Joint Contractures Following Intra- Articular Fracture Surgery: Where Are We Now?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

International Journal of Pharmtech Research CODEN (USA): IJPRIF, ISSN: 0974-4304, ISSN(Online): 2455-9563 Vol.13, No.01, Pp 20-25, 2020
International Journal of PharmTech Research CODEN (USA): IJPRIF, ISSN: 0974-4304, ISSN(Online): 2455-9563 Vol.13, No.01, pp 20-25, 2020 Comparison of Post-Operative Clinical Outcome of Patients with PosteriorInstrumentation After Spinal Cord Injury in Thoracic, Thoracolumbar, and Lumbar Region at Haji Adam Malik General Hospital, Medan from 2016 to 2018 Budi Achmad M. Siregar1*, Pranajaya Dharma Kadar2, Aga Shahri Putera Ketaren3 1Resident of Orthopaedic and Traumatology, Faculty of Medicine, University of Sumatera Utara / Haji Adam Malik General Hospital, Medan, Indonesia 2Consultant Orthopaedic and Traumatology, Spine Division, Faculty of Medicine, University of Sumatera Utara / Haji Adam Malik General Hospital, Medan, Indonesia 3Consultant Orthopaedic and Traumatology, Upper Extremity Division,Faculty of Medicine, University of Sumatera Utara / Haji Adam MalikGeneral Hospital, Medan , Indonesia Abstract : Introduction : Spinal cord injury is a damaging situation related to severe disability and death after trauma.And the term spinal cord injury refers to damage of the spinal cord resulting from trauma. Spinal injuries treatment is still in debate for some cases, whether using conservative or surgical methods. Material and Methods : The study was a retrospective, unpaired observational analytic study with a cross- sectional approach. It was conducted at Haji Adam Malik General Hospital, Medan from January 2016 to December 2018. Clinical outcome of patientswere calculated using SF 36, ODI, and VAS.Data would be tested using the Saphiro-Wilk test. We were using the significance level of 1% (0.01) and the relative significance level of 10% (0.1). Results : Clinical outcomes of patients with spinal cord injuries before posterior instrumentation rated using ODI and VAS were 75.93±6.75 and 4.75±0.98 respectively. -

Missed Spinal Lesions in Traumatized Patients Ana M Cerván De La Haba*, Miguel Rodríguez Solera J, Miguel S Hirschfeld León and Enrique Guerado Parra
de la Haba et al. Trauma Cases Rev 2016, 2:027 Volume 2 | Issue 1 ISSN: 2469-5777 Trauma Cases and Reviews Case Series: Open Access Missed Spinal Lesions in Traumatized Patients Ana M Cerván de la Haba*, Miguel Rodríguez Solera J, Miguel S Hirschfeld León and Enrique Guerado Parra Department of Orthopaedic Surgery, Traumatology and Rehabilitation, Hospital Universitario Costa del Sol. University of Malaga, Spain *Corresponding author: Ana M Cerván de la Haba, Hospital Universitario Costa del Sol, Autovía A7 km 187 C.P. 29603, Marbella, Spain, Tel: 951976224, E-mail: [email protected] will help in decreasing the number of missed spinal injuries, being Abstract claim that standardized tertiary trauma survey is vitally important Overlooked spinal injuries and delayed diagnosis are still common in the detection of clinically significant missed injuries and should in traumatized patients. The management of trauma patients is one be included in trauma care, our misdiagnosis occurs at first or later of the most important challenges for the specialist in trauma. Proper examinations [3]. However despite even a third survey still many training and early suspicion of this lesion are of overwhelming injuries are overlooked [4,5]. importance. The damage control orthopaedics, diagnosis and treatment In this paper based on the case method, we discuss the diagnosis algorithm applied to multitrauma patients reduces both morbidity of missable spinal fractures within several traumatic settings. and mortality in polytrauma patients due to missed lesions. Algorithm on its diagnosis and after on its treatment is necessary Case Studies in order to decrease complications. Despite application of care protocols for trauma patients still exist missed spinal injuries. -

