The Role of Efflux Pumps in the Transition from Low-Level To
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Principles of Drug Addiction Treatment: a Research-Based Guide (Third Edition)
Publications Revised January 2018 Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition) Table of Contents Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition) Preface Principles of Effective Treatment Frequently Asked Questions Drug Addiction Treatment in the United States Evidence-Based Approaches to Drug Addiction Treatment Acknowledgments Resources Page 1 Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition) The U.S. Government does not endorse or favor any specific commercial product or company. Trade, proprietary, or company names appearing in this publication are used only because they are considered essential in the context of the studies described. Preface Drug addiction is a complex illness. It is characterized by intense and, at times, uncontrollable drug craving, along with compulsive drug seeking and use that persist even in the face of devastating consequences. This update of the National Institute on Drug Abuse’s Principles of Drug Addiction Treatment is intended to address addiction to a wide variety of drugs, including nicotine, alcohol, and illicit and prescription drugs. It is designed to serve as a resource for healthcare providers, family members, and other stakeholders trying to address the myriad problems faced by patients in need of treatment for drug abuse or addiction. Addiction affects multiple brain circuits, including those involved in reward and motivation, learning and memory, and inhibitory control over behavior. That is why addiction is a brain disease. Some individuals are more vulnerable than others to becoming addicted, depending on the interplay between genetic makeup, age of exposure to drugs, and other environmental influences. -

Natural Products As Alternative Choices for P-Glycoprotein (P-Gp) Inhibition
Review Natural Products as Alternative Choices for P-Glycoprotein (P-gp) Inhibition Saikat Dewanjee 1,*, Tarun K. Dua 1, Niloy Bhattacharjee 1, Anup Das 2, Moumita Gangopadhyay 3, Ritu Khanra 1, Swarnalata Joardar 1, Muhammad Riaz 4, Vincenzo De Feo 5,* and Muhammad Zia-Ul-Haq 6,* 1 Advanced Pharmacognosy Research Laboratory, Department of Pharmaceutical Technology, Jadavpur University, Raja S C Mullick Road, Kolkata 700032, India; [email protected] (T.K.D.); [email protected] (N.B.); [email protected] (R.K.); [email protected] (S.J.) 2 Department of Pharmaceutical Technology, ADAMAS University, Barasat, Kolkata 700126, India; [email protected] 3 Department of Bioechnology, ADAMAS University, Barasat, Kolkata 700126, India; [email protected] 4 Department of Pharmacy, Shaheed Benazir Bhutto University, Sheringal 18050, Pakistan; [email protected] 5 Department of Pharmacy, Salerno University, Fisciano 84084, Salerno, Italy 6 Environment Science Department, Lahore College for Women University, Jail Road, Lahore 54600, Pakistan * Correspondence: [email protected] (S.D.); [email protected] (V.D.F.); [email protected] (M.Z.-U.-H.) Academic Editor: Maria Emília de Sousa Received: 11 April 2017; Accepted: 15 May 2017; Published: 25 May 2017 Abstract: Multidrug resistance (MDR) is regarded as one of the bottlenecks of successful clinical treatment for numerous chemotherapeutic agents. Multiple key regulators are alleged to be responsible for MDR and making the treatment regimens ineffective. In this review, we discuss MDR in relation to P-glycoprotein (P-gp) and its down-regulation by natural bioactive molecules. P-gp, a unique ATP-dependent membrane transport protein, is one of those key regulators which are present in the lining of the colon, endothelial cells of the blood brain barrier (BBB), bile duct, adrenal gland, kidney tubules, small intestine, pancreatic ducts and in many other tissues like heart, lungs, spleen, skeletal muscles, etc. -

