CAGI Sickkids Challenges: Assessment of Phenotype and Variant Predictions Derived from Clinical and Genomic Data of Children with Undiagnosed Diseases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Applied Category Theory for Genomics – an Initiative
Applied Category Theory for Genomics { An Initiative Yanying Wu1,2 1Centre for Neural Circuits and Behaviour, University of Oxford, UK 2Department of Physiology, Anatomy and Genetics, University of Oxford, UK 06 Sept, 2020 Abstract The ultimate secret of all lives on earth is hidden in their genomes { a totality of DNA sequences. We currently know the whole genome sequence of many organisms, while our understanding of the genome architecture on a systematic level remains rudimentary. Applied category theory opens a promising way to integrate the humongous amount of heterogeneous informations in genomics, to advance our knowledge regarding genome organization, and to provide us with a deep and holistic view of our own genomes. In this work we explain why applied category theory carries such a hope, and we move on to show how it could actually do so, albeit in baby steps. The manuscript intends to be readable to both mathematicians and biologists, therefore no prior knowledge is required from either side. arXiv:2009.02822v1 [q-bio.GN] 6 Sep 2020 1 Introduction DNA, the genetic material of all living beings on this planet, holds the secret of life. The complete set of DNA sequences in an organism constitutes its genome { the blueprint and instruction manual of that organism, be it a human or fly [1]. Therefore, genomics, which studies the contents and meaning of genomes, has been standing in the central stage of scientific research since its birth. The twentieth century witnessed three milestones of genomics research [1]. It began with the discovery of Mendel's laws of inheritance [2], sparked a climax in the middle with the reveal of DNA double helix structure [3], and ended with the accomplishment of a first draft of complete human genome sequences [4]. -

Functional Effects Detailed Research Plan
GeCIP Detailed Research Plan Form Background The Genomics England Clinical Interpretation Partnership (GeCIP) brings together researchers, clinicians and trainees from both academia and the NHS to analyse, refine and make new discoveries from the data from the 100,000 Genomes Project. The aims of the partnerships are: 1. To optimise: • clinical data and sample collection • clinical reporting • data validation and interpretation. 2. To improve understanding of the implications of genomic findings and improve the accuracy and reliability of information fed back to patients. To add to knowledge of the genetic basis of disease. 3. To provide a sustainable thriving training environment. The initial wave of GeCIP domains was announced in June 2015 following a first round of applications in January 2015. On the 18th June 2015 we invited the inaugurated GeCIP domains to develop more detailed research plans working closely with Genomics England. These will be used to ensure that the plans are complimentary and add real value across the GeCIP portfolio and address the aims and objectives of the 100,000 Genomes Project. They will be shared with the MRC, Wellcome Trust, NIHR and Cancer Research UK as existing members of the GeCIP Board to give advance warning and manage funding requests to maximise the funds available to each domain. However, formal applications will then be required to be submitted to individual funders. They will allow Genomics England to plan shared core analyses and the required research and computing infrastructure to support the proposed research. They will also form the basis of assessment by the Project’s Access Review Committee, to permit access to data. -

Novel Association of Hypertrophic Cardiomyopathy, Sensorineural Deafness, and a Mutation in Unconventional Myosin VI (MYO6)
309 LETTER TO JMG J Med Genet: first published as 10.1136/jmg.2003.011973 on 1 April 2004. Downloaded from Novel association of hypertrophic cardiomyopathy, sensorineural deafness, and a mutation in unconventional myosin VI (MYO6) S A Mohiddin, Z M Ahmed, A J Griffith, D Tripodi, T B Friedman, L Fananapazir, R J Morell ............................................................................................................................... J Med Genet 2004;41:309–314. doi: 10.1136/jmg.2003.011973 amilial hypertrophic cardiomyopathy (FHC) is typically Key points characterised by left ventricular hypertrophy, diastolic Fdysfunction, and hypercontractility, and is often asso- ciated with disabling symptoms, arrhythmias, and sudden N Familial hypertrophic cardiomyopathy (FHC) is typi- death.1 FHC shows both non-allelic and allelic genetic cally confined to a cardiac phenotype and is caused by heterogeneity, and results from any one of more than 100 mutations in genes encoding sarcomeric proteins. mutations in genes encoding sarcomeric proteins.2 Identified Occasionally FHC may be one component of a genes include those encoding b myosin heavy chain, the hereditary multisystem disorder. myosin regulatory and essential light chains, myosin bind- N Sensorineural hearing loss is genetically heteroge- ing protein C, troponin I, troponin C, a cardiac actin, and neous. Mutations in the MYO6 gene, encoding 23 titin. The FHC phenotype is characterised by hypertrophy, unconventional myosin VI, have been found to cause myocyte disarray and fibrosis, and results from the dominant non-syndromic sensorineural hearing loss—that is, negative expression of one of these (mainly missense) sensorineural hearing loss in the absence of any other mutations. The resulting sarcomeric dysfunction leads related clinical features. ultimately, through mechanisms that remain obscure, to pathological left ventricular remodelling. -