The Athlete's Concussion Epidemic
Lindenwood University Digital Commons@Lindenwood University Theses Theses & Dissertations Spring 5-2020 The Athlete’s Concussion Epidemic Andrew James Marsh Lindenwood University Follow this and additional works at: https://digitalcommons.lindenwood.edu/theses Part of the Arts and Humanities Commons Recommended Citation Marsh, Andrew James, "The Athlete’s Concussion Epidemic" (2020). Theses. 17. https://digitalcommons.lindenwood.edu/theses/17 This Thesis is brought to you for free and open access by the Theses & Dissertations at Digital Commons@Lindenwood University. It has been accepted for inclusion in Theses by an authorized administrator of Digital Commons@Lindenwood University. For more information, please contact [email protected]. !1 THE ATHLETE’S CONCUSSION EPIDEMIC by Andrew Marsh Submitted in Partial Fulfillment of the Requirements for the Degree of Master of Arts in Mass Communication at Lindenwood University © May 2020, Andrew James Marsh The author hereby grants Lindenwood University permission to reproduce and to distribute publicly paper and electronic thesis copies of document in whole or in part in any medium now known or hereafter created. !2 THE ATHLETE’S CONCUSSION EPIDEMIC A Thesis Submitted to the Faculty of the Broadcast and Media Operations for the School of Arts, Media, and Communications Department in Partial Fulfillment of the Requirements for the Degree of Master of Arts at Lindenwood University By Andrew James Marsh Saint Charles, Missouri May 2020 !3 ABSTRACT Title of Thesis: The Athlete’s Concussion Epidemic Andrew Marsh, Master of Arts/Mass Communication, 2020 Thesis Directed by: Mike Wall, Director of Broadcast and Media Operations for the School of Arts, Media, and Communications The main goal of this project is to inform and educate you on the various threads concerning concussions in the world of sports. -

Treatment of Established Volkmann's Contracture*
~hop. Acta Treatment of Established Volkmann’sContracture* BY KENYA TSUGE, M.D.’J’, HIROSHIMA, JAPAN ldon, From the Department of Orthopaedic Surgery, Hiroshima Universi~.’ 1-76, School of Medicine, Hiroshima 38. The disease first described by Volkmann in 1881 is the extent of the disease: mild, moderate, and severe. In generally considered to result from spasm of the main ar- the mild type, also called the localized type, there was de- ~ts of teries of the forearm, and their branches as a consequence generation of part of the flexor digitorum profundus mus- Acta of trauma to the elbow or forearm. The severe and pro- cle, causing contractures in only two or three fingers. longed but incomplete interruption of arterial blood sup- There were hardly any neurological signs, and when pres- ~. (in ply, together with venostasis, produces acute ischemic ent they were minimum. In the moderate type, the muscle z and necrosis of the flexor muscles. The most marked ischemia degeneration involved all or nearly all of the flexor digito- occurs in the deeply situated muscles such as the flexor rum profundus and flexor pollicis longus, with partial pollicis longus and flexor digitorum profundus, but severe degeneration of the superficial muscles as well. The neu- ischemia is evident in the pronator teres and flexor rological signs were invariably present and generally -484, digitorum superficialis muscles, and comparatively mild the median nerve was more severely affected than the :rtag, ischemia occurs in the superficially located muscles such ulnar nerve. In the severe type, there was degeneration as the wrist flexors. The muscle degeneration which fol- of all the flexor muscles with necrosis in the center ). -

International Association of Dental Traumatology Guidelines for the Management of Traumatic Dental Injuries: 3
ENDORSEMENTS: INJURIES IN PRIMARY DENTITION International Association of Dental Traumatology Guidelines for the Management of Traumatic Dental Injuries: 3. Injuries in the Primary Dentition Endorsed by the American Academy + How to Cite: Day PF, Flores MT, O’Connell AC, et al. International of Pediatric Dentistry Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 3. Injuries in the primary dentition. 2020 Dent Traumatol 2020;36:343-359. https://doi.org/10.1111/edt.12576. Authors Peter F. Day1 • Marie Therese Flores2 • Anne C. O’Connell3 • Paul V. Abbott4 • Georgios Tsilingaridis5,6 Ashraf F. Fouad7 • Nestor Cohenca8 • Eva Lauridsen9 • Cecilia Bourguignon10 • Lamar Hicks11 • Jens Ove Andreasen12 • Zafer C. Cehreli13 • Stephen Harlamb14 • Bill Kahler15 • Adeleke Oginni16 • Marc Semper17 • Liran Levin18 Abstract Traumatic injuries to the primary dentition present special problems that often require far different management when compared to that used for the permanent dentition. The International Association of Dental Traumatology (IADT) has developed these Guidelines as a con- sensus statement after a comprehensive review of the dental literature and working group discussions. Experienced researchers and clinicians from various specialties and the general dentistry community were included in the working group. In cases where the published data did not appear conclusive, recommendations were based on the consensus opinions or majority decisions of the working group. They were then reviewed and approved by the members of the IADT Board of Directors. The primary goal of these Guidelines is to provide clinicians with an approach for the immediate or urgent care of primary teeth injuries based on the best evidence provided by the literature and expert opinions. -