Cell Volume Change Through Water Efflux Impacts Cell Stiffness And
Cell volume change through water efflux impacts cell PNAS PLUS stiffness and stem cell fate Ming Guoa,1, Adrian F. Pegoraroa, Angelo Maoa,b, Enhua H. Zhouc,2, Praveen R. Aranyd,e, Yulong Hana,f, Dylan T. Burnetteg, Mikkel H. Jensena,h, Karen E. Kaszaa,i, Jeffrey R. Moorej, Frederick C. Mackintoshk,l,m, Jeffrey J. Fredbergc, David J. Mooneya,b, Jennifer Lippincott-Schwartzn,3, and David A. Weitza,o,3 aJohn A. Paulson School of Engineering and Applied Sciences, Harvard University, Cambridge, MA 02138; bWyss Institute for Biologically Inspired Engineering, Harvard University, Cambridge, MA 02138; cHarvard T. H. Chan School of Public Health, Boston, MA 02115; dDepartment of Oral Biology, University at Buffalo, Buffalo, NY 14214; eDepartment of Biomedical Engineering, University at Buffalo, Buffalo, NY 14214; fBiomedical Engineering and Biomechanics Center, Xi’an Jiaotong University, Xi’an 710049, China; gDepartment of Cell and Developmental Biology, Vanderbilt University School of Medicine, Nashville, TN 37232; hDepartment of Physics and Astronomy, California State University, Sacramento, CA 95819; iDepartment of Mechanical Engineering, Columbia University, New York, NY 10027; jDepartment of Biological Sciences, University of Massachusetts at Lowell, Lowell, MA 01854; kDepartment of Physics and Astronomy, VU University, 1081 HV Amsterdam, The Netherlands; lDepartment of Chemical and Biomolecular Engineering, Rice University, Houston, TX 77030; mCenter for Theoretical Biophysics, Rice University, Houston, TX 77030; nHoward Hughes Medical Institute, Janelia Research Campus, Ashburn, VA 20147; and oDepartment of Physics, Harvard University, Cambridge, MA 02138 Contributed by Jennifer Lippincott-Schwartz, August 26, 2017 (sent for review March 29, 2017; reviewed by Daniel A. Fletcher and Valerie M. -

Involvement of Multiple Influx and Efflux Transporters in the Accumulation of Cationic Fluorescent Dyes by Escherichia Coli Srijan Jindal1,2,3, Lei Yang4, Philip J
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Liverpool Repository Jindal et al. BMC Microbiology (2019) 19:195 https://doi.org/10.1186/s12866-019-1561-0 RESEARCH ARTICLE Open Access Involvement of multiple influx and efflux transporters in the accumulation of cationic fluorescent dyes by Escherichia coli Srijan Jindal1,2,3, Lei Yang4, Philip J. Day2,3 and Douglas B. Kell1,2,4,5* Abstract Background: It is widely believed that most xenobiotics cross biomembranes by diffusing through the phospholipid bilayer, and that the use of protein transporters is an occasional adjunct. According to an alternative view, phospholipid bilayer transport is negligible, and several different transporters may be involved in the uptake of an individual molecular type. We recognise here that the availability of gene knockout collections allows one to assess the contributions of all potential transporters, and flow cytometry based on fluorescence provides a convenient high-throughput assay for xenobiotic uptake in individual cells. Results: We used high-throughput flow cytometry to assess the ability of individual gene knockout strains of E coli to take up two membrane-permeable, cationic fluorescent dyes, namely the carbocyanine diS-C3(5) and the DNA dye SYBR Green. Individual strains showed a large range of distributions of uptake. The range of modal steady-state uptakes for the carbocyanine between the different strains was 36-fold. Knockouts of the ATP synthase α- and β- subunits greatly inhibited uptake, implying that most uptake was ATP-driven rather than being driven by a membrane potential. -