Clinical Genetics and the Hutterite Brethren
Clinical Genetics and the Hutterite Brethren: What have we learned in the new millenium? Or: A Micheil Innes MD FRCPC FCCMG Adapted from: Medical Genetics Grand Rounds January 2013 History and Population Hutterite Population Today >40 000 in AB, 30000 MB, ND, SD 1593-1770 1874-1879 25000 Transylvania 1256 migrated to American Prairies 20000 15000 World War I 10000 1565-1592 1770 - 1870 Migration to Canada Moravia5000 Ukraine 0 1500s 1520 1540 1550 1570 1580 1590 1610 1620 1680 1750 1760 1840 1860 1890 1900 1950 1975 1990 Tyrolean Alps Why Identify Genes in this Population? • Direct Benefits to • Benefit to Larger Patients/Families population – Non-invasive – Most of these disorders diagnostic test are not confined to this – Carrier test (*marriage population restrictions) – May allow for diagnosis – ?Prenatal testing of atypical cases – Enhanced understanding of – Expand basic science disease may facilitate and clinical knowledge management or treatment Initial Presentations May be Non-Specific Highlighting Importance of Careful Syndrome Delineation and Early Genetic Diagnosis • Hearing Loss – Autosomal recessive non-syndromic hearing loss (> 2loci) – Usher syndrome (> 2loci) – HDR syndrome • Cerebellar Ataxia – Joubert syndrome – DES syndrome – DCMA syndrome – CASS syndrome • Muscular Dystrophy/ High CK – LGMD2H – LGDM2I – AR EDMD – Myopathy with CPEO – Microcephaly with Chorea Genetic services and the Hutterites Religion/Culture • Has posed little barrier overall • Very accepting of medical care and technology • Although they believe that God plays a day to day role in guiding their lives, most couples accept genetic explanations for their children’s disorders • Some leuts and individual colonies are more conservative than others • Colony leader is clearly the Minister • Who speaks for the overall community when it comes to community wide issues? – e.g. -

Hmms Representing All Proteins of Known Structure. SCOP Sequence Searches, Alignments and Genome Assignments Julian Gough* and Cyrus Chothia
268–272 Nucleic Acids Research, 2002, Vol. 30, No. 1 © 2002 Oxford University Press SUPERFAMILY: HMMs representing all proteins of known structure. SCOP sequence searches, alignments and genome assignments Julian Gough* and Cyrus Chothia MRC Laboratory of Molecular Biology, Hills Road, Cambridge CB2 2QH, UK Received September 28, 2001; Revised and Accepted October 30, 2001 ABSTRACT (currently 59) covering approximately half of the The SUPERFAMILY database contains a library of soluble protein domains. The assignments, super- family breakdown and statistics on them are available hidden Markov models representing all proteins of from the server. The database is currently used by known structure. The database is based on the SCOP this group and others for genome annotation, structural ‘superfamily’ level of protein domain classification genomics, gene prediction and domain-based genomic which groups together the most distantly related studies. proteins which have a common evolutionary ancestor. There is a public server at http://supfam.org which provides three services: sequence searching, INTRODUCTION multiple alignments to sequences of known structure, The SUPERFAMILY database is based on the SCOP (1) and structural assignments to all complete genomes. classification of protein domains. SCOP is a structural domain- Given an amino acid or nucleotide query sequence based heirarchical classification with several levels including the server will return the domain architecture and the ‘superfamily’ level. Proteins grouped together at the super- SCOP classification. The server produces alignments family level are defined as having structural, functional and sequence evidence for a common evolutionary ancestor. It is at of the query sequences with sequences of known this level, as the name suggests, that SUPERFAMILY operates structure, and includes multiple alignments of because it is the level with the most distantly related protein genome and PDB sequences. -

