Pharmacotherapy for Urinary Bladder Dysfunction in Spinal Cord Injury Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The National Drugs List
^ ^ ^ ^ ^[ ^ The National Drugs List Of Syrian Arab Republic Sexth Edition 2006 ! " # "$ % &'() " # * +$, -. / & 0 /+12 3 4" 5 "$ . "$ 67"5,) 0 " /! !2 4? @ % 88 9 3: " # "$ ;+<=2 – G# H H2 I) – 6( – 65 : A B C "5 : , D )* . J!* HK"3 H"$ T ) 4 B K<) +$ LMA N O 3 4P<B &Q / RS ) H< C4VH /430 / 1988 V W* < C A GQ ") 4V / 1000 / C4VH /820 / 2001 V XX K<# C ,V /500 / 1992 V "!X V /946 / 2004 V Z < C V /914 / 2003 V ) < ] +$, [2 / ,) @# @ S%Q2 J"= [ &<\ @ +$ LMA 1 O \ . S X '( ^ & M_ `AB @ &' 3 4" + @ V= 4 )\ " : N " # "$ 6 ) G" 3Q + a C G /<"B d3: C K7 e , fM 4 Q b"$ " < $\ c"7: 5) G . HHH3Q J # Hg ' V"h 6< G* H5 !" # $%" & $' ,* ( )* + 2 ا اوا ادو +% 5 j 2 i1 6 B J' 6<X " 6"[ i2 "$ "< * i3 10 6 i4 11 6! ^ i5 13 6<X "!# * i6 15 7 G!, 6 - k 24"$d dl ?K V *4V h 63[46 ' i8 19 Adl 20 "( 2 i9 20 G Q) 6 i10 20 a 6 m[, 6 i11 21 ?K V $n i12 21 "% * i13 23 b+ 6 i14 23 oe C * i15 24 !, 2 6\ i16 25 C V pq * i17 26 ( S 6) 1, ++ &"r i19 3 +% 27 G 6 ""% i19 28 ^ Ks 2 i20 31 % Ks 2 i21 32 s * i22 35 " " * i23 37 "$ * i24 38 6" i25 39 V t h Gu* v!* 2 i26 39 ( 2 i27 40 B w< Ks 2 i28 40 d C &"r i29 42 "' 6 i30 42 " * i31 42 ":< * i32 5 ./ 0" -33 4 : ANAESTHETICS $ 1 2 -1 :GENERAL ANAESTHETICS AND OXYGEN 4 $1 2 2- ATRACURIUM BESYLATE DROPERIDOL ETHER FENTANYL HALOTHANE ISOFLURANE KETAMINE HCL NITROUS OXIDE OXYGEN PROPOFOL REMIFENTANIL SEVOFLURANE SUFENTANIL THIOPENTAL :LOCAL ANAESTHETICS !67$1 2 -5 AMYLEINE HCL=AMYLOCAINE ARTICAINE BENZOCAINE BUPIVACAINE CINCHOCAINE LIDOCAINE MEPIVACAINE OXETHAZAINE PRAMOXINE PRILOCAINE PREOPERATIVE MEDICATION & SEDATION FOR 9*: ;< " 2 -8 : : SHORT -TERM PROCEDURES ATROPINE DIAZEPAM INJ. -

Inline-Supplementary-Material-1.Pdf
Appendix 1: STOPP/START criteria version 2 applied to the TRUST dataset Physiological system Criteria Criteria included Number (%) (The relevant () criteria for each participant were applied to the dataset and recorded in of Microsoft Office Excel ® (2013)) criteria included out of total criteria STOPP criteria Indication of medication A1. Any drug prescribed without an evidence-based clinical indication. X 1/3 (33.3) A2. Any drug prescribed beyond the recommended duration, where treatment duration is X well defined. A3. Any duplicate drug class prescription e.g. two concurrent NSAIDs, SSRIs, loop diuretics, ACE inhibitors, anticoagulants (optimisation of monotherapy within a single drug class should be observed prior to considering a new agent). Cardiovascular system B1. Digoxin for heart failure with preserved systolic ventricular function (no clear evidence X 7/13 (53.8) of benefit). B2. Verapamil or diltiazem with NYHA Class III or IV heart failure (may worsen heart failure). B3. Beta-blocker in combination with verapamil or diltiazem (risk of heart block). B4. Beta blocker with symptomatic bradycardia (< 50/min), type II heart block or complete heart block (risk of profound hypotension, asystole). B5. Amiodarone as first-line antiarrhythmic therapy in supraventricular tachyarrhythmias X (higher risk of side-effects than beta-blockers, digoxin, verapamil or diltiazem). B6. Loop diuretic as first-line treatment for hypertension (safer, more effective alternatives available). B7. Loop diuretic for dependent ankle oedema without clinical, biochemical evidence or radiological evidence of heart failure, liver failure, nephrotic syndrome or renal failure (leg elevation and /or compression hosiery usually more appropriate). B8. Thiazide diuretic with current significant hypokalaemia (i.e. -

PDF Download