Behavioral Tolerance: Research and Treatment Implications
US DEPARTMENT OF HEALTH EDUCATION AND WELFARE • Public Health Service • Alcohol Drug Abuse and Mental Health Administration Behavioral Tolerance: Research and Treatment Implications Editor: Norman A. Krasnegor, Ph.D. NIDA Research Monograph 18 January 1978 DEPARTMENT OF HEALTH, EDUCATION, AND WELFARE Public Health Service Alcohol, Drug Abuse, and Mental Health Administration National lnstitute on Drug Abuse Division of Research 5600 Fishers Lane RockviIle. Maryland 20657 For sale by tho Superintendent of Documents, U.S. Government Printing Office Washington, D.C. 20402 (Paper Cover) Stock No. 017-024-00699-8 The NIDA Research Monogroph series iS prepared by the Division of Research of the National Institute on Drug Abuse Its primary objective is to provide critical re- views of research problem areas and techniques. the content of state-of-the-art conferences, integrative research reviews and significant original research its dual publication emphasis iS rapid and targeted dissemination to the scientific and professional community Editorial Advisory Board Avram Goldstein, M.D Addiction Research Foundation Polo Alto California Jerome Jaffe, M.D College Of Physicians and Surgeons Columbia University New York Reese T Jones, M.D Langley Porter Neuropsychitnc Institute University of California San Francisco California William McGlothlin, Ph D Department of Psychology UCLA Los Angeles California Jack Mendelson. M D Alcohol and Drug Abuse Research Center Harvard Medical School McLeon Hospital Belmont Massachusetts Helen Nowlis. Ph.D Office of Drug Education DHEW Washington DC Lee Robins, Ph.D Washington University School of Medicine St Louis Missouri NIDA Research Monograph series Robert DuPont, M.D. DIRECTOR, NIDA William Pollin, M.D. DIRECTOR, DIVISION OF RESEARCH, NIDA Robert C. -

Pharmacology - Neuroadaptation
Pharmacology - Neuroadaptation All drugs of dependence are associated with increased dopamine activity in the so-called reward pathway of the brain-- this pathway that gives us pleasure and tells us what's good for our survival. The overstimulation of the reward system when we use drugs of abuse, or develop an addiction, sets in motion a reinforcing pattern that teaches us to repeat the behaviour. Over time, as drug use and addiction continues and develops, the brain adapts to the overwhelming surges in dopamine. And it adapts by producing less dopamine, by reducing the number and activity of the dopamine receptors, and by essentially turning down the volume on the dopamine system. Our brain strives for balance. In some respects, we can conceptualise it as constantly adapting and changing to function in a way that we can act and feel normal, a process called homeostasis. And when we talk about homeostasis occurring in the brain, we use the term neuroadaptation. When we consume a drug, we alter the functioning of our brain. We upset the balance, and as a result, our brain tries to adapt. It tries to minimise the effect of the drug and get back to normal. If we use a drug frequently, then the brain will adapt to try and be in balance when the drug is present. But if we then stop taking the drug, our brain is no longer in balance, and it can take a really long time for the brain to re-adapt. In psychopharmacology, we refer to these processes as drug tolerance and physical drug dependence. -

Biological Components of Substance Abuse and Addiction
Biological Components of Substance Abuse and Addiction September 1993 OTA-BP-BBS-117 NTIS order #PB94-134624 GPO stock #052-003-01350-9 Recommended Citation: U.S. Congress, Mice of Technology Assessment, BioZogicaZ Components of Substance Abuse and Addiction, OTA-BP-BBS-1 17 (Washington, DC: U.S. Government printing Offke, September 1993). II 10[ \cllc h> 111( I Is ( l(l\ c1 Illllclll 1’1 Illllllp ( )Illcc $L1pCrlfl[L’llL! L’11[ of [)(). UIIIC’111.. \lJl[ $[t~[~ \\( )1’ \\ J.hlllg({lll. [)( ?( l~()? ‘~ ~?h ISBN 0-16 -042096-2 Foreword ubstance abuse and addiction are complex phenomena that defy simple explanation or description. A tangled interaction of factors contributes to an individual’s experimentation with, use, and perhaps subsequent abuse of drugs. Regardless of the mix of contributing factors, the actions and effectss exerted by drugs of abuse underlie all substance abuse and addiction. In order to understand substance abuse and addiction it is first necessary to understand how drugs work in the brain, why certain drugs have the potential for being abused, and what, if any, biological differences exist among individuals in their susceptibility to abuse drugs. This background paper is the first of two documents being produced by OTA as part of an assessment of Technologies for Understanding the Root Causes of Substance Abuse and Addiction. The assessment was requested by the House Committee on Government Operations, the Senate Committee on Governmental Affairs, and the Senate Committee on Labor and Human Resources. This background paper describes biological contributing factors to substance abuse and addiction. The second document being produced by this study will discuss the complex interactions of biochemical, physiological, psychological, and sociological factors leading to substance abuse and addiction. -