Splicing-Correcting Therapeutic Approaches for Retinal Dystrophies: Where Endogenous Gene Regulation and Specificity Matter
New Developments Splicing-Correcting Therapeutic Approaches for Retinal Dystrophies: Where Endogenous Gene Regulation and Specificity Matter Niccolo` Bacchi,1 Simona Casarosa,1,2 and Michela A. Denti1,3 1Centre for Integrative Biology (CIBIO) - University of Trento, Trento, Italy 2Neuroscience Institute - National Research Council (CNR), Pisa, Italy 3Neuroscience Institute - National Research Council (CNR), Padova, Italy Correspondence: Simona Casarosa, Splicing is an important and highly regulated step in gene expression. The ability to modulate Centre for Integrative Biology it can offer a therapeutic option for many genetic disorders. Antisense-mediated splicing- (CIBIO) - University of Trento, Via correction approaches have recently been successfully exploited for some genetic diseases, Sommarive 9, 38123 Trento, Italy; and are currently demonstrating safety and efficacy in different clinical trials. Their [email protected]. application for the treatment of retinal dystrophies could potentially solve a vast panel of Michela A. Denti, Centre for Inte- grative Biology (CIBIO) - University cases, as illustrated by the abundance of mutations that could be targeted and the versatility of ofTrento,ViaSommarive9,38123 the technique. In this review, we will give an insight of the different therapeutic strategies, Trento, Italy; focusing on the current status of their application for retinal dystrophies. [email protected]. Keywords: splicing correction, antisense oligonucleotides, retinal dystrophy, gene therapy SC and MAD contributed equally to the work presented here and should therefore be regarded as equivalent authors. Submitted: April 8, 2014 Accepted: April 11, 2014 Citation: Bacchi N, Casarosa S, Denti MA. Splicing-correcting therapeutic approaches for retinal dystrophies: where endogenous gene regulation and specificity matter. Invest Oph- thalmol Vis Sci. -

AUTOPHY by Deepika Prasad a Thesis
ANALYZING MARKER GENE DIVERSITY USING AN AUTOMATED PHYLOGENETIC TOOL: AUTOPHY by Deepika Prasad A thesis submitted to the Faculty of the University of Delaware in partial fulfillment of the requirements for the degree of Master of Science in Bioinformatics and Computational Biology Spring 2017 © 2017 Deepika Prasad All Rights Reserved ANALYZING MARKER GENE DIVERSITY USING AN AUTOMATED PHYLOGENETIC TOOL: AUTOPHY by Deepika Prasad Approved: __________________________________________________________ Shawn Polson, Ph.D. Professor in charge of thesis on behalf of the Advisory Committee Approved: __________________________________________________________ Kathleen F.McCoy, Ph.D. Chair of the Department of Computer and Information Sciences Approved: __________________________________________________________ Babatunde A. Ogunnaike, Ph.D. Dean of the College of Engineering Approved: __________________________________________________________ Ann L. Ardis, Ph.D. Senior Vice Provost for Graduate and Professional Education ACKNOWLEDGMENTS I want to express my sincerest gratitude to Professor Shawn Polson for his patience, continuous support, and enthusiasm. I could not have imagined having a better mentor to guide me through the process of my Master’s thesis. I would like to thank my committee members, Professor Eric Wommack and Honzhan Huang for their insightful comments and guidance in the thesis. I would also like to express my gratitude to Barbra Ferrell for asking important questions throughout my thesis research and helping me with the writing process. I would like to thank my friend Sagar Doshi, and lab mates Daniel Nasko, and Prasanna Joglekar, for helping me out with data, presentations, and giving important advice, whenever necessary. Last but not the least, I would like to thank my family, for being my pillars of strength. -

Cardiomyopathy Precision Panel Overview Indications
Cardiomyopathy Precision Panel Overview Cardiomyopathies are a group of conditions with a strong genetic background that structurally hinder the heart to pump out blood to the rest of the body due to weakness in the heart muscles. These diseases affect individuals of all ages and can lead to heart failure and sudden cardiac death. If there is a family history of cardiomyopathy it is strongly recommended to undergo genetic testing to be aware of the family risk, personal risk, and treatment options. Most types of cardiomyopathies are inherited in a dominant manner, which means that one altered copy of the gene is enough for the disease to present in an individual. The symptoms of cardiomyopathy are variable, and these diseases can present in different ways. There are 5 types of cardiomyopathies, the most common being hypertrophic cardiomyopathy: 1. Hypertrophic cardiomyopathy (HCM) 2. Dilated cardiomyopathy (DCM) 3. Restrictive cardiomyopathy (RCM) 4. Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) 5. Isolated Left Ventricular Non-Compaction Cardiomyopathy (LVNC). The Igenomix Cardiomyopathy Precision Panel serves as a diagnostic and tool ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes. Indications The Igenomix Cardiomyopathy Precision Panel is indicated in those cases where there is a clinical suspicion of cardiomyopathy with or without the following manifestations: - Shortness of breath - Fatigue - Arrythmia (abnormal heart rhythm) - Family history of arrhythmia - Abnormal scans - Ventricular tachycardia - Ventricular fibrillation - Chest Pain - Dizziness - Sudden cardiac death in the family 1 Clinical Utility The clinical utility of this panel is: - The genetic and molecular diagnosis for an accurate clinical diagnosis of a patient with personal or family history of cardiomyopathy, channelopathy or sudden cardiac death. -

