object. Although craniofacial approaches to the midline skull base have been defined and surgical results have been published, clear descriptions of these complex approaches in a step-wise manner are lacking. The objective of this study is to demonstrate the surgical technique of craniofacial approaches based on Barrow classification (Levels I–III) and to study the microsurgical anatomy pertinent to these complex craniofacial approaches. Methods. Ten adult cadaveric heads perfused with colored silicone and 24 dry human skulls were used to study the microsurgical anatomy and to demonstrate craniofacial approaches in a step-wise manner. In addition to cadaveric studies, case illustrations of anterior skull base meningiomas were presented to demonstrate the clinical application of the first 3 (Levels I–III) approaches. Results. Cadaveric head dissection was performed in 10 heads using craniofacial approaches. Ethmoid and sphe- noid sinuses, cribriform plate, orbit, planum sphenoidale, clivus, sellar, and parasellar regions were shown at Levels I, II, and III. In 24 human dry skulls (48 sides), a supraorbital notch (85.4%) was observed more frequently than the supraorbital foramen (14.6%). -

Effects of Morphological Changes in Sella Turcica: a Review
European Journal of Molecular & Clinical Medicine ISSN 2515-8260 Volume 07, Issue 03, 2020 1662 EFFECTS OF MORPHOLOGICAL CHANGES IN SELLA TURCICA: A REVIEW Chandrakala B1, Govindarajan Sumathy2, Bhaskaran Sathyapriya*, Pavishwarya P3, Sweta Jain3 1. Senior Lecturer, Department of Anatomy, Sree Balaji Dental College & Hospital, Bharath Institute of Higher Education & Research, Chennai. 2. Professor and Head, Department of Anatomy, Sree Balaji Dental College & Hospital, Bharath Institute of Higher Education & Research, Chennai. 3. Graduate student, Sree Balaji Dental College and Hospital, Bharath Institute of Higher Education and Research *Professor, Department of Anatomy, Sree Balaji Dental College & Hospital, Bharath Institute of Higher Education & Research, Chennai. Corresponding author: Dr. Bhaskaran Sathyapriya Professor, Department of Anatomy, Sree Balaji Dental College & Hospital, Bharath Institute of Higher Education & Research, Chennai. ABSTRACT Sella turcica is a saddle shaped bony structure present on the sphenoid bone. The pituitary gland is seated at the inferior aspect of the sella turcica, called hypophyseal fossa. Sella turcica serves as a cephalometric landmark, that being said any morphological changes can affect the overall craniometry of the individual as well as alter the function of the structures it lodges. The following review emphasis on the possible morphological changes of sella turcica and its effects on the individual. Keywords: Pituitary gland, morphology, bridge, foramen, bone. 1662 European Journal of Molecular -
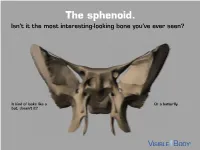
The Sphenoid. Isn’T It the Most Interesting-Looking Bone You’Ve Ever Seen?
The sphenoid. Isn’t it the most interesting-looking bone you’ve ever seen? It kind of looks like a Or a butterfly. bat, doesn’t it? The sphenoid articulates with 12 bones, both in the neurocranium and facial skeleton. The sphenoid is not just present in human skeletons, but also in mammalian ones. : A human has 1 Factoid sphenoid bone, but a dog has 8 bones that make up its sphenoid. The sphenoid is one of the 8 bones of the neurocranium (bones that protect the brain). It is the keystone* bone at the base of the skull. *In architecture, a keystone is the piece at the apex of an arch, locking all the other pieces together and bearing the weight of it all. The body of the sphenoid is the central part of the bone. It is a hollowed-out, cubical portion of the bone that forms the sphenoidal sinuses. The body is home to a deep depression known as the Sella turcica, which houses the pituitary gland. Factoid: sella turcica is Latin for “Turkish saddle” because of its resemblance to the saddles used by Turks, which had supports in the front and back. The greater wings of the sphenoid articulate with several bones, including the frontal, temporal, parietal, and zygomatic. They also serve as the attachment site for the temporalis muscles. The lesser wings are thin, triangular plates located above the greater wings. They, along with the body, form the optic canal. The optic nerve (II) passes through the optic canal to the eyes. The lateral and medial pterygoid plates project downward from the sphenoid body to give shape to the nasal cavity. -

Surgical Anatomy of the Paranasal Sinus M
13674_C01.qxd 7/28/04 2:14 PM Page 1 1 Surgical Anatomy of the Paranasal Sinus M. PAIS CLEMENTE The paranasal sinus region is one of the most complex This chapter is divided into three sections: develop- areas of the human body and is consequently very diffi- mental anatomy, macroscopic anatomy, and endoscopic cult to study. The surgical anatomy of the nose and anatomy. A basic understanding of the embryogenesis of paranasal sinuses is published with great detail in most the nose and the paranasal sinuses facilitates compre- standard textbooks, but it is the purpose of this chapter hension of the complex and variable adult anatomy. In to describe those structures in a very clear and systematic addition, this comprehension is quite useful for an accu- presentation focused for the endoscopic sinus surgeon. rate evaluation of the various potential pathologies and A thorough knowledge of all anatomical structures their managements. Macroscopic description of the and variations combined with cadaveric dissections using nose and paranasal sinuses is presented through a dis- paranasal blocks is of utmost importance to perform cussion of the important structures of this complicated proper sinus surgery and to avoid complications. The region. A correlation with intricate endoscopic topo- complications seen with this surgery are commonly due graphical anatomy is discussed for a clear understanding to nonfamiliarity with the anatomical landmarks of the of the nasal cavity and its relationship to adjoining si- paranasal sinus during surgical dissection, which is con- nuses and danger areas. A three-dimensional anatomy is sequently performed beyond the safe limits of the sinus.