Rotator Cuff Tear Arthropathy: Pathophysiology, Diagnosis And
yst ar S em ul : C c u s r u r e M n t & R Orthopedic & Muscular System: c e Aydin, et al., Orthopedic Muscul Syst 2014, 3:2 i s d e e a p ISSN: 2161-0533r o c DOI: 10.4172/2161-0533-3-1000159 h h t r O Current Research Review Article Open Access Rotator Cuff Tear Arthropathy: Pathophysiology, Diagnosis and Treatment Nuri Aydin*, Okan Tok and Bariş Görgün Istanbul University Cerrahpaşa, School of Medicine, Istanbul, Turkey *Corresponding author: Nuri Aydin, Istanbul University Cerrahpaşa, School of Medicine, Orthopaedics and Traumatology, Istanbul, Turkey, Tel: +905325986232; E- mail: [email protected] Rec Date: Jan 25, 2014, Acc Date: Mar 22, 2014, Pub Date: Mar 28, 2014 Copyright: © 2014 Aydin N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract The term rotator cuff tear arthropathy is a broad spectrum pathology but it involves common characteristic features as rotator cuff tear, leading to glenohumeral joint arthritis and superior migration of the humeral head. Although there are several factors described causing rotator cuff tear arthropathy, the exact mechanism is still unknown because the rotator cuff tear arthropathy develops in only a group of patients with chronic rotator cuff tear. The aim of this article is to review pathophysiology of rotator cuff tear arthropathy, to explain the diagnostic features and to discuss the management of the disease. Keywords: Arthropathy; Glenohumeral joint; Articular fluid Rotator cuff tear not only plays a role at the beginning of the disease, but also a developed rotator cuff tear is a result of the inflammatory Introduction process. -

About Soft Tissue Sarcoma Overview and Types
cancer.org | 1.800.227.2345 About Soft Tissue Sarcoma Overview and Types If you've been diagnosed with soft tissue sarcoma or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is a Soft Tissue Sarcoma? Research and Statistics See the latest estimates for new cases of soft tissue sarcoma and deaths in the US and what research is currently being done. ● Key Statistics for Soft Tissue Sarcomas ● What's New in Soft Tissue Sarcoma Research? What Is a Soft Tissue Sarcoma? Cancer starts when cells start to grow out of control. Cells in nearly any part of the body can become cancer and can spread to other areas. To learn more about how cancers start and spread, see What Is Cancer?1 There are many types of soft tissue tumors, and not all of them are cancerous. Many benign tumors are found in soft tissues. The word benign means they're not cancer. These tumors can't spread to other parts of the body. Some soft tissue tumors behave 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 in ways between a cancer and a non-cancer. These are called intermediate soft tissue tumors. When the word sarcoma is part of the name of a disease, it means the tumor is malignant (cancer).A sarcoma is a type of cancer that starts in tissues like bone or muscle. Bone and soft tissue sarcomas are the main types of sarcoma. Soft tissue sarcomas can develop in soft tissues like fat, muscle, nerves, fibrous tissues, blood vessels, or deep skin tissues. -