WES Gene Package Multiple Congenital Anomalie.Xlsx
Whole Exome Sequencing Gene package Multiple congenital anomalie, version 5, 1‐2‐2018 Technical information DNA was enriched using Agilent SureSelect Clinical Research Exome V2 capture and paired‐end sequenced on the Illumina platform (outsourced). The aim is to obtain 8.1 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA‐MEM algorithm (reference: http://bio‐bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x A4GALT [Blood group, P1Pk system, P(2) phenotype], 111400 607922 101 100 100 99 [Blood group, P1Pk system, p phenotype], 111400 NOR polyagglutination syndrome, 111400 AAAS Achalasia‐addisonianism‐alacrimia syndrome, 231550 605378 73 100 100 100 AAGAB Keratoderma, palmoplantar, -

Accounts of Chemical Research 8 (1975) - 21, 22 {1-11}, 23 - 30 (1997)
A Accounts of Chemical Research 8 (1975) - 21, 22 {1-11}, 23 - 30 (1997) Acta Chemica Scandinavica 1 (1947) - 27 (1973) : Acta Chemica Scandinavica. 1974 - 1988 : Ser. Aと Ser. B . に分離 A 28 (1974) - A 42 (1988) : Ser. A : Physical and Inorganic Chemistry B 28 (1974) - B 42 (1988) : Ser. B : Organic Chemistry and Biochemistry 43 (1989) : 合併 Acta Chemica Scandinavica. 1 (1947) - 51 (1997) Acta Phytotaxonomica et Geobotanica →APG * Advances in Analytical Chemistry and Instrumentation 1 (1960) - 11 (1973) * Advances in Biological and Medical Physics 10 (1965) - 17 (1980) * Advances in Carbohydrate Chemistry → Advances in Carbohydrate Chemistry and Biochemistry * Advances in Carbohydrate Chemistry and Biochemistry 1 (1945) - 23 (1968) : Advances in Carbohydrate Chemistry 1 (1945) - 61 (2007) 62 (2008) + : 電子ジャーナル * Advances in Catalysis 1 (1948) - 21 (1970) : Advances in Catalysis and Related Subjects 1 (1948) - 41 (1996) * Advances in Catalysis and Related Subjects → Advances in Catalysis * Advances in Chemical Engineering 1 (1956) - 23 (1996) * Advances in Chemical Physics 1 (1958) - 58, 60 - 93, 95 - 96 (1996) * Advances in Clinical Chemistry 1 (1958) - 31 (1994) * Advances in Drug Research 1 (1964) - 12 (1977) * Advances in Electrochemistry and Electrochemical Engineering 1 1 (1961) - 13 (1984) * Advances in Enzyme Regulation 1 (1963) - 33 (1993) * Advances in Enzymology * Advances in Enzymology and Related Subjects * Advances in Enzymology and Related Subjects of Biochemistry → Advances in Enzymology and Related Areas of Molecular Biology -
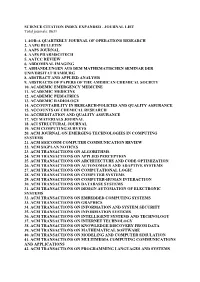
SCIENCE CITATION INDEX EXPANDED - JOURNAL LIST Total Journals: 8631
SCIENCE CITATION INDEX EXPANDED - JOURNAL LIST Total journals: 8631 1. 4OR-A QUARTERLY JOURNAL OF OPERATIONS RESEARCH 2. AAPG BULLETIN 3. AAPS JOURNAL 4. AAPS PHARMSCITECH 5. AATCC REVIEW 6. ABDOMINAL IMAGING 7. ABHANDLUNGEN AUS DEM MATHEMATISCHEN SEMINAR DER UNIVERSITAT HAMBURG 8. ABSTRACT AND APPLIED ANALYSIS 9. ABSTRACTS OF PAPERS OF THE AMERICAN CHEMICAL SOCIETY 10. ACADEMIC EMERGENCY MEDICINE 11. ACADEMIC MEDICINE 12. ACADEMIC PEDIATRICS 13. ACADEMIC RADIOLOGY 14. ACCOUNTABILITY IN RESEARCH-POLICIES AND QUALITY ASSURANCE 15. ACCOUNTS OF CHEMICAL RESEARCH 16. ACCREDITATION AND QUALITY ASSURANCE 17. ACI MATERIALS JOURNAL 18. ACI STRUCTURAL JOURNAL 19. ACM COMPUTING SURVEYS 20. ACM JOURNAL ON EMERGING TECHNOLOGIES IN COMPUTING SYSTEMS 21. ACM SIGCOMM COMPUTER COMMUNICATION REVIEW 22. ACM SIGPLAN NOTICES 23. ACM TRANSACTIONS ON ALGORITHMS 24. ACM TRANSACTIONS ON APPLIED PERCEPTION 25. ACM TRANSACTIONS ON ARCHITECTURE AND CODE OPTIMIZATION 26. ACM TRANSACTIONS ON AUTONOMOUS AND ADAPTIVE SYSTEMS 27. ACM TRANSACTIONS ON COMPUTATIONAL LOGIC 28. ACM TRANSACTIONS ON COMPUTER SYSTEMS 29. ACM TRANSACTIONS ON COMPUTER-HUMAN INTERACTION 30. ACM TRANSACTIONS ON DATABASE SYSTEMS 31. ACM TRANSACTIONS ON DESIGN AUTOMATION OF ELECTRONIC SYSTEMS 32. ACM TRANSACTIONS ON EMBEDDED COMPUTING SYSTEMS 33. ACM TRANSACTIONS ON GRAPHICS 34. ACM TRANSACTIONS ON INFORMATION AND SYSTEM SECURITY 35. ACM TRANSACTIONS ON INFORMATION SYSTEMS 36. ACM TRANSACTIONS ON INTELLIGENT SYSTEMS AND TECHNOLOGY 37. ACM TRANSACTIONS ON INTERNET TECHNOLOGY 38. ACM TRANSACTIONS ON KNOWLEDGE DISCOVERY FROM DATA 39. ACM TRANSACTIONS ON MATHEMATICAL SOFTWARE 40. ACM TRANSACTIONS ON MODELING AND COMPUTER SIMULATION 41. ACM TRANSACTIONS ON MULTIMEDIA COMPUTING COMMUNICATIONS AND APPLICATIONS 42. ACM TRANSACTIONS ON PROGRAMMING LANGUAGES AND SYSTEMS 43. ACM TRANSACTIONS ON RECONFIGURABLE TECHNOLOGY AND SYSTEMS 44. -