Pharmacogenomics: the Promise of Personalized Medicine for CNS Disorders
Neuropsychopharmacology REVIEWS (2009) 34, 159–172 & 2009 Nature Publishing Group All rights reserved 0893-133X/09 $30.00 REVIEW ............................................................................................................................................................... www.neuropsychopharmacology.org 159 Pharmacogenomics: The Promise of Personalized Medicine for CNS Disorders Jose de Leon*,1,2,3,4 1 2 Mental Health Research Center, Eastern State Hospital, University of Kentucky, Lexington, KY, USA; College of Medicine, 3 4 University of Kentucky, Lexington, KY, USA; College of Pharmacy, University of Kentucky, Lexington, KY, USA; Psychiatry and Neurosciences Research Group (CTS-549), Institute of Neurosciences, Medical School, University of Granada, Granada, Spain This review focuses first on the concept of pharmacogenomics and its related concepts (biomarkers and personalized prescription). Next, the first generation of five DNA pharmacogenomic tests used in the clinical practice of psychiatry is briefly reviewed. Then the possible involvement of these pharmacogenomic tests in the exploration of early clinical proof of mechanism is described by using two of the tests and one example from the pharmaceutical industry (iloperidone clinical trials). The initial attempts to use other microarray tests (measuring RNA expression) as peripheral biomarkers for CNS disorders are briefly described. Then the challenge of taking pharmacogenomic tests (compared to drugs) into clinical practice is explained by focusing on regulatory -

Blood-Brain Barrier Active Efflux Transporters
NeuroRx: The Journal of the American Society for Experimental NeuroTherapeutics Blood-Brain Barrier Active Efflux Transporters: ATP-Binding Cassette Gene Family Wolfgang Lo¨scher and Heidrun Potschka Department of Pharmacology, Toxicology, and Pharmacy, University of Veterinary Medicine Hannover, Hannover D-30559, Germany Summary: The blood-brain barrier (BBB) contributes to brain efflux transporters in the BBB include minimizing or avoiding homeostasis by protecting the brain from potentially harmful neurotoxic adverse effects of drugs that otherwise would pen- endogenous and exogenous substances. BBB active drug efflux etrate into the brain. However, ABC efflux transporters may transporters of the ATP-binding cassette (ABC) gene family also limit the central distribution of drugs that are beneficial to are increasingly recognized as important determinants of drug treat CNS diseases. Furthermore, neurological disorders such distribution to, and elimination from, the CNS. The ABC efflux as epilepsy may be associated with overexpression of ABC transporter P-glycoprotein (Pgp) has been demonstrated as a efflux transporters at the BBB, resulting in pharmacoresistance key element of the BBB that can actively transport a huge to therapeutic medication. Therefore, modulation of ABC ef- variety of lipophilic drugs out of the brain capillary endothelial flux transporters at the BBB forms a novel strategy to enhance cells that form the BBB. In addition to Pgp, other ABC efflux the penetration of drugs into the brain and may yield new transporters such as members of the multidrug resistance pro- therapeutic options for drug-resistant CNS diseases. Key tein (MRP) family and breast cancer resistance protein (BCRP) Words: P-glycoprotein, multidrug resistance proteins, epi- seem to contribute to BBB function. -