CURRENT THERAPEUTIC RESEARCH VOL. 56, NO. 5, MAY 1995 EFFECTS OF CEREBRAL METABOLIC ENHANCERS ON BRAIN FUNCTION IN RODENTS KOICHIRO TAKAHASHI,l MINORU YAMAMOTO,’ MASANORI SUZUKI,’ YUKIKO OZAWA,’ TAKASHI YAMAGUCHI,l HIROFUMI ANDOH, AND KOUICHI ISHIKAWA2 ‘Department of Pharmacology, Clinical Pharmacology Research Laboratory, Yamunouchi Pharmaceutical Co. Ltd., and ‘Department of Pharmacology, School of Medicine, Nihon University, Tokyo, Japan AFWI’RACT The effects of cerebral metabolic enhancers (indeloxazine, bi- femelane, idebenone, and nicergoline) on reserpine-induced hypother- mia, the immobility period in forced swimming tests, and passive avoidance learning behavior were compared with the effects of ami- triptyline in rodents. Indeloxazine, bifemelane, and amitriptyline antagonized hypothermia in mice given reserpine. Indeloxaxine and amitriptyline decreased the immobility period in mice in the forced swimming test in a dose-dependent manner. The latency of step- through in the passive avoidance test in rats was prolonged by ad- ministration of indeloxazine but shortened by administration of amitriptyline. Neither idebenone nor nicergoline displayed any phar- macologic action in these tests. The results suggest that indeloxaxine possesses an antidepressant activity similar to that of amitriptyline but differs from amitriptyline in its anticholinergic properties and its ability to ameliorate impaired brain function such as that of learning behavior. In addition, indeloxazine exhibited broader effects on brain functions than either bifemelane, idebenone, or nicergoline. INTRODUCTION Cerebral metabolic enhancers (drugs that enhance energy metabolism) including brain glucose and ATP levels such as indeloxazine,1*2 bi- femelane, 3*4idebenone?6 and nicergoline,7>8 are currently used for the treatment of patients with various psychiatric symptoms. These symptoms include reduced spontaneity and emotional disturbance in patients with cerebral vascular disease. -

Updatirg the Beers Criteria for Potentially Inappropriate Medication Use in Older Adults
Updatirg the BeersCriteria for Potentially InappropriateMedication Use in Older Adults Resultsof a US ConsensusPanel of Experts DonnaM.Fich,PhD,RN;lamesW.Cooper,PhD,RPh;WilliamE.Wade,PhannD,FASHP,FCCP; JenniJerL. Waller, PhD;J, RossMaclean, MD; Marh H. Beers,MD Bcckground: Medication toxic effectsand drug- Reruhr: This study identified 48 individual medica- relatedproblems can have profound medical and safety tions or classeso[ medicationsto avoid in older adults consequencesfor older adults and economically affect the and their potential concernsand 20 diseases/conditions health caresystem. The purpose of this initiative was to and medicationsto be avoidedin older adultswith these reviseand update the Beerscriteria for potentially inap- conditions.Of thesepotentially inappropriate drugs, 66 propriate medicationuse in adults 65 yearsand older in wereconsidered by the panelto haveadverse outcomes the United States. of high severity. lYlcthcdr: This study used a modified Delphi method, a Concludonr: This study is an importantupdate of pre- setof proceduresand methodsfor formulating a groupjudg- viously establishedcriteria that have been widely used ment for a subject matter in which precise information is and cited. The application of the Beerscriteria and other Iacking. The criteria reviewed covered 2 types of state- tools for identifying potentially inapproprlate medica- ments: (l) medicationsor medicationclasses that should tion use will continue to enableproviders to plan inter- grnerally be avoidedin persons 65 years or older because -

Local Product Document Pfizer Venezuela, S.A