Clinical Exome Sequencing for Genetic Identification of Rare Mendelian Disorders
Supplementary Online Content Lee H, Deignan JL, Dorrani N, Strom SP, Kantarci S, Quintero-Rivera F, et al. Clinical exome sequencing for genetic identification of rare Mendelian disorders. JAMA. doi:10.1001/jama.2014.14604. eMethods 1. Sample acquisition and pre-test sample processing eMethods 2. Exome capture and sequencing eMethods 3. Sequence data analysis eMethods 4. Variant filtration and interpretation eMethods 5. Determination of variant pathogenicity eFigure 1. UCLA Clinical Exome Sequencing (CES) workflow eFigure 2. Variant filtration workflow starting with ~21K variants across the exome and comparing the mean number of variants observed from trio-CES versus proband-CES eFigure 3. Variant classification workflow for the variants found within the primary genelist (PGL) eTable 1. Metrics used to determine the adequate quality of the sequencing test for each sample eTable 2. List of molecular diagnoses made eTable 3. List of copy number variants (CNVs) and uniparental disomy (UPD) reported and confirmatory status eTable 4. Demographic summary of 814 cases eTable 5. Molecular Diagnosis Rate of Phenotypic Subgroups by Age Group for Other Clinical Exome Sequencing References © 2014 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 10/01/2021 This supplementary material has been provided by the authors to give readers additional information about their work. © 2014 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 10/01/2021 eMethods 1. Sample acquisition and pre-test sample processing. Once determined by the ordering physician that the patient's presentation is clinically appropriate for CES, patients were offered the test after a counseling session ("pre-test counseling") [eFigure 1].