Prescription Drug Abuse See Page 10
Preventing and recognizing prescription drug abuse See page 10. from the director: The nonmedical use and abuse of prescription drugs is a serious public health problem in this country. Although most people take prescription medications responsibly, an estimated 52 million people (20 percent of those aged 12 and Prescription older) have used prescription drugs for nonmedical reasons at least once in their lifetimes. Young people are strongly represented in this group. In fact, the National Institute on Drug Abuse’s (NIDA) Drug Abuse Monitoring the Future (MTF) survey found that about 1 in 12 high school seniors reported past-year nonmedical use of the prescription pain reliever Vicodin in 2010, and 1 in 20 reported abusing OxyContin—making these medications among the most commonly abused drugs by adolescents. The abuse of certain prescription drugs— opioids, central nervous system (CNS) depressants, and stimulants—can lead to a variety of adverse health effects, including addiction. Among those who reported past-year nonmedical use of a prescription drug, nearly 14 percent met criteria for abuse of or dependence on it. The reasons for the high prevalence of prescription drug abuse vary by age, gender, and other factors, but likely include greater availability. What is The number of prescriptions for some of these medications has increased prescription dramatically since the early 1990s (see figures, page 2). Moreover, a consumer culture amenable to “taking a pill for drug abuse? what ails you” and the perception of 1 prescription drugs as less harmful than rescription drug abuse is the use of a medication without illicit drugs are other likely contributors a prescription, in a way other than as prescribed, or for to the problem. -
Pharmacogenomic Testing Panels for Major Depressive Disorder
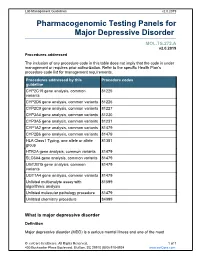
Lab Management Guidelines v2.0.2019 Pharmacogenomic Testing Panels for Major Depressive Disorder MOL.TS.272.A v2.0.2019 Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline CYP2C19 gene analysis, common 81225 variants CYP2D6 gene analysis, common variants 81226 CYP2C9 gene analysis, common variants 81227 CYP3A4 gene analysis, common variants 81230 CYP3A5 gene analysis, common variants 81231 CYP1A2 gene analysis, common variants 81479 CYP2B6 gene analysis, common variants 81479 HLA Class I Typing, one allele or allele 81381 group HTR2A gene analysis, common variants 81479 SLC6A4 gene analysis, common variants 81479 UGT2B15 gene analysis, common 81479 variants UGT1A4 gene analysis, common variants 81479 Unlisted multianalyte assay with 81599 algorithmic analysis Unlisted molecular pathology procedure 81479 Unlisted chemistry procedure 84999 What is major depressive disorder Definition Major depressive disorder (MDD) is a serious mental illness and one of the most © eviCore healthcare. All Rights Reserved. 1 of 7 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines v2.0.2019 common mental disorders in the United States, carrying the heaviest burden of disability among all mental and behavioral disorders. In 2016, roughly 16 million adults in the United States experienced at least one major depression episode in the previous year; this number represented 6.7% of all adults in the United States.1 A major depressive episode can include a number of symptoms, including depressed mood, insomnia or hypersomnia, change in appetite or weight, low energy, poor concentration, and recurrent thoughts of death or suicide, among other symptoms. -

Targeting the Zinc Transporter ZIP7 in the Treatment of Insulin Resistance and Type 2 Diabetes
nutrients Review Targeting the Zinc Transporter ZIP7 in the Treatment of Insulin Resistance and Type 2 Diabetes John Adulcikas, Sabrina Sonda, Shaghayegh Norouzi, Sukhwinder Singh Sohal and Stephen Myers * College of Health and Medicine, School of Health Sciences, University of Tasmania, TAS 7005, Australia; [email protected] (J.A.); [email protected] (S.S.); [email protected] (S.N.); [email protected] (S.S.S.) * Correspondence: [email protected]; Tel.: +61-3-6324-5459 Received: 20 December 2018; Accepted: 12 February 2019; Published: 15 February 2019 Abstract: Type 2 diabetes mellitus (T2DM) is a disease associated with dysfunctional metabolic processes that lead to abnormally high levels of blood glucose. Preceding the development of T2DM is insulin resistance (IR), a disorder associated with suppressed or delayed responses to insulin. The effects of this response are predominately mediated through aberrant cell signalling processes and compromised glucose uptake into peripheral tissue including adipose, liver and skeletal muscle. Moreover, a major factor considered to be the cause of IR is endoplasmic reticulum (ER) stress. This subcellular organelle plays a pivotal role in protein folding and processes that increase ER stress, leads to maladaptive responses that result in cell death. Recently, zinc and the proteins that transport this metal ion have been implicated in the ER stress response. Specifically, the ER-specific zinc transporter ZIP7, coined the “gate-keeper” of zinc release from the ER into the cytosol, was shown to be essential for maintaining ER homeostasis in intestinal epithelium and myeloid leukaemia cells. Moreover, ZIP7 controls essential cell signalling pathways similar to insulin and activates glucose uptake in skeletal muscle.