LOCAL PRODUCT DOCUMENT PFIZER VENEZUELA, S.A. 1. MEDICINAL PRODUCT BRAND NAME ® SERMION 2. CUALITATIVE AND CUANTITATIVE COMPOSITION Every coated tablet contains 10 and 30 mg of Nicergoline. 3. PHARMACEUTICAL FORM Coated tablets. 4. CLINICAL PARTICULARS 4.1 THERAPEUTIC INDICATIONS 1. Cerebrovascular insufficiency of senile source. 2. Peripheral Vasodilator. 3. Treatment of Senile dementia from light to medium level of vascular type and Alzheimer. 4.2 DOSAGE 1. 30 mg/day and Cerebrovascular insufficiency of senile source. 2. 30 mg twice per day, as Peripheral Vasodilator and on treatment of Senile dementia from light to medium level of vascular type and Alzheimer. 4.3 CONTRAINDICATIONS Hypersensitivity to Nicergoline. 4.4 WARNINGS AND PRECAUTIONS Nicergoline, as other adrenergic blocking agents, may significantly reduce blood pressure (arterial hypotension) in some patients. Likewise, as other sympatholytic agents, it has been associated to different degrees of sexual impotence and libido reduction. Do not administer this product if pregnant, if pregnancy is suspected or during breast-feeding. 4.5 ADVERSE EFFECTS Drowsiness, cephalea, tiredness, constipation, pyrosis, vomiting, diarrhea, facial flushing, sexual impotence and libido reduction, uric acid and L.H increment. 5. PHARMACOLOGICAL PROPERTIES 5.1 Pharmacokinetics Properties A) Onset and Duration - Benign prostatic hypertrophy, intramuscular: 2 hours. - Two hours after a single 4-mg intramuscular injection, average peak and mean urinary flow rates increased by 50% and 77%, respectively. B) Drug Concentration Levels - ORAL: 1 to 1.5 hours. - Maximal blood levels are reached 1 to 1.5 hours after oral dosing. - The mean maximum plasma concentrations after daily administration of a 30-mg film-coated tablet and a 30-mg effervescent tablet solution are 88 ng/mL and 41 ng/mL, respectively). -

Non-Antibiotics, Efflux Pumps and Drug Resistance of Gram-Negative Rods
Polish Journal of Microbiology MINIREVIEW 2018, Vol. 67, No 2, 129–135 DOI: 10.21307/pjm-2018-017 Non-antibiotics, Efflux Pumps and Drug Resistance of Gram-negative Rods AGNIESZKA EWA LAUDY* Department of Pharmaceutical Microbiology, Medical University of Warsaw, Warsaw, Poland Submitted 24 March 2018, revised 29 March 2018, accepted 04 April 2018 Abstract Non-antibiotic medicinal products consist of drugs with diverse activity against bacteria. Many non-antibiotics demonstrate direct anti- bacterial activity against Gram-positive cocci. The activity observed against Gram-negative rods is much lower and non-antibiotics primarily from the following groups: non-steroidal anti-inflammatory drugs, cardiovascular and antidepressant medicinal products demonstrate this activity. It has been shown that the low activity of some non-antibiotics or the absence of activity against Gram-negative rods is related, among other things, to the extrusion of these compounds from bacterial cells by multi-drug resistance efflux pumps. Substrates for the resistance-nodulation-division efflux systems include the following non-antibiotics: salicylate, diclofenac, ibuprofen, mefenamic acid, naproxen, amitriptyline, alendronate sodium, nicergoline, and ticlopidine. In addition, interactions between non-antibiotics and multi-drug resistance efflux pumps have been observed. It has also been revealed that depending on the concentration, salicylate induces expression of multi-drug resistance efflux pumps in Escherichia coli, Salmonella enterica subsp. enterica serotype Typhimurium, and Burkholderia cenoce pacia. However, salicylate does not affect the expression of the resistance-nodulation-division efflux systems Stenotrophomonasin maltophilia and Acinetobacter baumannii. Most importantly, there were no effects of medicinal products containing some non-antibiotic active substances, except salicylate, as substrates of multi-drug resistance efflux pumps, on the induction of Gram-negative rod resistance to quinolones. -

The Role of Antispasmodics in Managing Irritable Bowel Syndrome