Chinese Expert Consensus on Echelons Treatment of Thoracic
Zong et al. Military Medical Research (2018) 5:34 https://doi.org/10.1186/s40779-018-0181-6 POSITION ARTICLE AND GUIDELINES Open Access Chinese expert consensus on echelons treatment of thoracic injury in modern warfare Zhao-Wen Zong1*, Zhi-Nong Wang2, Si-Xu Chen1, Hao Qin1, Lian-Yang Zhang3, Yue Shen3, Lei Yang1, Wen-Qiong Du1, Can Chen1, Xin Zhong1, Lin Zhang4, Jiang-Tao Huo4, Li-Ping Kuai5, Li-Xin Shu6, Guo-Fu Du5, Yu-Feng Zhao3 and Representing the Traumatology Branch of the China Medical Rescue Association, the Youth Committee on Traumatology Branch of the Chinese Medical Association, the PLA Professional Committee and the Youth Committee on Disaster Medicine, and the Disaster Medicine Branch of the Chongqing Association of Integrative Medicine Abstract The emergency treatment of thoracic injuries varies of general conditions and modern warfare. However, there are no unified battlefield treatment guidelines for thoracic injuries in the Chinese People’s Liberation Army (PLA). An expert consensus has been reached based on the epidemiology of thoracic injuries and the concept of battlefield treatment combined with the existing levels of military medical care in modern warfare. Since there are no differences in the specialized treatment for thoracic injuries between general conditions and modern warfare, first aid, emergency treatment, and early treatment of thoracic injuries are introduced separately in three levels in this consensus. At Level I facilities, tension pneumothorax and open pneumothorax are recommended for initial assessment during the first aid stage. Re-evaluation and further treatment for hemothorax, flail chest, and pericardial tamponade are recommended at Level II facilities. -

Table of Contents 1
GENERAL THORACIC SURGERY DATABASE v.2.3 TRAINING MANUAL August 2017 Table of Contents 1. Demographics ................................................................................................................................................................. 2 2. Follow Up ........................................................................................................................................................................ 9 3. Admission ..................................................................................................................................................................... 10 4. Pre-Operative Evaluation ............................................................................................................................................. 14 5. Diagnosis (Category of Disease) ................................................................................................................................... 48 6. Procedure ..................................................................................................................................................................... 70 7. Post-Operative Events ................................................................................................................................................ 111 8. Discharge .................................................................................................................................................................... 135 9. Quality Measures ...................................................................................................................................................... -

The European Perspective on the Management of Acute Major Hemorrhage and Coagulopathy After Trauma: Summary of the 2019 Updated European Guideline
Journal of Clinical Medicine Article The European Perspective on the Management of Acute Major Hemorrhage and Coagulopathy after Trauma: Summary of the 2019 Updated European Guideline Marc Maegele Department of Traumatology and Orthopedic Surgery, Cologne-Merheim Medical Center (CMMC), Institute for Research in Operative Medicine (IFOM), University Witten-Herdecke, D-51109 Cologne, Germany; [email protected]; Tel.: +49-(0)-221-89-07-13-614; Fax: +49-(0)-221-89-07-30-85 Abstract: Non-controlled hemorrhage with accompanying trauma-induced coagulopathy (TIC) remains the most common cause of preventable death after multiple injury. Rapid identification followed by aggressive treatment is the key for improved outcomes. Treatment of trauma hemorrhage begins at the scene, with manual compression, the use of tourniquets and (non) commercial pelvic slings, and rapid transfer to an adequate trauma center. Upon hospital admission, coagulation monitoring and support are to be initiated immediately. Bleeding is controlled surgically following damage control principles. Modern coagulation management includes goal-oriented, individualized therapies, guided by point-of-care viscoelastic assays. Idarucizumab can be used as an antidote to the thrombin inhibitor dabigatran, andexanet alpha as an antidote to factor Xa inhibitors. This review summarizes the key recommendations of the 2019 updated European guideline on the management of major bleeding and coagulopathy following trauma. These evidence-based recommendations may form the backbone of algorithms adapted to local logistics and infrastructure. Keywords: trauma; hemorrhage; coagulopathgy; guideline Citation: Maegele, M. The European Perspective on the Management of Acute Major Hemorrhage and Coagulopathy after Trauma: 1. Introduction Summary of the 2019 Updated Despite significant improvements in acute trauma care, uncontrolled hemorrhage European Guideline. -