DOI: https://doi.org/10.22516/25007440.309 Review articles The role of antispasmodics in managing irritable bowel syndrome Valeria Atenea Costa Barney,1* Alan Felipe Ovalle Hernández.1 1 Internal Medicine and Gastroenterology specialist Abstract in San Ignacio University Hospital, Pontificia Universidad Javeriana, Bogotá, Colombia. Although antispasmodics are the cornerstone of treating irritable bowel syndrome, there are a number of an- tispasmodic medications currently available in Colombia. Since they are frequently used to treat this disease, *Correspondence: [email protected] we consider an evaluation of them to be important. ......................................... Received: 26/10/18 Keywords Accepted: 11/02/19 Antispasmodic, irritable bowel syndrome, pinaverium bromide, otilonium bromide, Mebeverin, trimebutine. INTRODUCTION consistency. The criteria must be met for three consecutive months prior to diagnosis and symptoms must have started Irritable bowel syndrome (IBS) is one of the most fre- a minimum of six months before diagnosis. (3, 4) quent chronic gastrointestinal functional disorders. It is There are no known structural or anatomical explanations characterized by recurrent abdominal pain associated with of the pathophysiology of IBS and its exact cause remains changes in the rhythm of bowel movements with either or unknown. Nevertheless, several mechanisms have been both constipation and diarrhea. Swelling and bloating are proposed. Altered gastrointestinal motility may contribute frequent occurrences. (1) to changes in bowel habits reported by some patients, and a IBS is divided into two subtypes: predominance of cons- combination of smooth muscle spasms, visceral hypersen- tipation (20-30% of patients) and predominance of dia- sitivity and abnormalities of central pain processing may rrhea (20-30% of patients). -

4 Supplementary File
Supplemental Material for High-throughput screening discovers anti-fibrotic properties of Haloperidol by hindering myofibroblast activation Michael Rehman1, Simone Vodret1, Luca Braga2, Corrado Guarnaccia3, Fulvio Celsi4, Giulia Rossetti5, Valentina Martinelli2, Tiziana Battini1, Carlin Long2, Kristina Vukusic1, Tea Kocijan1, Chiara Collesi2,6, Nadja Ring1, Natasa Skoko3, Mauro Giacca2,6, Giannino Del Sal7,8, Marco Confalonieri6, Marcello Raspa9, Alessandro Marcello10, Michael P. Myers11, Sergio Crovella3, Paolo Carloni5, Serena Zacchigna1,6 1Cardiovascular Biology, 2Molecular Medicine, 3Biotechnology Development, 10Molecular Virology, and 11Protein Networks Laboratories, International Centre for Genetic Engineering and Biotechnology (ICGEB), Padriciano, 34149, Trieste, Italy 4Institute for Maternal and Child Health, IRCCS "Burlo Garofolo", Trieste, Italy 5Computational Biomedicine Section, Institute of Advanced Simulation IAS-5 and Institute of Neuroscience and Medicine INM-9, Forschungszentrum Jülich GmbH, 52425, Jülich, Germany 6Department of Medical, Surgical and Health Sciences, University of Trieste, 34149 Trieste, Italy 7National Laboratory CIB, Area Science Park Padriciano, Trieste, 34149, Italy 8Department of Life Sciences, University of Trieste, Trieste, 34127, Italy 9Consiglio Nazionale delle Ricerche (IBCN), CNR-Campus International Development (EMMA- INFRAFRONTIER-IMPC), Rome, Italy This PDF file includes: Supplementary Methods Supplementary References Supplementary Figures with legends 1 – 18 Supplementary Tables with legends 1 – 5 Supplementary Movie legends 1, 2 Supplementary Methods Cell culture Primary murine fibroblasts were isolated from skin, lung, kidney and hearts of adult CD1, C57BL/6 or aSMA-RFP/COLL-EGFP mice (1) by mechanical and enzymatic tissue digestion. Briefly, tissue was chopped in small chunks that were digested using a mixture of enzymes (Miltenyi Biotec, 130- 098-305) for 1 hour at 37°C with mechanical dissociation followed by filtration through a 70 µm cell strainer and centrifugation. -