Bilateral Simultaneous Rupture of the Quadriceps Tendons in Healthy Individuals Takuro Moriya1,2* and Abe Yoshihiro1
Moriya et al. Trauma Cases Rev 2016, 2:043 Volume 2 | Issue 3 ISSN: 2469-5777 Trauma Cases and Reviews Case Report: Open Access Bilateral Simultaneous Rupture of the Quadriceps Tendons in Healthy Individuals Takuro Moriya1,2* and Abe Yoshihiro1 1Department of Orthopaedic Surgery, Chiba Rosai Hospital, Japan 2Department of Orthopaedic Surgery, Chiba Kaihin Municipal Hospital, Japan *Corresponding author: Takuro Moriya, Department of Orthopaedic Surgery, Chiba Rosai Hospital, 2-16 Tatsumidai- higashi, Ichihara 290-0003, Japan, Tel: +81-436-74-1111, Fax: +81-436-74-1151, E-mail: [email protected] Abstract Quadriceps tendon rupture is an uncommon injury in healthy individuals. This paper presents two case reports of patients of bilateral quadriceps tendon rupture, who were misdiagnosed as muscle weakness of quadriceps with contusion of the knee joint. Subsequent physical examination showed a supra-patellar gap, moderate hemarthrosis of both knees, and failure of active knee extension. MRI showed bilateral rupture of the quadriceps tendons at the osteotendinous junction. Radiographs described the depression in the suprapatellar soft tissue, patella baja and an avulsion bony fragment on the patella. Surgery confirmed the MRI observation, so transosseous suturing and augmentation were undertaken. Both patients returned to a normal life with useful function. Adequate physical examination and correct understanding of both radiograph and MRI were required to prevent misdiagnosis. Keywords Bilateral quadriceps tendon ruptures, Healthy individuals Figure 1: Suprapatellar gap in Case 1. Introduction avulsion fragment on the patella (Figure 3). The patellar heights of his right and left knees were 0.89 and 0.68, respectively, using the Insall- Rupture of the quadriceps tendon is an uncommon injury, and Saivati method. -
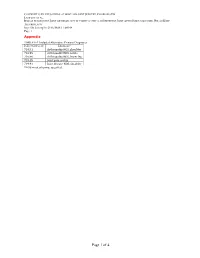
Page 1 of 4 COPYRIGHT © by the JOURNAL of BONE and JOINT SURGERY, INCORPORATED LAMPLOT ET AL
COPYRIGHT © BY THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED LAMPLOT ET AL. RISK OF SUBSEQUENT JOINT ARTHROPLASTY IN CONTRALATERAL OR DIFFERENT JOINT AFTER INDEX SHOULDER, HIP, OR KNEE ARTHROPLASTY http://dx.doi.org/10.2106/JBJS.17.00948 Page 1 Appendix TABLE E-1 Included Alternative Primary Diagnoses ICD-9-CM Code Diagnosis* 716.91 Arthropathy NOS, shoulder 716.95 Arthropathy NOS, pelvis 716.96 Arthropathy NOS, lower leg 719.45 Joint pain, pelvis 719.91 Joint disease NOS, shoulder *NOS = not otherwise specified. Page 1 of 4 COPYRIGHT © BY THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED LAMPLOT ET AL. RISK OF SUBSEQUENT JOINT ARTHROPLASTY IN CONTRALATERAL OR DIFFERENT JOINT AFTER INDEX SHOULDER, HIP, OR KNEE ARTHROPLASTY http://dx.doi.org/10.2106/JBJS.17.00948 Page 2 TABLE E-2 Excluded Diagnoses* ICD-9- ICD-9- ICD-9- ICD-9- CM Code Diagnosis CM Code Diagnosis CM Code Diagnosis CM Code Diagnosis 274 Gouty arthropathy NOS 696 Psoriatic 711.03 Pyogen 711.38 Dysenter arthropathy arthritis- arthritis NEC forearm 274.01 Acute gouty arthropathy 696.1 Other psoriasis 711.04 Pyogen 711.4 Bact arthritis- arthritis-hand unspec 274.02 Chr gouty arthropathy 696.2 Parapsoriasis 711.05 Pyogen 711.46 Bact arthritis- w/o tophi arthritis-pelvis l/leg 274.03 Chr gouty arthropathy w 696.3 Pityriasis rosea 711.06 Pyogen 711.5 Viral arthritis- tophi arthritis-l/leg unspec 274.1 Gouty nephropathy NOS 696.4 Pityriasis rubra 711.07 Pyogen 711.55 Viral arthritis- pilaris arthritis-ankle pelvis 274.11 Uric acid nephrolithiasis 696.5 Pityriasis NEC & 711.08