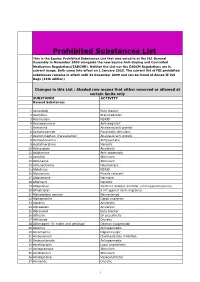
Prohibited Substances List
Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). Neither the List nor the EADCM Regulations are in current usage. Both come into effect on 1 January 2010. The current list of FEI prohibited substances remains in effect until 31 December 2009 and can be found at Annex II Vet Regs (11th edition) Changes in this List : Shaded row means that either removed or allowed at certain limits only SUBSTANCE ACTIVITY Banned Substances 1 Acebutolol Beta blocker 2 Acefylline Bronchodilator 3 Acemetacin NSAID 4 Acenocoumarol Anticoagulant 5 Acetanilid Analgesic/anti-pyretic 6 Acetohexamide Pancreatic stimulant 7 Acetominophen (Paracetamol) Analgesic/anti-pyretic 8 Acetophenazine Antipsychotic 9 Acetylmorphine Narcotic 10 Adinazolam Anxiolytic 11 Adiphenine Anti-spasmodic 12 Adrafinil Stimulant 13 Adrenaline Stimulant 14 Adrenochrome Haemostatic 15 Alclofenac NSAID 16 Alcuronium Muscle relaxant 17 Aldosterone Hormone 18 Alfentanil Narcotic 19 Allopurinol Xanthine oxidase inhibitor (anti-hyperuricaemia) 20 Almotriptan 5 HT agonist (anti-migraine) 21 Alphadolone acetate Neurosteriod 22 Alphaprodine Opiod analgesic 23 Alpidem Anxiolytic 24 Alprazolam Anxiolytic 25 Alprenolol Beta blocker 26 Althesin IV anaesthetic 27 Althiazide Diuretic 28 Altrenogest (in males and gelidngs) Oestrus suppression 29 Alverine Antispasmodic 30 Amantadine Dopaminergic 31 Ambenonium Cholinesterase inhibition 32 Ambucetamide Antispasmodic 33 Amethocaine Local anaesthetic 34 Amfepramone Stimulant 35 Amfetaminil Stimulant 36 Amidephrine Vasoconstrictor 37 Amiloride Diuretic 1 Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). -
![Pharmacological and Ionic Characterizations of the Muscarinic Receptors Modulating [3H]Acetylcholine Release from Rat Cortical Synaptosomes’](https://docslib.b-cdn.net/cover/3023/pharmacological-and-ionic-characterizations-of-the-muscarinic-receptors-modulating-3h-acetylcholine-release-from-rat-cortical-synaptosomes-753023.webp)
Pharmacological and Ionic Characterizations of the Muscarinic Receptors Modulating [3H]Acetylcholine Release from Rat Cortical Synaptosomes’
0270.6474/85/0505-1202$02.00/O The Journal of Neuroscience CopyrIght 0 Society for Neuroscrence Vol. 5, No. 5, pp. 1202-1207 Printed in U.S.A. May 1985 Pharmacological and Ionic Characterizations of the Muscarinic Receptors Modulating [3H]Acetylcholine Release from Rat Cortical Synaptosomes’ EDWIN M. MEYER* AND DEBORAH H. OTERO Department of Pharmacology and Therapeutics, University of Florida School of Medicine, Gainesville, Florida 32610 Abstract brain (Gonzales and Crews, 1984). M,-receptors, however, appear pre- and postsynaptically in brain, are regulated by an intrinsic The muscarinic receptors that modulate acetylcholine membrane protein that binds to GTP (g-protein), and may not be release from rat cortical synaptosomes were characterized coupled to changes in phosphatidylinositol turnover. with respect to sensitivity to drugs that act selectively at M, The present studies were designed to determine whether M,- or or Ma receptor subtypes, as well as to changes in ionic Mp-receptors mediate the presynaptic modulation of ACh release. strength and membrane potential. The modulatory receptors These studies involve dose-response curves for the release of appear to be of the M2 type, since they are activated by synaptosomal [3H]ACh in the presence of selected muscarinic ago- carbachol, acetylcholine, methacholine, oxotremorine, and nists and antagonists, as well as treatments that selectively alter MI- bethanechol, but not by pilocarpine, and are blocked by or M,-receptor activity. Our results indicate that the presynaptic atropine, scopolamine, and gallamine (at high concentra- modulation of [3H]ACh release is mediated by MP- but not MI- tions), but not by pirenzepine or dicyclomine. -

Supplemental Table 1: Patient Characteristics, Interventions and Definitions/Variables of Persistence, Adherence and Discontinuation Reported in the Studies
Adherence and persistence to OAB medication Supplemental Table 1: Patient characteristics, interventions and definitions/variables of persistence, adherence and discontinuation reported in the studies. Author (year) and Definition of persistence/adherence/discontinuation and Length of country (database) Participants Drug/intervention* independent variables on persistence follow-up Brostrøm and Hallas n=2477 Any prescription of OAB Patients who continued taking a particular drug for up to 7 years with Up to 7 (2009)1 Male: n=836 (33.8%) medication: no more than 120-day gaps were regarded as experiencing single- years Odense University Female: n=1641 (66.2%) flavoxate (n=21) treatment episodes Pharmacoepidemio- Mean age: 68.3 yearsa oxybutynin TD (n=48) logical Database tolterodine (n=1478) Variables: age, gender, prior use of OAB agents and use of (OPED); Denmark) solifenacin (n=774) anti-diabetic drugs (1999–2006) trospium (n=271) darifenacin (n=52) Chancellor et al (2013)2 n=103 250 First (new) prescription of OAB To be considered a discontinuation, patients were required to have a 2 years IMS Lifelink Database, Male: n≈25 916a (25.1%) medication in adults ≥18 years: gap of at least 45 days in therapy based on fill dates and days’ Connecticut; USA Female: n≈77 334a (74.9%) tolterodine ER (n=43 881)a supply (2005–2008) Mean (SD) age: 58.7 (15.7) solifenacin (n=15 488)a years oxybutynin (n=15 075)a Adherence rate was defined as the proportion of patients filling more darifenacin (n=10 532)a than one prescription with an MPR of ≥80% oxybutynin -

BETHANECHOL CHLORIDE TABLETS, USP5 Mg, 10 Mg, 25 Mg
BETHANECHOL CHLORIDE- bethanechol chloride tablet Upsher-Smith Laboratories, LLC ---------- BETHANECHOL CHLORIDE TABLETS, USP 5 mg, 10 mg, 25 mg and 50 mg Rx only DESCRIPTION Bethanechol chloride, USP, a cholinergic agent, is a synthetic ester which is structurally and pharmacologically related to acetylcholine. It is designated chemically as 2-[(aminocarbonyl)oxy]-N, N, N-trimethyl-1-propanaminium chloride. Its molecular formula is C7H17ClN2O2 and its structural formula is: It is a white, hygroscopic crystalline powder having a slight amine-like odor, freely soluble in water, and has a molecular weight of 196.68. Each tablet for oral administration contains 5 mg, 10 mg, 25 mg or 50 mg bethanechol chloride, USP. Tablets also contain the following inactive ingredients: colloidal silicon dioxide, lactose monohydrate, magnesium stearate, microcrystalline cellulose, sodium starch glycolate, (25 mg and 50 mg) D&C Yellow #10 Lake and FD&C Yellow #6 Lake. CLINICAL PHARMACOLOGY Bethanechol chloride acts principally by producing the effects of stimulation of the parasympathetic nervous system. It increases the tone of the detrusor urinae muscle, usually producing a contraction sufficiently strong to initiate micturition and empty the bladder. It stimulates gastric motility, increases gastric tone and often restores impaired rhythmic peristalsis. Stimulation of the parasympathetic nervous system releases acetylcholine at the nerve endings. When spontaneous stimulation is reduced and therapeutic intervention is required, acetylcholine can be given, but it is rapidly hydrolyzed by cholinesterase and its effects are transient. Bethanechol chloride is not destroyed by cholinesterase and its effects are more prolonged than those of acetylcholine. Effects on the GI and urinary tracts sometimes appear within 30 minutes after oral administration of bethanechol chloride, but more often 60 to 90 minutes are required to reach maximum effectiveness.